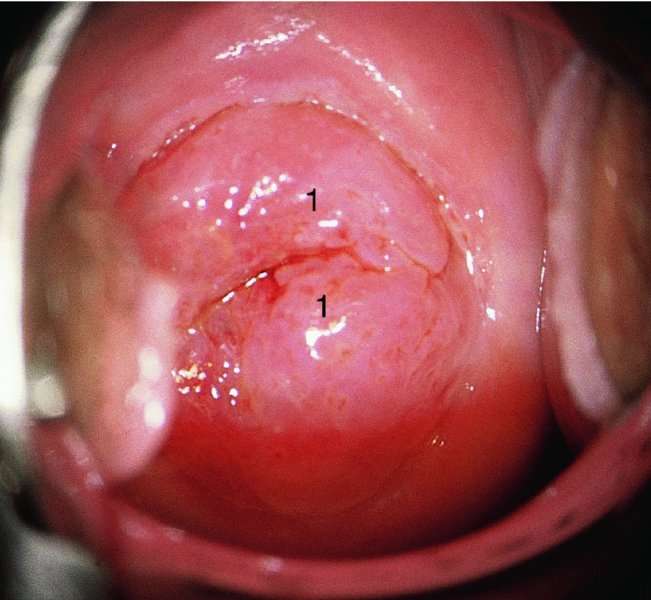
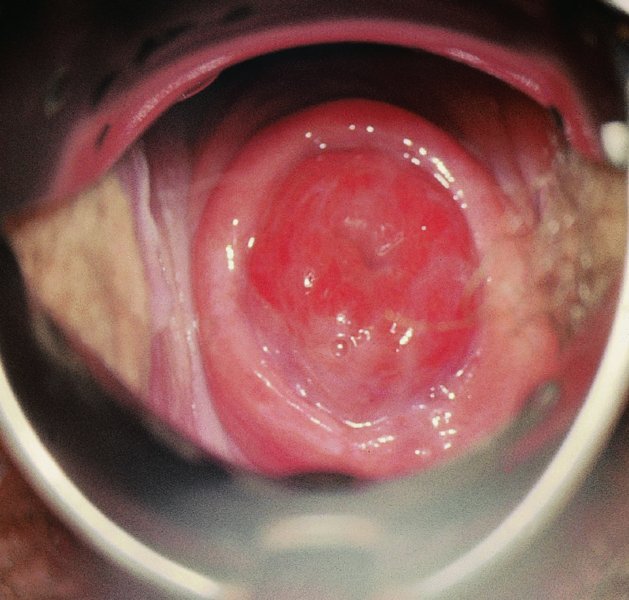
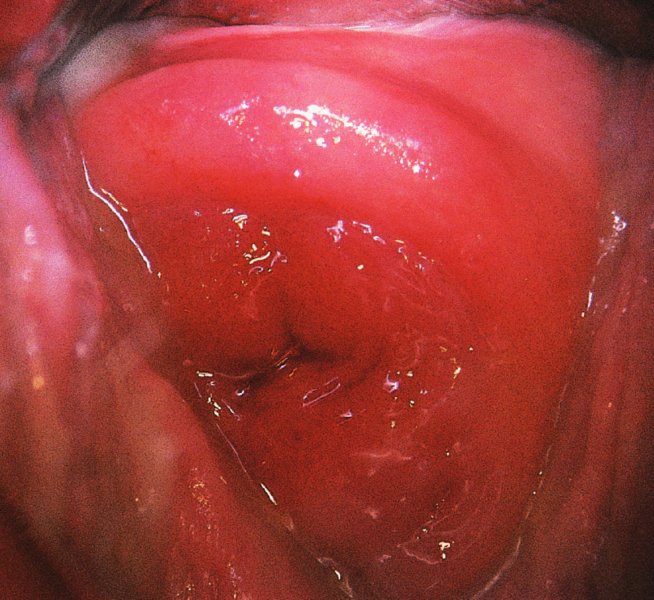
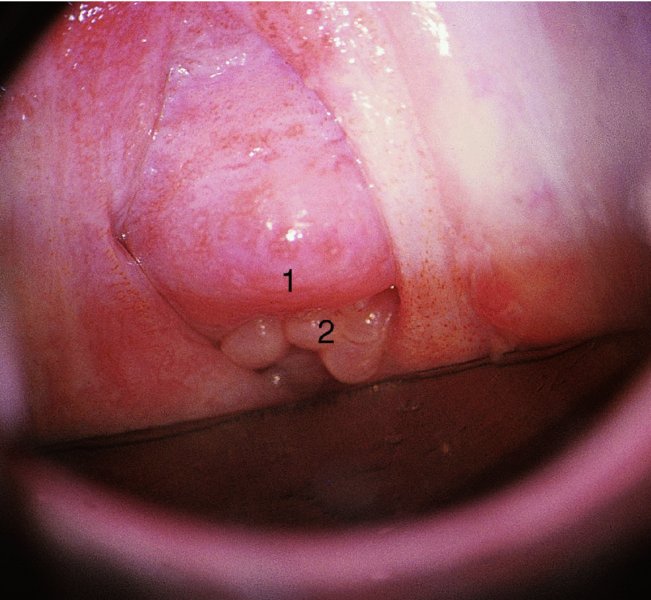
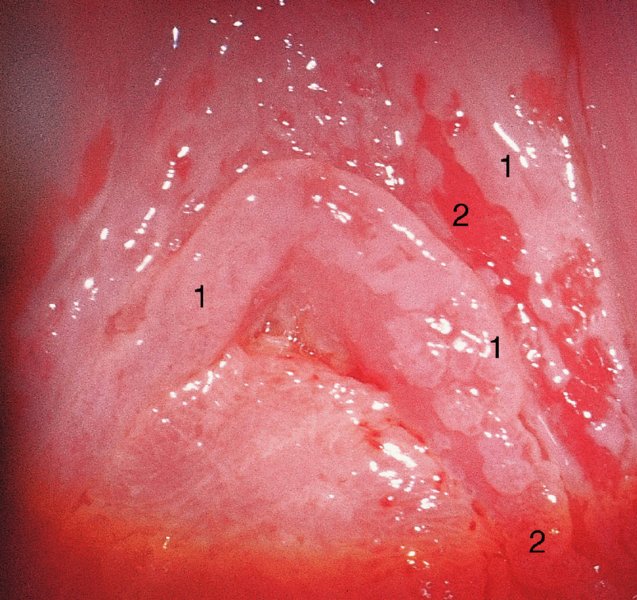
CHAPTER 11 Diethylstilbestrol (DES) was developed in the 1940s on the assumption that it prevented pregnancy complications, namely miscarriage. However, by the 1970s it was found that this was a false assumption, and soon it was realized that its usage was associated in young women with the occurrence of genital tract adenosis and of rare adenocarcinomas of the vagina and cervix in those who had been exposed in utero to DES. Now nearly four decades later the genital tract complications have virtually disappeared but more sinister genital and extragenital problems in this unfortunate cohort group are developing and will be discussed below. During the intrauterine life of the female fetus, the paired Müllerian paramesonephric ducts arise from the urogenital ridges, extend caudally, and then fuse at the urogenital sinus. This column of cells is replaced by a solid core of squamous epithelium that arises from the vaginal plate. The vaginal plate grows from the urogenital sinus, extends along the paired Müllerian ducts, and develops to form the major part of the vagina and cervix. In the newly born female child, the junction between the glandular Müllerian epithelium and the squamous epithelium extending from the urogenital sinus lies close to the external os of the cervix. The position of the squamocolumnar junction is quite variable. In the normal young girl, the vagina does not contain any glandular elements, except for occasional remnants that lie in the deep tissues and may form cystic structures (Gartner’s duct cysts) at a later date. From time to time, congenital variations of this development occur and remnants of the columnar epithelium may extend from the cervix onto the upper vagina, usually in an anteroposterior line. Later squamous metaplasia occurs in this area, producing the so-called congenital acetowhite changes (or congenital transformation zone) that are seen in a small number of individuals. Approximately 2.5% of women will have a squamocolumnar junction that extends from the cervix onto the vagina. Vaginal adenosis is a further variation of this development in that glandular epithelium is present in the vagina; this epithelium is of an endocervical type. It can either be on the surface, replacing the normal squamous epithelium, or occur as mucus-secreting cystic glands and crypts in the dermis. In1971, it was recognized for the first time that maternal ingestion of DES could lead to the development in female offspring of extensive cervicovaginal adenosis and rarely to adenocarcinoma of the vagina. DES was first produced in 1938 and was in clinical use by the mid-1940s. Since 1971, vaginal adenosis has been reported mainly in association with prenatal exposure to DES, but still may occur in women without such exposure. Adenosis found in females born prior to the DES era is similar in type to that found in women exposed to DES. The widespread use of colposcopy has meant that small areas of surface adenosis have been noted in asymptomatic women who have no history of DES exposure. The symptoms, when present, include profuse mucoid vaginal discharge, soreness, and/or postcoital bleeding resulting from the fragile and exposed glandular epithelium. The symptoms can be distressing and lead to concern about malignancy. Although an uncommon condition, it has been seen by the authors with increasing frequency and in two cases, seen by one of us (A.S.), it has been associated with pregnancy in which a postpartum hemorrhage necessitated the use of a vaginal pack. In both women, vaginal adenosis developed within 6 months; in one such case it was associated with erosive lichen planus of the vulva and vagina. Lichen planus in association with vaginal adenosis is also not very uncommon. Ingestion of DES and its effects on the offspring of women taking it had a profound effect on gynecology, especially in the USA, during the 1970s and 1980s. In the following section, the developmental anomalies caused by this drug will be discussed, and the clinical management will also be considered. The role of DES as a teratogen has been confirmed in other species. DES might act on the stroma and this could result in the production of some of the morphologic deformities and epithelial abnormalities of connective tissue that were seen in women exposed to DES. The increased risk of clear cell adenocarcinoma in the offspring of such women, especially those exposed in early pregnancy, may be due to large areas of the ectopic columnar epithelium in the vagina undergoing inductive changes, as described above. After its synthesis in 1938, DES was used, especially in the late 1940s, to treat patients with habitual abortion, on the understanding that the cause of abortion was a failure by the mother and her placenta to generate adequate levels of estrogen to support the pregnancy It was estimated that some 2–4 million women in the USA were treated with DES to support such worrying pregnancies. In 1970, clear cell adenocarcinoma of the vagina was noted in females aged 14–22 years. A special register was developed by Dr A.L. Herbst and has since been maintained in Boston, MA. This register has collected data from almost 400 clear cell adenocarcinomas of the vagina and cervix from around the world. The majority of these cases occurred in the USA, but a wide-ranging geographic pattern showed cases coming from Europe, Central America, Africa, and Asia. Clear cell adenocarcinoma of the cervix and vagina is a rare cancer but there has been a marked increase in reports of its incidence in recent years, both associated with DES and arising in untreated patients. These tumors are extremely rare in females under 14 years old; there then seems to be a rapid rise in the age–incidence curve to an irregular plateau with peak incidence rates around age 22. After this age, there seems to be a sharp decline in incidence. It is now obvious that these tumors are uncommon even in those females who have definitely been exposed to DES. It has been calculated that the risk of a clear cell adenocarcinoma developing in exposed women between birth and age 34 years is approximately one case per 1000. It has been extremely difficult to calculate the rate for females in their mid-twenties and older because only a small number of cases have been reported. However, it would seem that there is a life-long risk, because before the DES problem arose it was obvious that clear cell adenocarcinoma of both vagina and cervix was a disease of older women, and it may be that younger women who are at present free of malignancies could develop them at a later date. Following maternal ingestion of DES, the development of the fetal female genital tract is modified so that Müllerian columnar epithelium persists in the vagina, the fornices, and on the cervix. It appears that it is necessary for the fetus to be exposed to DES during the first 20 weeks of gestation for these abnormalities to develop. If DES treatment is begun after 20 weeks, the risks of generating the stigmata of DES changes are minimized. Figure 11.1 shows the characteristic features of an exuberant vaginal epithelium with a wide area of columnar epithelium present on the ectocervix (1). Figures 11.2 and 11.3 show the characteristic hooding surrounding a cervix that is entirely covered by persistent columnar epithelium; in Figure 11.4, squamous metaplasia (1) replaces the columnar epithelium; some hypertrophied endocervical columnar epithelium exists at (2). Figure 11.5 shows the columnar epithelium (2) extending onto the anterior lip, generating a characteristic cockscomb pattern. Squamous metaplasia has occurred in areas (1). Although most patients will develop stigmata associated with the cervix and upper vagina from time to time, patchy persistent columnar epithelium will be seen in other parts of the cervix and vagina. These patchy areas require careful monitoring. If there is any doubt about the nature of these lesions, a wide local excision should be undertaken and the material submitted for careful histologic assessment. The risk of development of clear cell cancer of the cervix or vagina in the patient exposed to DES is markedly increased if exposure occurred during early pregnancy (i.e., before 63 days); the risk beyond 63 days is nil. Not all fetuses will demonstrate stigmata, and the risks of development are as given above. The characteristic appearance of the clear cell carcinoma will be either hypertrophic, as shown on the anterior cervical lip (cervical hood) in Figure 11.6, or of an invading ulcer in the vagina or cervix (Figure 11.7). The most common site of occurrence is in the posterior vaginal fornix. The lesion is commonly diagnosed as an incidental finding at the time of assessment of the cervix.
Genital tract adenosis
11.1 Introduction
11.2 Developmental anatomy
11.3 Developmental anomalies caused by diethylstilbestrol
Epidemiology
Clinical findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


