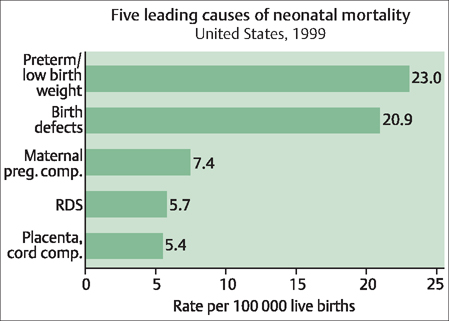
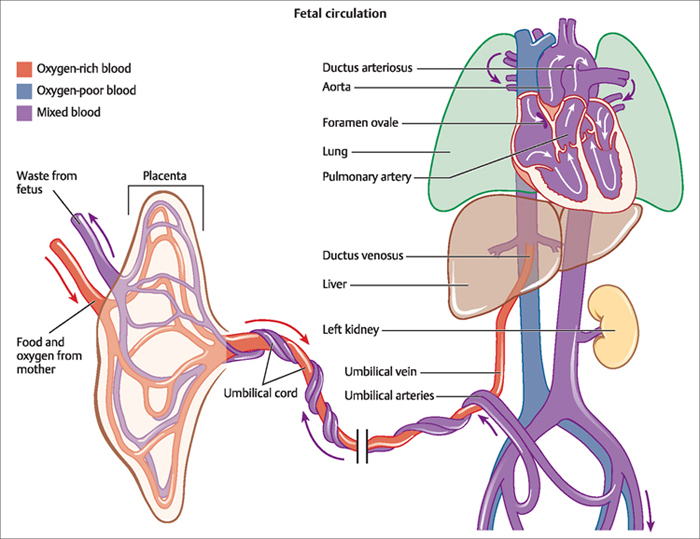
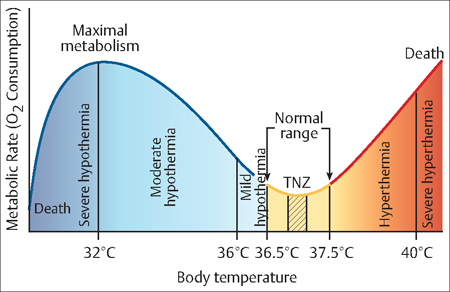
12 Immediate and Postpartum Newborn Care Julieta E. Irman and Gustavo F. Leguizamòn The neonatal period comprises the four weeks following delivery. During this phase, the newborn must rapidly adjust to its extrauterine life. To survive and achieve normal development, it must make major physiologic changes, including increased respiratory gas exchange, switching from fetal to neonatal circulation, and taking over its own thermoregulation. This chapter addresses these major physiologic changes involved in the newborn’s transition to its extrauterine life. It also offers the basics of medical interventions commonly used to assist newborns throughout this critical transition. Apgar score: The Apgar score provides an objective method of evaluating the physical condition of a newborn infant soon after delivery. The score takes into account the heart rate, respiratory effort, muscle tone, skin color, and responce to a catheter in the nostril. Each of these objective signs can receive 0, 1, or 2 points, and each test is performed at 1 minute and 5 minutes after delivery. A common mnemonic is APGAR: Appareance, Pulse, Grimace, Activity and Respiration. Hyperbilirubinemia: This term refers to excess bilirubin in the blood, usually characterized by jaundice or yellowing of the eyes. Hyperthermia: Abnormally high body temperature that occurs when the body’s metabolic heat production or environmental heat load exceeds the normal heat loss capacity (or when heat loss is impaired). Hypothermia: A dangerous lowering of body-core temperature, caused by losing heat faster than it is produced by the body. Postpartum: A term used to describe something that occurs after childbirth, usually involving the mother. Tachypnea: This refers to an excessively rapid respiratory rate, defined as greater than 20 breaths per minute. Transition: The transition period is referred to as 6–12 hours after birth, when the baby goes through physiological adaptation to extrauterine life. Vaginal introitus: This is the anatomical term for the vaginal opening. The alveoli of the fetus in utero are filled with fluid that must be cleared during the initial transitional period, so that the baby can breathe. In addition, to ensure effective pulmonary perfusion and to match perfusion to ventilation, the baby must be able to increase blood flow to the lungs. During the last few weeks of pregnancy, there is a maturation and recruitment of sodium channels in the epithelial cells of the lungs in response to endogenous steroid and catecholamine surges that are triggered by the onset of labor. It is through these epithelial sodium channels that a significant part of the fluid in the fetus’ lungs is purged. Liquid is also driven out of the fetus’ lungs through the pulmonary epithelium into the vasculature as well as through the mechanical squeeze and Starling forces that occur during the process of labor and vaginal delivery. Newborns sometimes have difficulty purging all the liquid from their lungs, particularly if they are late pre-term babies. As a result, they may exhibit respiratory difficulties that require stabilization and immediate supportive therapy, such as supplemental oxygen and assisted ventilation. They are also at increased risk for associated morbidities. Wang et al. estimated that nearly one-third of late preterm newborns exhibit respiratory difficulties. Neonates who are born by cesarean delivery before labor begins are at increased risk for respiratory distress, as are late preterm males compared with late preterm females. Hemodynamic instability caused by hypothermia or hypoglycemia may worsen the newborn’s underlying respiratory distress. Acute respiratory distress syndrome (RDS) is the most common respiratory condition experienced in newborns. The condition, which is characterized by severe difficulty in breathing and related complications, occurs primarily in neonates born between 34 and 36 weeks’ gestation. It is the fourth leading cause of death for neonates in the United States (Fig. 12.1). Late preterm infants also are at increased risk of having low Apgar scores, transient tachypnea of the newborn (TTN), persistent pulmonary hypertension, and respiratory failure. TTN and RDS are both common respiratory conditions in the late preterm newborn and are related to difficulty in clearing fluid from the lungs or a surfactant deficiency, or both. The protocols for managing a child in respiratory distress are covered later in this chapter. As described in Chapter 9, there is a substantial difference between the circulation of a fetus and a neonate. In the womb, well oxygenated blood from the placenta is delivered to the fetus through the umbilical vein. The umbilical vein gives off branches to the left lobe of the liver and then continues as the ductus venosus (Fig. 12.2). The left hepatic vein fuses with the well oxygenated ductus venosus and fows into the inferior vena cava to reach the left atrium by crossing thorough the foramen ovale. Then, via the aorta and carotid circulation, this blood supplies the brain and upper body. The right ventricular output is directed through the ductus arteriosus to the descending aorta. Since the pulmonary vascular resistance is high and the mean pulmonary artery pressures are higher than aortic pressures, the flow is mainly directed toward the ductus arteriosus, leaving the pulmonary circulation with 5–10% of the ventricular output. Finally, fetal blood returns to the placenta through the umbilical arteries. However, when delivery occurs, clamping the umbilical cord provokes a sudden decrease in the amount of neonatal blood draining toward and away from the baby. This leads to a sudden increase pressure in the systemic circulation and a decrease in the right side circulation, reversing the right-to-left shunt and leading to the closure of the ductus arteriosus. Prostaglandins play a pivotal role in maintaining patency of the ductus arteriosus in utero and in its closure during early neonatal life. Fig. 12.1 Respiratory distress syndrome (RDS) is the fourth leading cause of death among neonates in the United States at approximately 6 per 100 000 live births Adapted from the National Center for Health Statistics, 1999 period birth/infant death data; prepared by March of Dimes Perinatal Data Center, 2002 Thermoregulation is a critical physiologic function that is closely related to the transition and survival of the infant. An understanding of transitional events and the physiologic adaptations that must be made is essential in helping the neonate to maintain its thermal stability. This section reviews neonatal thermal regulation, heat loss and gain, and infant thermoregulatory behavior. Measures to ensure thermal stability for the neonate are discussed later in this chapter. Babies are not as adaptable as adults to temperature change. A baby’s body surface is about three times greater than an adult’s, relative to the weight of the body. Babies can lose heat rapidly, as much as four times more quickly than adults. Premature and low birth weight babies usually have little body fat and may be too immature to regulate their own temperature, even in a warm environment. Even full-term and healthy newborns may not be able to maintain their body temperature if the environment is too cold. Fig. 12.2 The fetus receives all the necessary nutrition, oxygen, and life support from the mother’s placenta via the blood vessels in the umbilical cord Waste products and carbon dioxide from the fetus are sent back through the umbilical cord and placenta to the mother’s circulation to be eliminated. When babies are stressed by cold, they use energy and oxygen to generate warmth. If skin temperature drops just one degree from the ideal 36.5 °C (97.7 °F), a baby’s oxygen use can increase by 10%. Keeping babies at optimal temperatures, neither too hot nor too cold, enables them to conserve energy and build up reserves. This is especially important when babies are sick or premature. For optimal thermal stability the baby’s temperature must be kept within the Thermal Neutral Zone (Fig. 12.3). Once stabilized within the Thermal Neutral Zone, the baby’s energy expenditure and oxygen consumption are minimized, promoting optimal growth. Thermoregulation is controlled by the hypothalamus, a region of the central nervous system responsible for certain metabolic process and other activities of the autonomic nervous system. Thermal stimuli from the skin and body’s deep (central) thermal receptors provide information on body temperature to the hypothalamus (Fig. 12.4). It is in the hypothalamus that sensory information describing thermal status throughout the body is processed and compared against the temperature set point. Just like a thermostat, the hypothalamus modifes body heat—and therefore body temperature—by altering metabolism, motor tone and activity, vasomotor activity, and sweating to produce either heat gain or loss. Fig. 12.3 Thermal stability is essential for every baby, especially those with limited metabolic capacity due to illness, prematurity, or low birth weight Research has shown that the Thermal Neutral Zone for preterm babies less than 30 weeks old is less than 0 5 °C.
Definitions
The Respiratory Transition
The Circulatory Transition
The Thermoregulatory Transition
Neonatal Thermoregulation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


