FIGURE 44-1 Preoperative radiograph of a 13-year-old male with a history of Ewing’s sarcoma of the left humerus, previously treated with tumor resection and intercalary allograft reconstruction. He went on to develop a symptomatic fracture nonunion at the proximal host-graft junction.
Free Vascularized Fibula Grafts
Wouldn’t it be interesting to have an occasional zebra in a horse race?
—The Vent
The fibula has long been recognized as an attractive choice for vascularized bone grafting procedures.3,4 The fibula bears only 15% of the axial load across the ankle, allowing for its use as an autogenous bone graft with minimal biomechanical consequences on the weightbearing status of the lower limb.5 As the distal fibula also plays an important role in conferring rotational stability and restraint against lateral translation of the talus, the distal fibula is preserved during graft harvest to avoid subsequent ankle deformity or instability.6–9
Furthermore, the vascular supply to the fibula has been well established.4,9 The endosteal blood supply to the fibula is provided by a nutrient artery, which typically enters the posterior fibular cortex at the junction of the proximal one-third and distal two-thirds. This nutrient artery is a branch of the peroneal artery, which runs along the posterior aspect of the fibular diaphysis. The fibula receives additional vascularity via a number of segmental musculoperiosteal vessels, which also emanate from the peroneal artery. Based upon this understanding of the vascularity of the fibula, techniques of vascularized fibula graft harvest have been developed that preserve both the nutrient artery and the rich periosteal blood supply.
Free vascularized fibular grafting has a number of additional theoretical advantages over conventional, non-vascularized bone grafting techniques. Given the length of fibular diaphysis that may be harvested, free fibular grafts are well suited for the reconstruction of segmental defects of the long bones, providing both mechanical strength and biological stimulus for healing. Furthermore, based upon the fasciocutaneous arterial branches of the peroneal artery, skin, fascia, and muscle may be harvested concomitantly with the fibula to allow for more complex soft tissue reconstruction. Finally, given the ability to transfer the proximal fibular epiphysis with the diaphysis during FVFG, there is potential for preserving continued skeletal growth of the fibular graft.10
Despite its many theoretical advantages and applications, however, FVFG is technically challenging and confers its own set of inherent risks and potential complications. Sound microsurgical technique is essential in performing the required arterial and venous anastomoses and ensuring long-term graft viability. Furthermore, donor site morbidity has been well documented, and up to 10% of patients may subsequently develop ankle pain, instability, and/or progressive valgus deformity if fibula harvest is not performed with proper technique.7,8 Given these considerations, FVFG should be employed in specific clinical situations.
Table 44.1 Properties of bone grafts
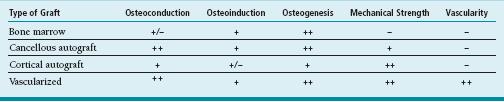
From Buckwalter JA, Einhorn TA, Simon SR, eds. Orthopaedic Basic Science. Chicago, IL: American Academy of Orthopaedic Surgeons; 2000.
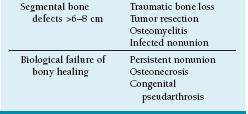
Currently, the indications for FVFG fall into two categories11 (Table 44.2). The first indication is for segmental bony defects of >6 to 8 cm, such as seen in tumor resection, posttraumatic, or postinfectious bone loss. The second indication is for smaller bony defects in which there has been a biological failure of bony healing, such as seen in recalcitrant fracture nonunions, congenital pseudarthroses, and osteonecrosis. In addition, there has been recent work examining the use of free vascularized fibular periosteum—with or without small “matchstick” strips of cortical bone—to bring biological bony healing potential to areas of bony defects or failed healing. While we have no personal experience with this technique, the potential applications are great and principles are similar to what is presented here.
Applications in Pediatric Hand and Upper Extremity Surgery
Congenital Ulnar Pseudarthrosis
Congenital ulnar pseudarthrosis is a rare abnormality of skeletal growth characterized by the development of pathological fractures of the ulna and long-standing pseud-arthroses. Often associated with neurofibromatosis or fibrous dysplasia, congenital ulnar pseudarthrosis may lead to pain, deformity, and growth disturbance (see Chapter 48). Traditional methods of fracture care, including open reduction and internal fixation with nonvascularized bone grafting, are often unsuccessful. For these reasons, we have utilized FVFG to achieve bony healing in these challenging cases.12,13 In addition to achieving bony healing across the site of the previous pseudarthrosis, careful restoration of ulnar length and alignment will result in preserved elbow and wrist motion and distal radioulnar joint (DRUJ) stability. Furthermore, when used in an intercalary fashion, vascularized fibula grafts can result in revascularization of the dystrophic, hypoplastic distal ulnar segment.
In addition, in the very young with marked growth remaining, concomitant proximal fibular epiphyseal transfer can preserve skeletal growth of the ulna. If successful, this will maintain a balanced wrist and forearm throughout skeletal maturation10,12 (Figure 44-2).
Allograft Nonunion
Limb salvage surgery is an appealing option in skeletally immature patients with malignant bone tumors. In these situations, an intercalary or osteoarticular allograft is often utilized during bony reconstruction. Unfortunately, allograft fracture occurs in up to 20% of cases, and traditional methods of fracture care are often unsuccessful in these cases due to the high mechanical stresses and altered biological milieu.14 In these situations, FVFG has been proposed to promote fracture healing while preserving allograft structural integrity. Vascularized grafts have been used both: (1) during primary tumor resection and allograft reconstruction and (2) during allograft fracture nonunion reconstruction. In our institution, FVFG is predominately applied to secondary reconstruction of allograft fracture nonunion.15 About 90% of osteogenic sarcoma and Ewing sarcoma patients with upper limb allograft fracture nonunion will achieve successful bony healing following free fibular grafting. These patients will maintain limb preservation, with pain relief, extremity stability, and satisfactory functional outcomes.
Despite relatively high complication rates, we support the use of FVFG in these complex clinical situations. Careful attention to rigid internal fixation, meticulous microvascular surgical technique, and anatomic limb alignment is essential to optimize clinical outcomes.
Osteonecrosis of the Femoral Head
Osteonecrosis of the femoral head continues to be a cause of pain and disability to thousands of adolescents and young adults each year.16 This is particularly true in the pediatric patient population, where osteonecrosis of the femoral head may be a result of hip trauma, septic arthritis of the hip, slipped capital femoral epiphysis, Legg-Calve-Perthes disease, or chronic steroid use (such as seen following solid organ transplantation). While many treatments have been proposed, no universal solution has been found.
The use of FVFG has been proposed to provide mechanical support to and revascularization of the femoral head16–18 (Figure 44-3). Dean et al., in one of the largest published series of pediatric patients, reported the early results of free fibular grafting in 50 patients, with mean age of 14.8 years. The majority of patients developed osteonecrosis as a result of prior hip trauma, slipped femoral epiphysis, or steroid use. Average Harris Hip Scores improved from 55 preoperatively to 90 postoperatively, and at most recent follow-up, only 16% of patients had clinical symptoms or radiographic progression severe enough to warrant conversion to hip arthrodesis or arthroplasty. Based upon these results, the authors conclude that free fibular grafting in pediatric patients with femoral head osteonecrosis may relieve pain, improve function, and delay the need for future hip arthroplasty.
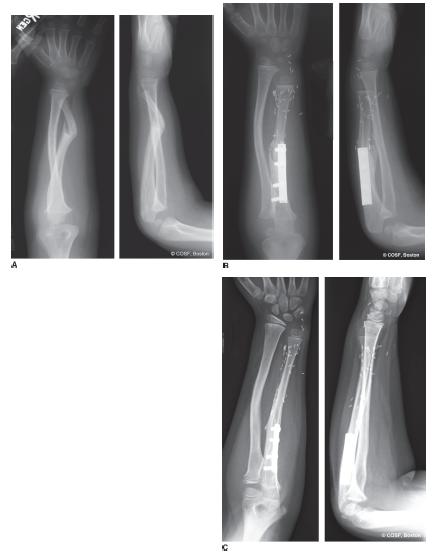
FIGURE 44-2 A: Forearm radiographs depicting a congenital ulnar pseudarthrosis in the setting of neurofibromatosis. B: Initial postoperative radiographs following distal ulnar resection and FVFG with concomitant proximal epiphyseal transfer. C: Follow-up radiographs demonstrating bony healing, preserved bony alignment, and longitudinal growth of the fibular graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree