Incision and Drainage of a Dental Abscess
Elliott M. Harris
Introduction
A dental abscess is an area of localized infection involving the structures surrounding the teeth. Often this becomes a fluctuant swelling that requires drainage to promote healing. Usually dental abscesses are seen in older children and are more likely to involve the permanent dentition. However, abscesses may be seen in younger patients with poor oral hygiene and carious teeth (1). Although the vast majority of cases are managed by a dentist or an oral surgeon, the emergency physician is occasionally called upon to perform incision and drainage for patients with simple abscesses when referral is delayed. Emergency care will help speed the recovery process and provide some relief from pain. Further dental care will normally be needed once the infectious process subsides.
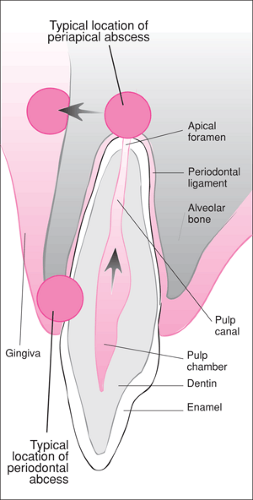
The most common types of dental abscesses include periapical and periodontal abscesses. The periapical abscess is by far the most common dental abscess in children and results from spread of infection or inflammation from the pulp to the periapical tissues via the apical foramen of the tooth (1). Periodontal abscesses, which involve the periodontal structures (such as the gingivae or periodontal ligament), are more common in adults and are usually a complication of periodontal disease. When seen in children, periodontal abscesses are most often the result of a foreign body introduced into previously healthy periodontal tissue (1).
Anatomy and Physiology
The most common predisposing factor to formation of a dental abscess in children is the presence of caries. Once the carious process has extended through the hard structures of the tooth (the enamel and the dentin) and into the pulp cavity (Fig. 63.1), pulpal infection and/or inflammation occur. This process usually results in pulp necrosis. The inflammatory process then extends to the periapical tissues via the apical foramen, leading to the formation of a periapical abscess. Although caries are the most common predisposing factor, any process that causes or predisposes to pulp necrosis (e.g., trauma, recent dental procedures) may lead to abscess formation (2,3,4).
Primary teeth have thinner enamel than permanent teeth, and therefore the pulp of the primary dentition has relatively less protection. In addition, because of a more abundant blood supply, the pulp of primary teeth tends to have a greater inflammatory response to injury. One advantage primary teeth have is that they are better at forming dentin beneath carious lesions. This provides some extra protection for the pulp in the face of the poor oral hygiene practiced by many children.
As mentioned previously, periodontal abscesses in children, unlike in adults, are not associated with periodontal disease. Often a cause cannot be elucidated, but frequently they are due to impaction of a foreign body in the periodontal tissues. In contrast to periapical abscesses, periodontal abscesses are associated with vital teeth (1).
Dental abscesses may be found on either side of the gingiva, but lesions are found more frequently on the buccal aspect than on the lingual side. The vast majority (more than 80%) of abscesses are found in the maxillary arch (2). Such infections can be complicated by the spread of infection through the soft-tissue planes of the head and neck via paths of least resistance. Infection of the orbit, maxillary sinuses, infratemporal fossa, and sublingual and submandibular regions may result from untreated dental abscesses. Chronically draining fistulas also may occur. The buccinator muscle often serves as a barrier to the spread of infection to other areas of the head and neck. In children (who have a shorter facial height), the apices of
the teeth—especially the permanent first molars, incisors, and canines—lie outside the muscle attachments. This leads to an increased risk of extraoral spread in younger patients (1).
the teeth—especially the permanent first molars, incisors, and canines—lie outside the muscle attachments. This leads to an increased risk of extraoral spread in younger patients (1).
Bacteria in dental abscesses tend to correspond to normal oral flora. Gram-positive cocci and anaerobes are the usual pathologic bacteria. Although Streptococcus viridans tends to predominate in caries, once the pulp chamber is entered, anaerobes become the more frequently cultured offending organisms (3,4). Penicillin is still considered by most to be the drug of choice when antibiotics are required (2,3,4); however, longer standing infections tend to have a higher incidence of penicillin-resistant organisms (4). Clindamycin has become the recommended empiric therapy for those with more chronic presentations or allergy to penicillin (2,4). Erythromycin has fallen out of favor as a second-line agent (2,4). Amoxicillin, although broader in spectrum than penicillin, has not been shown to have any significant advantage except in dosing interval and palatability (4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree