Fig. 11.1
Multiple hyperpigmented macules
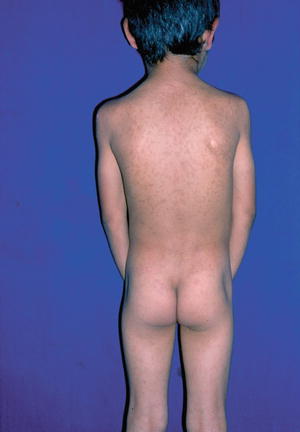
Fig. 11.2
Hyperpigmented macules without erythema
Treatment of IEMP is unnecessary because in most of the cases, spontaneous disappearance of the lesions over several months to years seems to be the rule. The disease does not relapse. An unusual case of a 24-year-old woman with IEMP lasting 21 years characterized by several periods of spontaneous resolution followed by recurrences was reported [9].
At the beginning, tentative diagnoses are usually ashy dermatosis (erythema dyschromicum perstans), fixed drug eruption, or mastocytosis. The diagnosis of IEMP is based on the absence of history of any erythema, and drug medication as well as the absence of Darier’s sign.
Histopathology is seldom justified and the histological picture is not specific. The biopsy of a pigmented spot shows an increased number of melanocytes in the basal-cell layer of the epidermis (Fig. 11.3) and prominent melanophages in the papillary dermis, without visible basal layer damage or lichenoid inflammatory infiltrate (Fig. 11.4). A mild perivascular, lymphocytic, and histiocytic infiltrate may be present. Mast cells are not found. The histopathological study from velvety lesions of nine Indian patients, seven males and two females aged 6–14 years, showed papillomatosis of the dermis with prominent pigmentation of the basal layer (pigmented papillomatosis) without any significant dermal inflammation. Two cases had spores of Pityrosporum ovale in the thickened horny layer, one of which also had bacterial colonies in the stratum corneum [10].
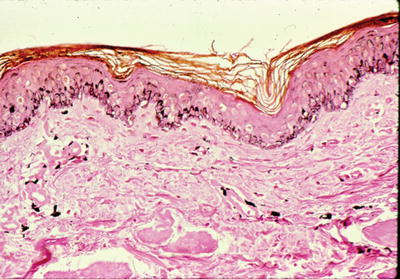
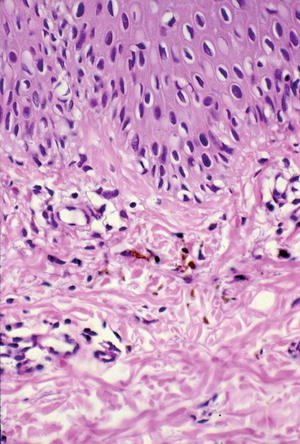
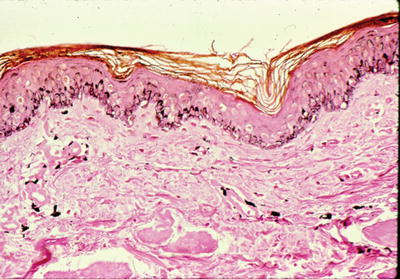
Fig. 11.3
Skin biopsy reveals increased number of melanocytes in the epidermis (silver stain ×10)
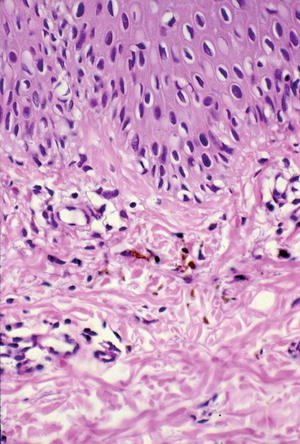
Fig. 11.4
Prominent melanophages in papillary dermis without basal layer damage (H/E × 20)
Electron microscopy shows keratinocytes of the basal and suprabasal layers filled with large numbers of mature and clustered melanosomes. Keratinocytes of all epidermal layers appeared otherwise normal. The number and aspect of melanosomes in melanocytes were normal, as was the overall appearance of melanocytes. In the papillary dermis, macrophages contained large aggregates of melanosomes [7].
Differential diagnosis includes erythema dyschromicum perstans (EDP) or “ashy” dermatosis which was described by Ramirez [11] as a peculiar, slowly progressive, occasionally pruritic ash-colored hyperpigmentation, which leaves a permanent discoloration. It occurs most frequently in Central and South America, mainly in adults, but the condition was reported in 14 Caucasian prepubertal children in Spain by Torrelo et al. [12]. Histologic changes include basal layer vacuolization, apoptotic or cytoid bodies, edema of the dermal papillae, a mild dermal lymphohistiocytic infiltrate, and pigment in dermal macrophages. Peripherally located lichenoid changes can be observed. The authors suggest that EDP is a distinctive clinical entity, different from lichen planus, but may be identical to the so-called idiopathic eruptive macular pigmentation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


