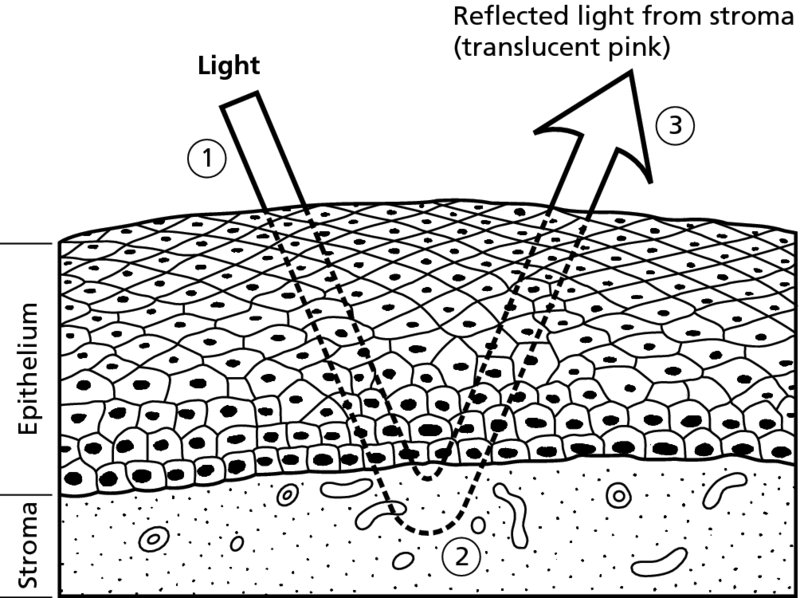
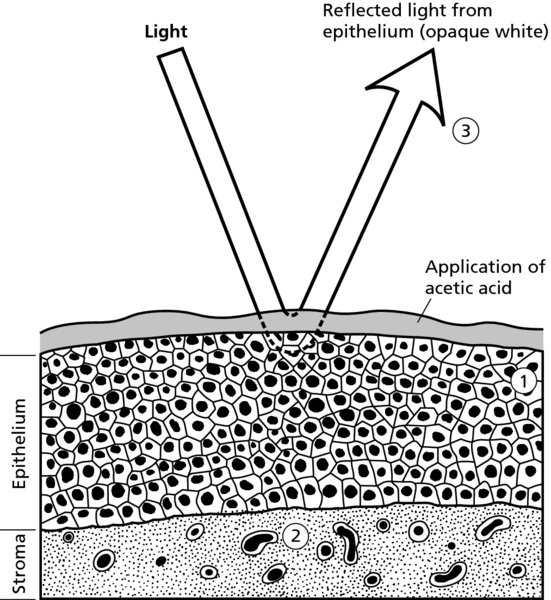
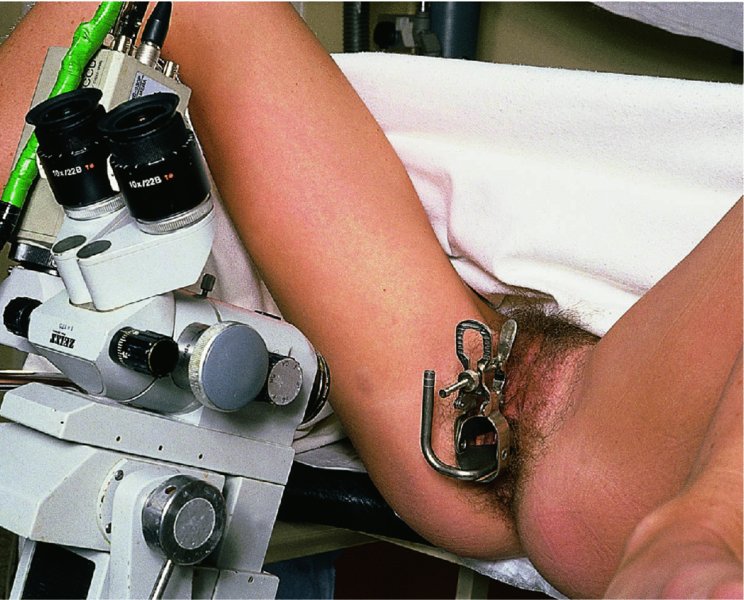
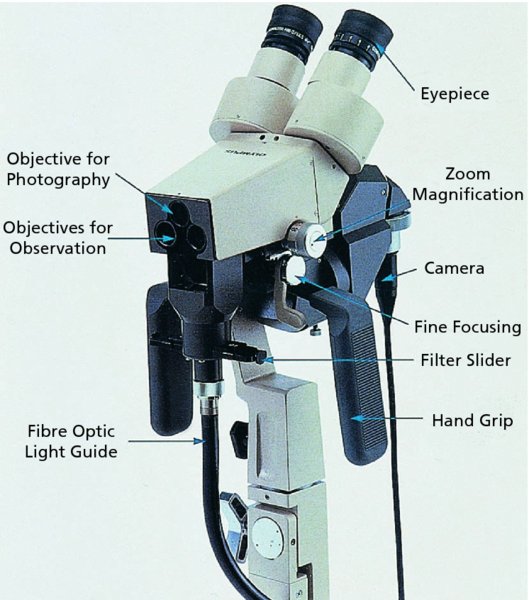
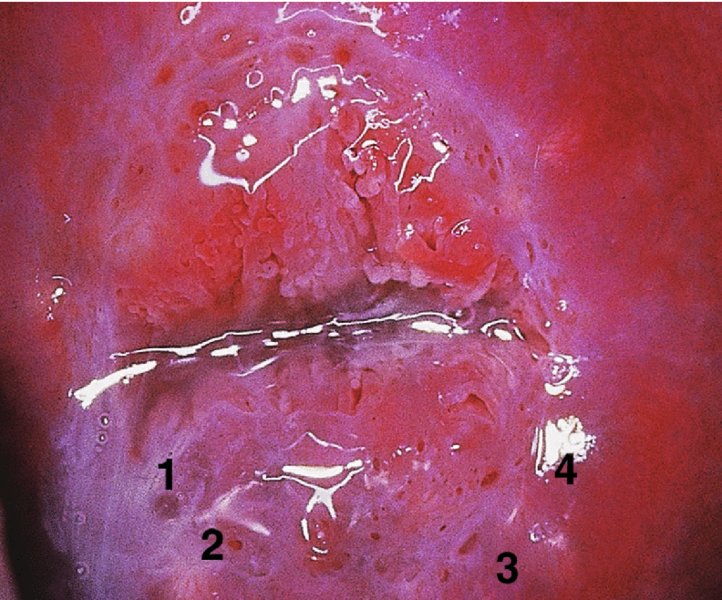
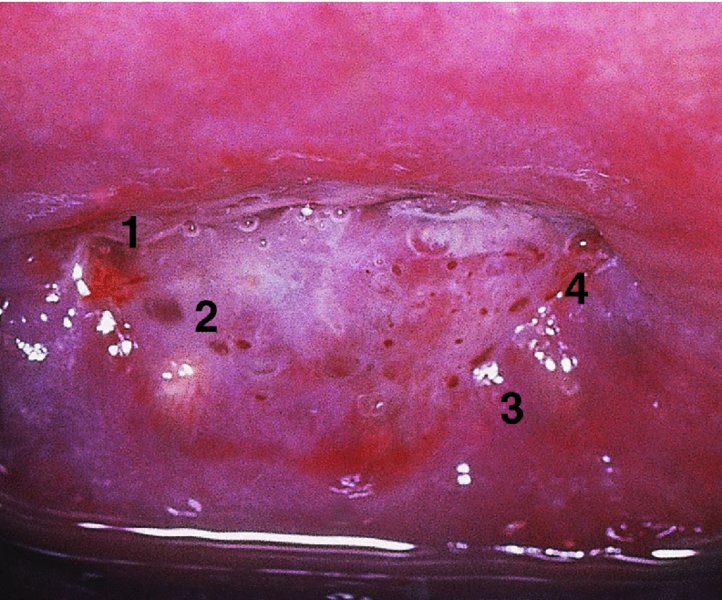
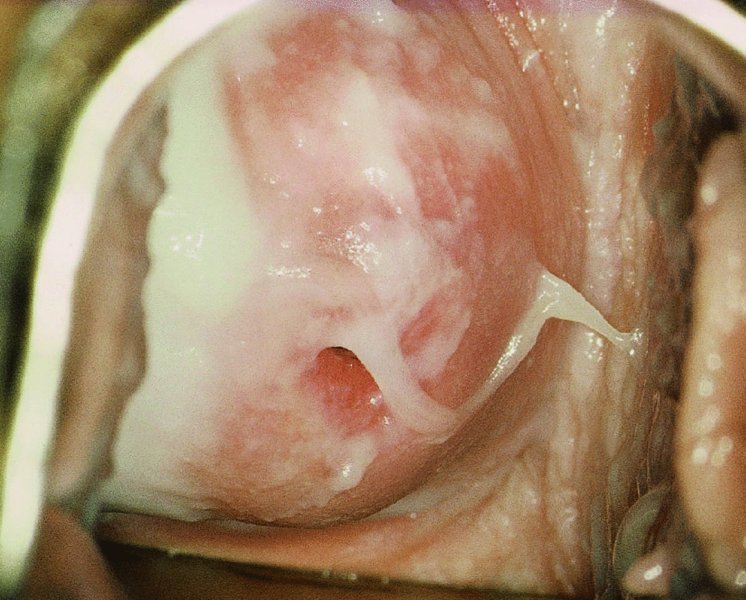
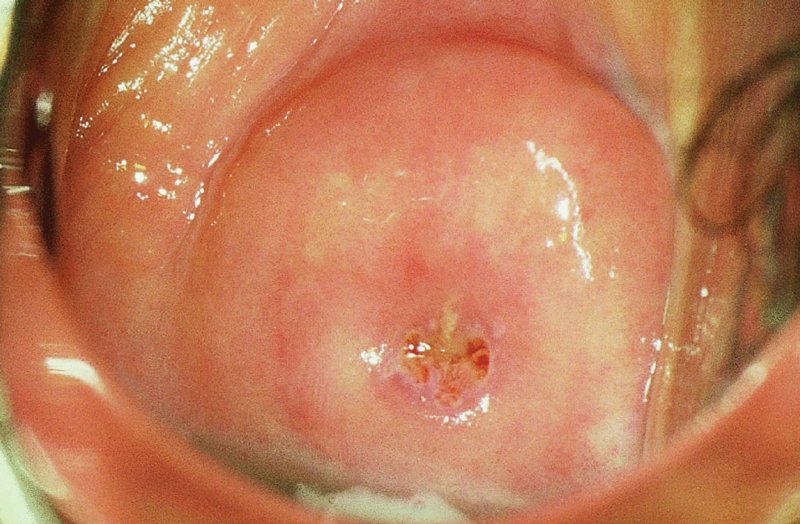
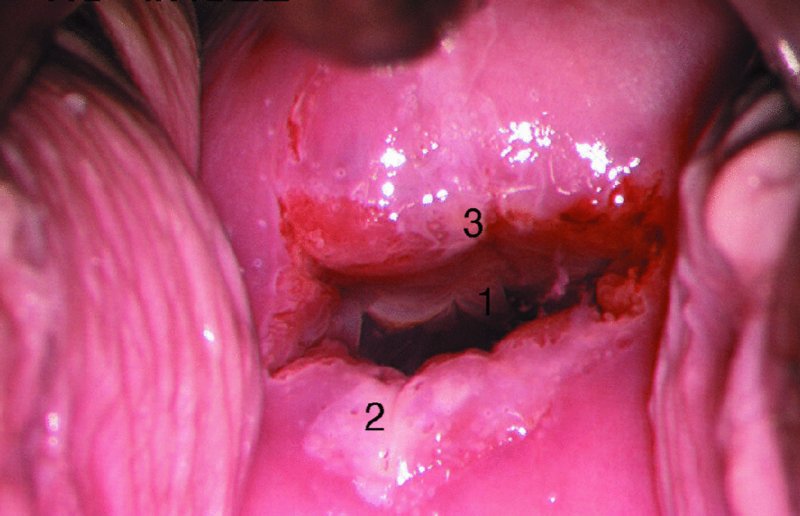
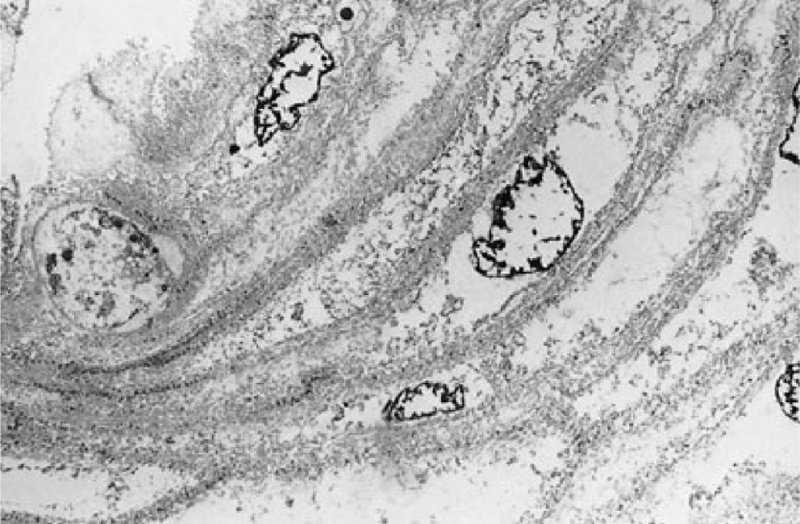
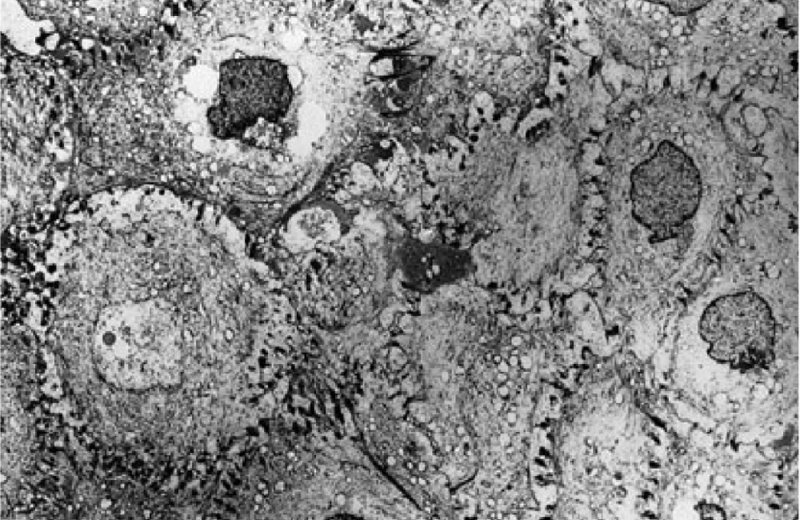
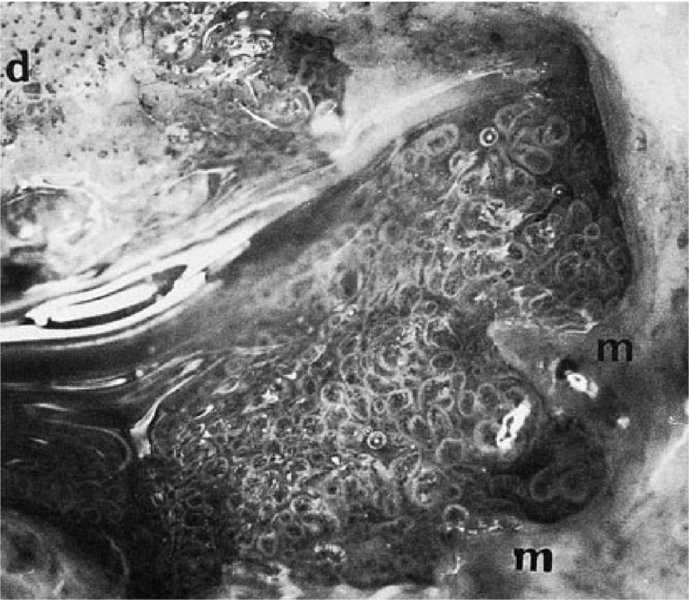
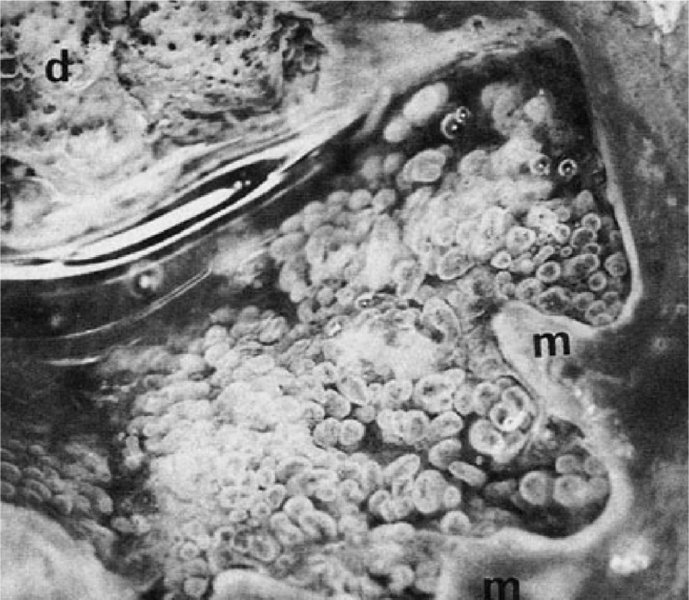
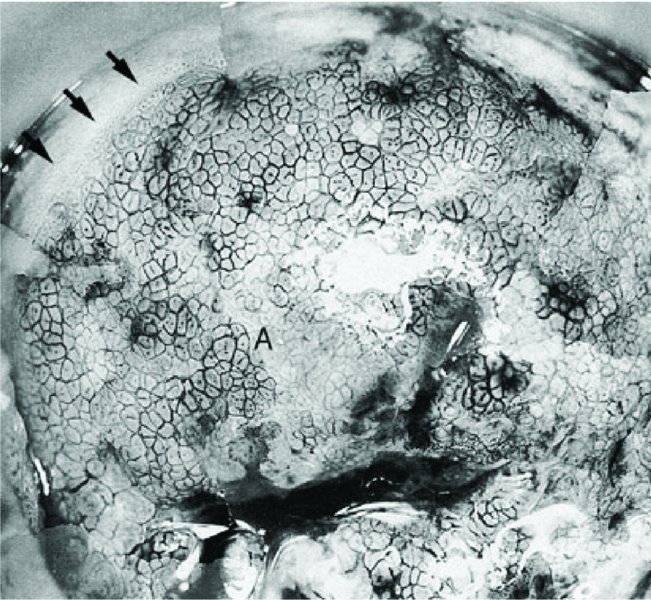
CHAPTER 3 In the detection of cervical intraepithelial neoplasia (CIN), exfoliative cytology, molecular tests for detecting the presence of human papilloma virus (HPV), and colposcopy are essential diagnostic aids. Alterations from the normal pattern, revealed during exfoliative cytology or a positive HPV finding, will have alerted the clinician to the possibility of an abnormality within the cervical epithelium. Use of the colposcopy, providing magnified and illuminated vision, enables the examiner to locate these changes. In this chapter the tissue basis for colposcopy and the colposcopic examination will be discussed. To interpret correctly the colposcopic appearance of normal and precancerous tissue a knowledge of the histopathologic changes that occur within the cervical epithelium and its stroma is required. It is essential that examiners are able to visualize what they have seen of the living tissues and to extrapolate that image to what is present in the fixed or stained tissue specimen under the microscope. The colposcopic appearances are a summation of various factors. These include the following. The image seen through the colposcope is therefore based on the reciprocal relationship between these three morphologic characteristics. The epithelium acts as a filter through which both the reflected and the incident light must pass to produce the final colposcopic picture. The epithelium is colorless, whereas the stroma is colored by the blood vessels it contains. The redness of the stroma is transmitted back to the observer, with modifications depending on the characteristics of the epithelium through which the light must pass. As seen in Figure 3.1, as the light passes through the normal epithelium it will be altered, depending upon a number of characteristics of the epithelium. The thickness, architecture, and resultant density of the epithelium will all produce alterations. The reflected light from the underlying stroma will impart a pink appearance to the normal epithelium. In Figure 3.2, the epithelium is abnormal (atypical) (1) and has an increased thickness and altered architecture, with the result that the reflected light imparts an opaque appearance, especially after the application of acetic acid. Figure 3.1 Normal epithelium. Figure 3.2 Abnormal (atypical) epithelium (cervical intraepithelial neoplasia). Various epithelial types modify the general features of the colposcopic appearance described above. In the normal cervix, glycogen-containing squamous epithelium, which is present during reproductive life, is thick and multilayered and acts as an effective filter, imparting a pink to reddish appearance when viewed colposcopically. The columnar epithelium is thin, contains mucus, and is highly translucent, resulting in a dense red colposcopic appearance. Within the bounds of the transformation zone, defined as the area in the columnar epithelium where a new squamous (metaplastic) epithelium forms, will be found metaplastic epithelium at various stages of development. It may be thinner than the normal squamous epithelium, devoid of glycogen, and appear reddish. Very rapidly regenerating epithelium, as seen in immature squamous metaplastic tissue, may adopt an opaque appearance. Abnormal epithelium contains the CIN stages, some of which will be precancerous. It differs from normal epithelium in that it is more cellular, with a higher nuclear content. The result is an opaque appearance, which has sometimes been described as deep red mixed with a dirty gray of whitish discoloration. The atrophic or postmenopausal, or indeed the prepubertal, squamous epithelium is thinner than normal squamous epithelium and devoid of glycogen. The stromal blood supply is reduced and, as seen later, is characterized by a pale red colposcopic appearance. When inflammatory infiltration occurs within the stroma, the resultant colposcopic appearance of the epithelium may be altered. The result may be a grayish white or yellowish appearance, dependent purely upon the degree of stromal inflammatory infiltration. This is determined by the surface shape and by the variations in thickness of the epithelium. The surface shape can be either smooth or papillary. Columnar epithelium, for example, is represented colposcopically as grape-like villi that, when pronounced, become conglomerated into the so-called columnar ectopy. Vascular patterns also become evident through the surface, as will be discussed later (Chapter 6). The capillaries may shine through the epithelium, either appearing as red dots on a white or opaque background, giving rise to so-called punctation, or arborizing within the stromal papillary ridges that subdivide the surface epithelium and thereby forming discrete fields, the so-called mosaic epithelium. An addition to the colposcopic image may occur when white patches, which can be seen by the unaided eye, appear on the surface epithelium. This so-called leukoplakia is due to a thick keratin covering that may overlie both histologic normal and abnormal epithelium. The combination of variable degrees of epithelial maturity, alterations in surface contour, and in blood vessel patterns, as described above, results in variation in the appearance of both normal and abnormal epithelia. There is no single appearance which can be called pathognomonic, especially for the abnormal epithelium; these changes therefore allow grading systems to be adopted. This helps in the identification of lesions that are insignificant or significant in respect of management; the former with minimal neoplastic potential, where invasion is years away (if it ever occurs), and the latter with a neoplastic potential with a high malignant potential. This grading system will be described later in Chapter 6, together with the Reid colposcopic index (see Table 6.2) and the recently described Swede score (see Table 6.4). The colposcope is a microscope providing illuminated magnification that allows the cervix to be viewed at between six- and 40-fold magnification. Originally developed by Hinselmann in the 1920s, it has gained popularity in the last five decades in Western Europe and North and South America. The colposcope lens has a focal length ranging between 200 and 300 mm; this establishes a comfortable working distance for the observer. Occasionally, the objective can be less, i.e., 125 mm; this is used predominantly when the saline method of colposcopy, a technique to demonstrate the vascular patterns within the surface epithelium, is employed. The colposcope is binocular and has eyepiece lenses (Figure 3.3a) that have a magnification range from six- to 12-fold. As seen in Figure 3.3 there are accessories to the colposcope itself. On most machines there is a tilting mechanism, a fine focus, binocular eyepieces, and a side arm that allows either a still or video camera to be attached. Another attachment sometimes used is a green filter; this may be inserted between the light source and the objective lens of the colposcope. It will absorb red light so that blood vessels become much darker and appear black and is used in particular when the saline technique is employed. Colposcopic examination is usually conducted with the patient placed in a modified lithotomy position on a suitable couch. The couch shown in Figure 3.3a makes use of a heel rest rather than the knee crutches that are sometimes employed. An instrument tray is placed beside the couch and on this tray are instruments that are essential for colposcopy. The legend to Figure 3.4 lists instruments that are used in the examination. Most important is the bivalve speculum, which may vary in width and length to allow the easy placement of the cervix between the blades. Occasionally the patulous walls of the vagina may fall in and obscure the view; in this situation a rubber condom, or the finger of a glove with the end cut off, can be placed around the blade, thereby keeping the vaginal walls away from the central viewing area. Lateral wall retraction, provided by attachments to the speculum or held by an attendant, can also be used to hold back patulous vaginal walls. Figure 3.4 A typical tray used in colposcopy: 1, pots with solution (acetic acid, saline, and Lugol’s iodine); 2, vaginal speculum; 3, sponge-holding forceps; 4, Desjardins’ endocervical forceps; 5, three-pronged probe for retraction; 6, cotton-tipped fine swab sticks; 7, Aylesbury cytology spatula; 8, larger cotton-tipped swab sticks; 9, local anesthetic syringe; 10, silver nitrate sticks for hemostasis; 11, endocervical brushes; 12, antibiotic cream; 13, cotton swabs; 14, diathermy electrodes for diagnosis or treatment; 15, Monsel’s solution (ferric subsulfate); 16, local anesthetic ampules; 17, Eppendorfer cervical biopsy forceps. Before examining the cervix, the vulva and vagina are inspected. This is important as there is a small but increased risk of vulval and vaginal neoplasia in women with cervical disease. The vulva can be examined with the naked eye, but the vagina should be viewed through the sixfold magnification of the colposcope. It is not usually necessary to take a cervical smear or a brush sample for HPV analysis before examination, but if it is necessary then it must be remembered that this could interfere with the surface epithelium. Abrasions and bleeding could be caused by an associated inflammatory condition such as Chlamydia trachomatis. When the speculum has been inserted and the cervix manipulated between the ends of the blades, the epithelia that are visualized are predominantly those on the ectocervix. Once the blades of the speculum have been opened, not only the ectocervix but also part of the endocervix becomes visible. This is shown in Figure 3.5a,b. In Figure 3.5a the speculum is fully opened and the cervix is in what is referred to as the “apparent view.” The endocervix with its columnar epithelium comes fully into view. The metaplastic squamous epithelium on the ectocervix, existing between points 1 and 4, is clearly seen. When the speculum is removed into the lower vagina, imitating the normal in vivo situation, the so-called “real view” becomes obvious. This view (Figure 3.5b) shows how the endocervical tissues have retracted and all that is “outside” on the ectocervix is the metaplastic squamous epithelium (between points 1 and 4). As will be discussed later, this epithelium has indeed developed as a result of the exposure of columnar epithelium to the effects of the vaginal environment (i.e., pH) during certain periods, such as pregnancy. It is usual to find a small amount of vaginal discharge, mixed with cervical mucus, covering and obscuring the area to be examined. A dry swab is normally used to remove the secretions. In Figures 3.6 and 3.7a, this procedure has taken place: the vaginal and cervical secretions (Figure 3.6) have been removed, allowing the cervix to be more easily visualized (Figure 3.7a). Visualization of the endocervix can be optimized if the examination is conducted at the mid-cycle. The profuse outflowing of clear cervical mucus allows an uninterrupted view of the endocervical tissues, as can be seen in Figure 3.7b. The endocervix is marked at (1) and an area of atypical (abnormal) epithelium is seen at (2) and (3). After the patient has been placed in the modified lithotomy position, the cervix is exposed, as shown in Figure 3.3, using a bivalve speculum. Solutions of acetic acid (3% or 5%) or normal saline are then applied to the cervix. Other solutions, such as Lugol’s iodine (1%), can also be applied. In the acetic acid technique, strengths of between 3% and 5% acetic acid are used; the solution is applied with either a cotton ball or spray. The acetic acid causes the tissues, especially the columnar and abnormal epithelia, to become edematous. Abnormal (atypical) epithelium adopts a white or opaque appearance, as described previously, which is then quite easy to distinguish from the normal epithelium, which appears pink. The acetic acid seems to act by causing the coagulation of epithelial and stromal cytokeratins in a reversible event. There also seems to be swelling of the tissues with an increase in the keratin filament proteins in the epithelium, which stain white with acetic acid. These keratin filament proteins, called cytokeratin, seem to be increased in association with cellular edema caused by acetic acid in this type of epithelium. There are 20 different cytokeratin polypeptides, but it is cytokeratin 10 which is believed to be an essential requirement for the formation of the so-called acetowhite epithelial change. The appearance of white areas within the atypical transformation zone following the application of 3% or 5% aqueous acetic acid solution is one of the basics of colposcopy. Its effect within the nucleus of cells is to precipitate nucleoprotein (Figure 3.7c). The cytoplasm undergoes vacuolation, the cell becomes swollen, and desmosomes are separated (Figure 3.7d). When acetic acid is applied to normal squamous epithelium, the penetration through the sparsely nucleated surface and intermediate layers produces little precipitation. The parabasal and basal cells of the epithelium contain more nucleoprotein, but this is not sufficient to obscure the color of the underlying cervical stroma with its rich network of subepithelial vessels, and the epithelium looks pink. When acetic acid is applied to areas of CIN, the precipitated nucleoprotein within the neoplastic cells obscures the underlying vessels, the light is reflected, and the epithelium appears white—acetowhite epithelium. With low-grade CIN the acid must penetrate into the lower half of the epithelium and the onset of “white” is delayed. High-grade or full-thickness CIN will give an almost instant response and will appear markedly “white.” The effect is slowly reversed because the acid is buffered and nucleoprotein is no longer precipitated. The appearances are not unique for neoplasia, and will be seen on other occasions when there is increased nucleoprotein present, for example during metaplasia, healing, and with the presence of virus or viral products. Figure 3.7(c) Transmission electron micrograph of superficial nucleated epithelial cells (cervical intraepithelial neoplasia) with precipitated nucleoprotein and cytoplasmic vacuolation. Figure 3.7(d) Transmission electron micrograph showing swelling of the cells and separation of desmosomes. It is usual to allow some time for the various changes within the epithelium to appear (Figures 3.8, 3.9). The cervix painted with a 5% solution will obviously respond quicker than one painted with a 3% solution. The effects will wear off in about 50–60 seconds. This is readily seen in Figures 3.10 and 3.11. In Figure 3.10 the cervix has had no acetic acid applied to it, whereas in Figure 3.11, 40 seconds after acetic acid application a whitish appearance has been produced. Figure 3.8 The transformation zone before the application of acetic acid: d, dysplasia; m, metaplasia. Figure 3.9 After the application of 3% acetic acid, the edematous columnar villi are seen in the central part of the picture; the metaplastic tissue (m) appears opaque and the dysplastic (d) area has a pronounced whiteness with small vessel punctation. Figure 3.10 In this figure a large ectropion (normal transformation zone) exists, with the endocervix at (1) and the ectocervix at (2). Figure 3.11 In this figure, after the application of 5% acetic acid, the squamous (metaplastic) epithelium that covers the ectocervix at (2) appears opaque and the area is clearly distinct from the surrounding pink squamous epithelium. Normally functioning squamous epithelial cells contain glycogen storage, which can be stained mahogany brown with Lugol’s iodine. Normal columnar cells do not contain enough glycogen storage and appear paler after application of iodine solution. Similarly transformation zones with precancerous or cancerous lesion contain very little or no glycogen. These areas appear pale yellow following application of Lugol’s iodine. Application of Lugol’s iodine is not essential, but it is an important part of colposcopic examination. It is especially helpful to clearly delineate the abnormal area prior to any treatment. Vaginal lesions can be better identified with an iodine test then with an acetic acid test. The saline technique, expounded by the late Professor Kolstad of Oslo, Norway, involves the application of a cotton wool swab, soaked in physiologic saline, to the cervix. This allows the subepithelial angioarchitecture to become obvious. A green filter must be used to identify the red vessels that appear dark and stand out most clearly. This allows the various vascular features of the atypical (abnormal) epithelium to be clearly visualized (Figures 3.12, 3.13). Figure 3.12 An atypical transformation zone showing a large area of mosaic epithelium characterized by large intercapillary distances. This is clearly seen at (A) and the original squamocolumnar junction is arrowed. Figure 3.13 Atypical vessels (at) are clearly seen within the transformation zone with two areas of punctation (p). The sharp edge of the transformation zone is arrowed. HPV and human immunodeficiency virus (HIV) are associated with serious genital tract pathology. This has made it imperative that the decontamination of any equipment used in the colposcopy clinic is 100% reliable. Before the choice of instruments is made, one of the parameters which must be assessed is the ease with which decontamination may be accomplished. The hazard to the patient arises from the flora of the vagina and contamination with blood or serum. Although bacteria are easily dealt with largely by cleaning, the hazards posed by the blood-borne viruses (hepatitis A and C, and HIV) and the local viral pathogens (HPV and herpes simplex virus) are perhaps more emotive. It is now normal practice in most clinics in developed countries to use single-use sterilized equipment. Otherwise the rules that should be followed are simple: The local disinfection policies should be observed and local expert guidance sought. There is also value in using disposable instruments, especially vaginal speculi. However, this is an expensive exercise and there is no reason why, if the above decontamination procedures and principles are followed, concern should arise either in the patient or in the colposcopist.
Examination for cervical precancer: Use of colposcopy
3.1 Introduction
3.2 Tissue basis for colposcopy
The role of the epithelium
The role of the stroma
The role of the surface configurations or patterns
3.3 The colposcopic examination
The colposcope
The examination

Application of acetic acid


Application of Lugol’s iodine
Application of saline

Decontamination of colposcopy clinic equipment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


