Background
Reported rates of gluteal pain after sacrospinous ligament fixation range from 12–55% in the immediate postoperative period and from 4–15% 4–6 weeks postoperatively. The source of gluteal pain often is attributed to injury to the nerve to levator ani or pudendal nerve. The inferior gluteal nerve and other sacral nerve branches have not been examined thoroughly as potential sources of gluteal pain.
Objectives
The purpose of this study was to further characterize anatomy of the inferior gluteal nerve and other nerves that are associated with the sacrospinous ligament from a combined gluteal and pelvic approach and to correlate findings to sacrospinous ligament fixation.
Study Design
Dissections were performed in female cadavers that had not been embalmed with gluteal and pelvic approaches. From a pelvic perspective, the closest structure to the superior border of the sacrospinous ligament midpoint was noted, and the sacral nerves that perforated the ventral surface of coccygeus muscle were examined. From a gluteal perspective, the closest distances from ischial spine to the pudendal, inferior gluteal, posterior femoral cutaneous, and sciatic nerves were measured. In addition, the closest distance from the midpoint of sacrospinous ligament to the inferior gluteal nerve and the origin of this nerve were documented. The thickness and height of the sacrospinous ligament at its midpoint were measured. Sacral nerve branches that coursed between the sacrospinous and sacrotuberous ligaments were assessed from both a pelvic and a gluteal approach. Descriptive statistics were used for data analysis.
Results
Fourteen cadavers were examined. From a pelvic perspective, the closest structure to the superior border of sacrospinous ligament at its midpoint was the S3 nerve (median distance, 3 mm; range, 0–11 mm). Branches from S3 and/or S4 perforated the ventral surface of coccygeus muscles in 94% specimens. From a gluteal perspective, the closest structure to ischial spine was the pudendal nerve (median distance, 0 mm; range, 0–9 mm). Median closest distance from inferior gluteal nerve to ischial spine and to the midpoint of sacrospinous ligament was 28.5 mm (range, 6–53 mm) and 31.5 mm (range, 10–47 mm), respectively. The inferior gluteal nerve arose from dorsal surface of combined lumbosacral trunk and S1 nerves in all specimens; a contribution from S2 was noted in 46% of hemipelvises. At its midpoint, the sacrospinous ligament median thickness was 5 mm (range, 2–7 mm), and its median height was 14 mm (range, 3–22 mm). In 85% of specimens, 1 to 3 branches from S3 and/or S4 nerves pierced or coursed ventral to the sacrotuberous ligament and perforated the inferior portion of the gluteus maximus muscle.
Conclusions
Damage to the inferior gluteal nerve during sacrospinous ligament fixation is an unlikely source for postoperative gluteal pain. Rather, branches from S3 and/or S4 that innervate the coccygeus muscles and those coursing between the sacrospinous and sacrotuberous ligaments to supply gluteus maximus muscles are more likely to be implicated. A thorough understanding of the complex anatomy surrounding the sacrospinous ligament, limiting depth of needle penetration into the ligament, and avoiding extension of needle exit or entry point above the upper extent of sacrospinous ligament may reduce nerve entrapment and postoperative gluteal pain.
Gluteal pain after sacrospinous ligament fixation (SSLF) procedures has been reported in up to 55% of patients in the immediate postoperative period. Fixation of the vaginal vault to the sacrospinous ligament (SSL) was introduced in the United States by Randall and Nichols in 1971 and has remained a mainstay in the surgical treatment of vaginal vault prolapse. Reported rates of serious adverse events that are associated with SSLF are low and similar to comparable vaginal prolapse repair procedures, such as the uterosacral ligament suspension. In a recent randomized trial that compared outcomes of SSLF and uterosacral ligament suspension, the rates of gluteal or posterior thigh pain that persisted 4–6 weeks postoperatively were higher in the SSLF group (4%) compared with the uterosacral ligament suspension group (0.5%).
As previously described, “the SSL consists of dense connective tissue that attaches to the ischial spine laterally and to the lower part of the sacrum and coccyx medially. The SSL, along with the sacrotuberous ligament (STL), divides the sciatic notches of the ischium and ilium into the lesser and greater sciatic foramen (GSF), respectively. The internal pudendal and inferior gluteal vessels, pudendal and sciatic nerves, and other branches of the sacral nerve plexus pass through the GSF in close proximity to the ischial spine and SSL. The coccygeus muscle lies on the ventral or pelvic surface of the SSL and together with the levator ani muscles comprises the pelvic diaphragm. The coccygeus muscle has the same bony attachments and runs an identical course to the SSL.” The muscle and the ligament are connected closely and separable only by vigorous dissection; thus, many refer to these structures as the coccygeus–SSL (C-SSL) complex. Because of this relationship, needle entry into the SSL requires passage through the coccygeus muscle and overlying layer of fascia.
Suture placement into the SSL can be achieved with various ligature carriers, such as the Deschamps, Capio, Miya hook or a Mayo needle and straight needle driver. Various rates of gluteal or thigh pain have been reported with the use of different devices. For example, 55.4% gluteal or thigh pain was noted in the immediate postoperative period in a retrospective study of women who underwent SSLF in which the Capio device was used. In this study, pain persisted in 15.4% of patients at 6 weeks follow up. Another retrospective review compared 3 different techniques for suture placement (Deschamps, Miya hook, and standard needle driver) showed an 18% rate of nerve injury with the use of Deschamps; no nerve injuries were reported with the use of the Miya hook or the standard needle driver. These striking differences in the rates of gluteal or thigh pain with the use of different devices may be explained by depth of needle penetration into the SSL, number of ligament punctures, extent of ligament spanned, and surgeon experience with a specific device.
The neuroanatomy that is associated with the SSL has been described mainly from a transabdominal or pelvic approach. These studies have emphasized the relationship of the pudendal nerve and vessels and that of the nerve to levator ani to the C-SSL complex. The inferior gluteal nerve (IGN) exits the pelvis between the piriformis muscle and C-SSL complex and supplies the gluteus maximus muscle and overlying skin. Thus, injury to this nerve may lead to gluteal pain after SSLF. However, the course and anatomic relationships of the IGN has not been examined thoroughly. The objectives of this study were to further characterize the anatomy of the IGN and other nerves that are associated with the SSL from a combined gluteal and pelvic approach and to correlate findings to SSLF.
Materials and Methods
Detailed dissections were performed in female cadavers that had not been embalmed that were obtained from the Willed Body Program at the University of Texas Southwestern Medical Center in Dallas, TX. This study was considered exempt from review by the University of Texas Southwestern Medical Center Institutional Review Board in accordance with the Code of Federal Regulations, Title 45. Age, race, height, weight, and cause of death were available for all donated bodies.
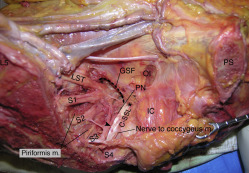
Cadavers were transected above the level of aortic bifurcation, at mid thigh, and in the midsagittal plane to facilitate exposure. Dissections were first performed from a pelvic approach before midsagittal transection ( Figure 1 ). The peritoneum overlying the iliac vessels and the fascia that covers the piriformis muscles was resected to expose the lumbosacral trunk (L4, L5), first through fourth sacral nerves (S1–S4), and the inferior gluteal and internal pudendal arteries. These vessels were tagged with sutures for later identification during gluteal dissections. The visceral branches of the internal iliac artery and internal iliac veins were removed to expose the ventral surface of the coccygeus muscle and its superior fascial layer. Sacral nerve branches that perforated the coccygeus muscle were dissected carefully, and their origin was documented. The tip of the ischial spine was identified and marked with a metal pin. Dissections were then continued through a gluteal approach. The skin and subcutaneous tissue overlying the gluteus maximus muscles and posterior thigh were removed sharply starting at the midline of the sacrum. The gluteus maximus was then cut from its attachments at the sacrum and iliac crest and carefully reflected laterally to preserve the inferior gluteal neurovascular bundle. Once identified, the inferior gluteal artery and nerve were tagged with sutures. The dorsal surface of STL was exposed between the lateral sacrum and ischial tuberosity, and neurovascular structures that were noted in proximity to the ligament were dissected carefully. The STL was then transected in its midpoint, perpendicular to its long axis, and the pudendal neurovascular bundle was identified on the dorsal surface of the SSL. The length of the SSL was measured from the tip of the ischial spine to the ligament attachment on the lateral and lower aspect of the sacrum, and a metal pin was placed at the ligament’s midpoint. The transected edges of the STL were reflected, and the point at which the sacrotuberous and SSLs fused was identified. The distance from the ischial spine to this fusion point was measured. Other structures that exited the pelvis through the GSF were then identified. These included the piriformis muscle and the sciatic and posterior femoral cutaneous nerves.
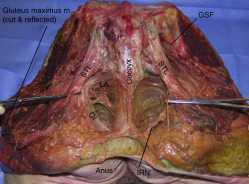
From a gluteal perspective, the closest distances from the tip of the ischial spine to the pudendal, inferior gluteal, posterior femoral cutaneous, and sciatic nerves were measured. In addition, the closest distance from the midpoint of SSL to the IGN and the origin of this nerve were documented. The width of these nerves and that of the piriformis muscles in the midgluteal region were also documented. Last, the ventral to dorsal (thickness) and superior to inferior (height) extents of the C-SSL complex at its midpoint were measured. From a pelvic perspective, the closest structure to the superior border of the SSL midpoint and the origin of sacral nerves that perforated the ventral surface of the coccygeus muscle were documented. Sacral nerve branches that coursed between the sacrospinous and STLs were examined from both the gluteal and pelvic approaches, and their origin and termination was documented.
All measurements were taken twice by the same examiner who used the same caliper and 10-cm plastic ruler. Photographs of all dissections were taken, and descriptive statistics were used for data analysis and reporting.
Results
Fourteen female cadavers that had not been embalmed were examined. All cadavers were white, with median age of 74.5 years (range, 59–94 years). The median body mass index was 20 kg/m 2 (range, 13–30 kg/m 2 ). The most common cause of death was lung disease. Dissections and available medical histories revealed no evidence of previous pelvic surgery or pelvic disease such as cancer, fractured pelvic bones, or trauma.
Pelvic approach
In 50% of specimens, the closest structure to the superior border of SSL at its midpoint was the S3 nerve, with a median distance of 3 mm (range, 0–11 mm; Figure 2 ). In the remaining specimens, the pudendal nerve (35%) or S4 (15%) were the closest structures. Branches from S3 and/or S4 were noted to perforate the ventral surface of the coccygeus muscles in 94% of specimens. An S5 nerve, 1–2 mm wide, was identified coursing beneath the coccygeus fascia in 43% of hemipelvises. When identified, it joined the S4 nerve close to the fourth sacral foramen and contributed to coccygeus muscle innervation.
Gluteal approach
The closest distances from the ischial spine to the pudendal, inferior gluteal, posterior femoral cutaneous, and sciatic nerves and the widths of these nerves in the midgluteal region are presented in the Table . In 82% of cadavers, the closest structure to the tip of the ischial spine was the pudendal nerve (median distance, 0 mm; range 0–8 mm). In all specimens, this nerve coursed medial to the ischial spine ( Figure 3 ). In remaining 18% of specimens, the internal pudendal artery was the closest structure to the ischial spine (median distance, 4 mm; range, 0–8 mm). The median distance from the midpoint of SSL to IGN was 31.5 mm (range, 10–47 mm). The closest median distance from the inferior gluteal artery to ischial spine was 19 mm (range, 4–33 mm). The IGN arose from the dorsal surface of the combined lumbosacral trunk and S1 nerves in all specimens; a contribution from S2 was noted in 46% of hemipelvises.



