Heel Sticks
Susan Duffy
Dale Steele
Introduction
Capillary blood sampling by means of a heel stick is used to obtain blood for hematologic, biochemical, and blood gas analysis in elective and emergent situations. It is most useful in young infants in whom venous access is difficult or limited. It is a relatively simple procedure that can be performed by physicians, nurses, emergency medical technicians, and other trained personnel.
Anatomy and Physiology
The primary arterial and venous blood supply for the heel skin is located at the junction of the dermis and subcutaneous tissues. In infants, the distance from the surface of the heel to this junction is quite constant at 0.35 to 1.6 mm (1). The distance to the calcaneus from the heel surface increases with infant weight. The mean depth from the skin to the calcaneus is greater in the medial and lateral portions of the heel than in the posterior aspect. Calcaneal depth also increases with growth; however, after 1 year of age, callus formation in the heel precludes using this site (2,4).
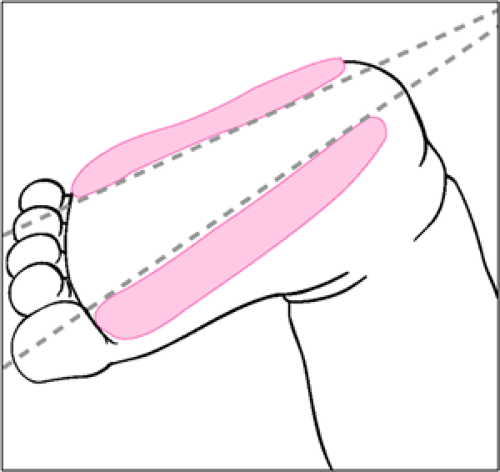
The boundaries of the calcaneus can be located by extending a line posteriorly from between the fourth and fifth toes running parallel to the lateral aspect of the heel and a line extending posteriorly from the middle of the great toe running parallel to the medial portion of the heel. To avoid calcaneal puncture, heel sticks should be performed only in the areas delineated in Figure 40.1.
Indications
Heel puncture samples are useful for most common laboratory studies that require frequent measurement, including hemoglobin, hematocrit, and electrolyte determination. It is most practical in the newborn and especially the premature infant but can be performed in children up to 1 year of age. If hemolysis, venous stasis, or bacterial contamination will interfere with interpretation, samples are better obtained by vascular puncture.
Heel puncture is not recommended when poor peripheral perfusion (e.g., shock) is present. It is not recommended in the setting of compromised blood flow to an extremity, local infection or edema, or significant polycythemia or if there is a need for an accurate measurement of PaO2.
Equipment
Gloves
Warm, wet towel or hot pack
Alcohol swab
Sterile petroleum jelly
Sterile gauze
Detachable capillary blood collector
Collection tubes
Capillary blood gases: heparinized glass capillary tubes
Chemistries: Microtainer tube with serum separator available
Complete blood count: Microtainer tube with heparin or EDTA
Hemoglobin/hematocrit (spun): heparinized glass capillary tube
Capillary cap adapters
Clay pad
Incision device (choose one)
No. 11 surgical blade
Heel lancet device (e.g., Microlance, Minilancet, Microtainer Safety Lance)
Automated disposable incision device (e.g., Tenderfoot, Surgicutt, Nicky, Unistik, Autolet)
The blade and the lancet are subject to variability in operator technique and lack features to control puncture depth. The lancet compresses the dermis and does not allow for free flow of blood. Automated heel stick devices provide consistent penetration depths and standard incisions and allow the collection of increased volumes of blood more quickly and with reduced hemolysis (2).
Procedure
A warm, wet towel is applied to the heel for approximately 5 minutes before the procedure to increase blood flow to the skin surface. The heel is cleansed with alcohol and allowed to dry (alcohol on the skin may lead to erroneously high glucose values) (3). The leg is held in a dependent position while the patient is supine. The heel is held at an 80- to 90-degree angle to the leg. The incision device is then used to puncture the heel perpendicular to the skin on the most medial or lateral portion of the heel, as demonstrated in Figure 40.2A. The posterior curve of the heel should not be punctured, and any previous puncture sites that may be infected should be avoided. The puncture should not exceed 2.5 mm in depth. Milking the heel may activate clotting and cause hemolysis (4,5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree