Background
Women with hypertensive disorders in pregnancy are at an increased risk of cardiovascular disease and type 2 diabetes later in life. Offspring born from these hypertensive pregnancies have increased levels of cardiovascular risk factors; whether they are at an increased risk of type 2 diabetes is not known.
Objective
The objective of the investigation was to study the risk of type 2 diabetes in the adult offspring exposed to maternal preeclampsia or gestational hypertension in utero.
Study Design
We studied 5335 members of the Helsinki Birth Cohort Study, who were born between 1934 and 1944 and who lived in Finland in 1995 when the National Medication Purchase Register was initiated. We ascertained gestational hypertension and preeclampsia according to modern criteria by using maternal and birth records. We defined type 2 diabetes through purchases of antidiabetic medication recorded in the comprehensive National Medication Purchase Register, excluding the 31 subjects who had purchased only insulin. We used Cox regression to assess hazard ratios for type 2 diabetes.
Results
A total of 590 men (21.6%) and 433 women (16.9%) had purchased medication for diabetes. The hazard ratio for type 2 diabetes for offspring exposed to any maternal hypertension in pregnancy was 1.13 (95% confidence interval, 1.00–1.29; n = 1780). For maternal gestational hypertension, it was 1.15 (95% confidence interval, 1.00–1.33; n = 1336) and for preeclampsia 0.98 (95% confidence interval, 0.71–1.34; n = 231). For type 2 diabetes with first medication purchase before 62 years, the corresponding hazard ratios were 1.25 (95% confidence interval, 1.04–1.51); 1.28 (95% confidence interval, 1.05–1.58), and 1.18 (95% confidence interval, 0.75–1.84). The hazard ratios were similar when adjusted for birthweight SD score for gestation, length of gestation, maternal body mass index in late pregnancy, height, age, and parity and for childhood or adult socioeconomic position. An increased risk of type 2 diabetes was also associated with low birthweight SD score, independent of the association with gestational hypertension.
Conclusion
Offspring exposed to maternal gestational hypertension in utero have an increased risk of type 2 diabetes in late adult life. This finding underlines the role of the whole spectrum of hypertensive disorders of pregnancy as risk factors of offspring disease throughout life. It also reinforces previous suggestions that adult health care providers should incorporate birth histories when evaluating an individual’s risk to develop type 2 diabetes.
Hypertensive disorders of pregnancy, including preeclampsia and gestational hypertension, are among the most common pregnancy disorders. Women with these conditions have higher levels of insulin resistance than women with normotensive pregnancy. This difference persists after pregnancy and contributes to a higher risk of type 2 diabetes (T2D) and cardiovascular disease in later life.
Offspring born to these women have also increased levels of cardiovascular risk factors such as higher blood pressure and body mass index and an increased risk of manifest disease including stroke. However, evidence on the offspring risk of diabetes is scanty. Studies on premorbid traits such as glucose metabolism remain inconclusive. Two studies have assessed T2D as an outcome at mean ages of 47 and 45 years in offspring of mothers with preeclampsia. The association with T2D did not reach statistical significance in either study alone or a combined analysis ; neither study assessed other hypertensive disorders of pregnancy.
We used the unique data of the Helsinki Birth Cohort Study, with maternal hypertensive disorders confirmed from pregnancy and birth records using modern criteria, to study their effect on the risk of T2D in offspring born between 1934 and 1944.
Materials and Methods
We studied 6410 singleton members of the Helsinki Birth Cohort Study, born between 1934 and 1944, who had adequate antenatal clinic and birth hospital data to confirm diagnoses of maternal pregnancy disorders by modern criteria as described. The specific criteria are shown in Table 1 . Birthweight SD score, adjusted for gestational age and sex, was based on Finnish standards.
| Variables | Blood pressure | Proteinuria |
|---|---|---|
| Normotension | All systolic measurements <140 mm Hg and diastolic <90 mm Hg | No |
| Gestational hypertension | At least 1 systolic measurement ≥140 mm Hg or diastolic ≥90 mm Hg after 20 wks of gestation, no chronic hypertension | No |
| Nonsevere preeclampsia | At least 1 systolic measurement ≥140 mm Hg or diastolic ≥90 mm Hg after 20 wks of gestation, all systolic measurements <160 mm Hg, and diastolic <110 mm Hg | Yes a |
| Severe preeclampsia | At least 1 systolic measurement ≥160 mm Hg or diastolic ≥110 mm Hg after 20 wks of gestation | Yes a |
| Chronic hypertension or superimposed preeclampsia | At least 1 systolic measurement ≥140 mm Hg or diastolic ≥90 mm Hg before 20 wks of gestation b | Yes/No |
| Any hypertension in pregnancy | Any of the previously cited hypertensive conditions |
a Definition of proteinuria was based on a qualitative measurement, the cutoff of which approximates to 1 mg/mL of albumin
b A total of 816 of the 6410 mothers (12.7%) had blood pressure recordings before 20 weeks’ gestation and could be classified in relation to chronic hypertension/superimposed preeclampsia. Therefore, we do not present chronic hypertension/superimposed preeclampsia as a separate exposure group but include the offspring of these mothers in the any hypertension category.
Of the 6410 cohort members, 5335 lived in Finland in 1995, when the National Medication Reimbursement Database was initiated. Based on this database, we defined T2D as at least 1 purchase of medication for diabetes between 1995 and 2011. Because the early-life origins of type 1 diabetes are likely to be distinct from those of T2D, we excluded the 31 subjects who had purchased only insulin, who are likely to have type 1 diabetes. This left us with 5304 subjects.
Comparisons of these subjects with those who had died or emigrated from Finland before 1995 are shown in Supplemental Table 1 . Those who had died or emigrated were more likely to be men, were born to younger mothers, and had lower and more frequently unknown adult socioeconomic position. There was no difference in the frequency of hypertensive disorders of pregnancy or in childhood socioeconomic position.
The study was approved by the Ethics Committee at Helsinki and Uusimaa Hospital District, and data were linked with permission from the Ministry of Social and Health Affairs, the National Institute for Health and Welfare, and the National Social Insurance Institution. We used Cox regression, stratified for offspring sex and year of birth, to calculate hazard ratios for offspring T2D. Other censoring events were death and migration from Finland, whichever occurred first.
To allow for nonlinear associations with covariates, values of categorical covariates with more than 2 categories (childhood and adulthood socioeconomic position) were contrasted against an indicator category (lowest socioeconomic position). Continuous covariates were first entered as first-, second-, and third-degree polynomials. Because this had virtually no effect on the association between hypertensive pregnancy disorders and offspring T2D, we report the result adjusted for linear effects of the continuous covariates.
Results
Clinical characteristics are shown in Table 2 . A total of 590 men (21.6%) and 433 women (16.9%) had purchased medication for diabetes. The mean age at the first registered purchase was 61.7 years (SD 6.0) for men and 63.0 years (SD 6.0) for women. Because there was no difference in the association between maternal hypertension in pregnancy and T2D between male and female offspring ( P for interaction > .3), we report the results pooled for both sexes, stratified for sex and year of birth.
| Characteristics | Normotensive (n = 3524) | Any hypertension in pregnancy (n = 1780) a | Gestational hypertension (n = 1336) | Preeclampsia, nonsevere (n = 97) | Preeclampsia, severe (n = 134) | Missing |
|---|---|---|---|---|---|---|
| Men | 1836 (52.1%) | 899 (50.5%) | 677 (50.7%) | 54 (55.7%) | 71 (53.0%) | 0 |
| Maternal | ||||||
| Age at delivery, y | 27.9 (5.3) | 28.9 (5.7) | 28.9 (5.8) | 27.8 (4.9) | 29.2 (6.1) | 5 |
| Height | 159.5 (5.6) | 159.7 (5.8) | 159.6 (5.8) | 160.0 (5.8) | 160.2 (5.6) | 266 |
| Body mass index before delivery | 26.0 (2.8) | 26.8 (3.2) | 26.8 (3.2) | 27.0 (3.5) | 26.8 (3.0) | 339 |
| Primiparous | 1731 (49.1%) | 1000 (56.2%) | 731 (54.7%) | 66 (68.0%) | 101 (75.4%) | 0 |
| Birth | ||||||
| Length of gestation, wks | 40.0 (1.6) | 39.9 (1.7) | 40.0 (1.7) | 39.7 (1.9) | 39.3 (2.0) | 285 |
| Birthweight, g | 3430 (467) | 3345 (518) | 3379 (495) | 3227 (514) | 2881 (590) | 0 |
| Birthweight SD score | –0.3 (0.9) | –0.4 (1.1) | –0.4 (1.0) | –0.6 (1.0) | –1.3 (1.1) | 285 |
| Father’s occupational status | 0 | |||||
| Unknown | 211 (6.0%) | 116 (6.5%) | 88 (6.6%) | 6 (6.2%) | 9 (6.7%) | |
| Manual worker | 2385 (67.7%) | 1201 (67.5%) | 903 (67.6%) | 58 (59.8%) | 81 (60.4%) | |
| Lower official | 697 (19.8%) | 339 (19.0%) | 254 (19.0%) | 21 (21.6%) | 31 (23.1%) | |
| Higher official | 231 (6.6%) | 124 (7.0%) | 91 (6.8%) | 12 (12.4%) | 13 (9.7%) | |
| Own adult occupational status | 0 | |||||
| Unknown | 62 (1.8%) | 32 (1.8%) | 25 (1.9%) | 1 (1.1%) | 1 (0.7%) | |
| Manual worker | 1416 (40.2%) | 744 (41.8%) | 563 (42.1%) | 35 (36.1%) | 56 (41.8%) | |
| Self-employed | 330 (9.4%) | 163 (9.2%) | 121 (9.1%) | 10 (10.3%) | 12 (9.0%) | |
| Lower official | 1327 (37.7%) | 662 (37.2%) | 500 (37.4%) | 39 (40.2%) | 46 (34.3%) | |
| Higher official | 389 (11.0%) | 179 (10.1%) | 127 (9.5%) | 12 (12.4%) | 19 (14.2%) | |
| Adult | ||||||
| Ever purchased medication for diabetes, n, % | 660 (18.7%) | 363 (20.4%) | 277 (20.7%) | 17 (17.5%) | 25 (18.7%) | 0 |
| Mean age at first purchase, y | 62.5 (6.1) | 61.7 (6.0) | 61.8 (6.1) | 62.6 (6.2) | 61.4 (6.0) | 0 |
a The number includes in addition 213 mothers with chronic hypertension.
Hypertension in pregnancy and T2D in adult offspring
Offspring of mothers with hypertension in pregnancy had a higher risk of developing T2D in adult life, compared with offspring of normotensive women ( Figure ). The risk was due to an increased risk in offspring of women with gestational hypertension. We then assessed these associations separately among those whose first medication purchase for T2D occurred before and after age 62 years, the approximate mean age of first purchase. We selected this cutoff because the medication purchase register started in 1995, when the subjects were aged 50–61 years. The increased risk of T2D was confined to those with first medication purchase before age 62 years ( Figure ).
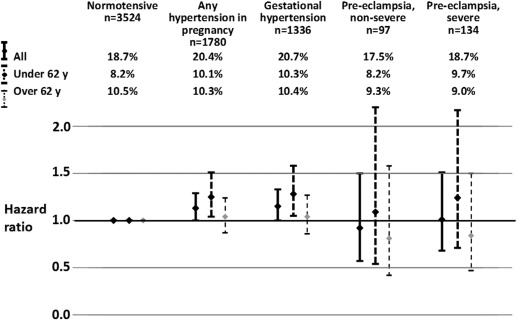
There was no association between the risk of T2D and maternal nonsevere or severe preeclampsia ( Figure ). A post hoc analysis with any maternal preeclampsia combined showed hazard ratios of 0.98 (95% confidence interval [CI], 0.71–1.34) for T2D, 1.18 (95% CI, 0.75–1.84) for onset before and 0.83 (95% CI, 0.53–1.29) after 62 years.
Prenatal factors and socioeconomic status
A 1 SD higher birthweight SD score was associated with a hazard ratio of 0.87 for T2D (95% CI, 0.81–0.93). The risk of T2D was not associated with length of gestation or preterm birth (hazard ratio, 1.18; 95% CI, 0.88–1.58), although the association with preterm birth before 35 weeks of gestation, previously reported in the source cohort, approached statistical significance (hazard ratio, 1.60; 95% CI, 0.94–2.72).
The risk of T2D was also not associated with maternal age, height, body mass index (BMI) before delivery or parity or with childhood socioeconomic position; offspring with lower adult socioeconomic position had higher rates of T2D. Adjustment for these variables had a negligible effect on the association between maternal hypertensive disorders and offspring T2D ( Table 3 ).



