Background
Atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion in abnormal cervical cytology among young women in cervical cancer screening is an increasing health burden, and comparative effectiveness studies of different management options for such diagnoses are needed.
Objective
The objective of the study was to compare the incidence of invasive cervical cancer, following different management options pursued after an atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion index smear.
Study Design
In this nationwide cohort study, we included all women aged 22-50 years and resident in Sweden 1989–2011 and with at least 1 cervical smear registered during the study period (n = 2,466,671). Follow-up of a first atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion cytological diagnosis within 25 months was classified as repeat cytology, colposcopy/biopsy, or without further assessment. Incidence rate ratios and 95% confidence intervals of subsequent cervical cancer within 6.5 years following atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion were estimated using Poisson regression by age group and management strategy.
Results
Women managed with repeat cytology within 6 months after atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion cytology had a similar risk of cervical cancer compared with colposcopy/biopsy (incidence rate ratio, 1.1, 95% confidence interval, 0.5–2.5, and incidence rate ratio, 2.0, 95% confidence interval, 0.6–6.5, respectively) among women aged 22–27 years. For women aged 28 years and older, women managed with repeat cytology had a higher risk for cervical cancer than women managed with colposcopy/biopsy.
Conclusion
Our findings suggest that women with a first cytological diagnosis of atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion up to age 27 years may indeed be safely followed up with repeat cytology within 6 months. A large amount of colposcopies that are currently performed in this group, therefore, could safely be discontinued.
In cervical screening of women under 30 years of age, atypical squamous cells of undetermined significance and low-grade squamous intraepithelial lesions are common and are increasing in incidence. Although these cytological diagnoses may signal significant risk of underlying high-grade histological cervical lesions, in young women these may have a high potential to regress spontaneously.
We previously showed that women with atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion who were referred to colposcopy and biopsy had the greatest cervical cancer risk reduction. This subsequently became the management policy in Sweden. However, our previous study was not powered to analyze cancer risk by age group. Because these lesions are common and are increasing among young women, this policy is a significant burden to both women and the health care system. Triaging with human papillomavirus (ie, referring only human papillomavirus-positive women to colposcopy/biopsy) is of limited usefulness because the human papillomavirus prevalence in atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion is very high in young women.
Comparative effectiveness research is used to study the effectiveness of health care as actually practiced in obtaining the desired effects, in our case that the management should achieve a reduced incidence of cervical cancer. To ensure adequate statistical power and optimal generalizability, we studied all cases of atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion that had been found in the entire country of Sweden over a period of 22 years to assess whether follow-up with colposcopy and biopsy is indeed necessary to achieve the desired effect. The cervical cancer risk following an atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion result was thus determined by management policy and age group to determine whether the currently used management policies are effective.
Materials and Methods
Study participants
The Swedish National Cervical Screening Registry has records of organized and opportunistic cervical screening since 1969 and is 100% complete for the nation since 1995. The National Cervical Screening Registry contains data on all tests, all biopsies from the genital tract, and all invitations issued in the national cervical screening program.
Women are invited to screening every 3 years from age 23 years and every 5 years between 50 and 60 years of age. Using the National Cervical Screening Registry, we constructed a population-based cohort including all women resident in Sweden at any time between Jan. 1, 1989 and Dec. 31, 2011, who had at least 1 cytology test registered between the ages of 22 and 50 years.
The Swedish individually unique personal identification numbers were used to link the study cohort to the Swedish nationwide and complete Patient, Cancer, Migration, and Cause of Death Registers. After linkage completion, all data were deidentified. Thus, we were able to follow up every woman from the first cytology registered during the study period until diagnosis of invasive cervical cancer, total hysterectomy, emigration, death, or Dec. 31, 2011, whichever came first.
Cytological diagnoses
We classified all cytology tests in the cohort into normal, atypical squamous cells of undetermined significance, cervical intraepithelial neoplasia grade 1, or other abnormalities. Cervical intraepithelial neoplasia grade 1 in Swedish clinical cytology terminology translates to a diagnosis of low-grade squamous intraepithelial lesion in the Bethesda system. We then identified all women who received a first cytological diagnosis of normal, or a first abnormal diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion, and classified this as their index cytology. Women who received a first cytological diagnosis of other abnormalities (such as high-grade squamous intraepithelial lesion) were censored from further follow-up.
Prevalent and incident cancer
We used the Swedish National Cancer Register to identify all cases of pathology-confirmed invasive cervical cancer ( International Classification of Diseases, Seventh Revision , code 171) diagnosed within 6.5 years following the index cytology in the cohort. We classified the subsequent diagnosis of invasive cervical cancer as a prevalent cancer if it was diagnosed within 6 months of the index cytology (ie, within 0–0.5 years) and an incident cancer if it was diagnosed after more than 6 months (ie, within 0.5–6.5 years), as previously described.
The interval for follow-up of incident cancer for an additional 6 years was chosen because it gave adequate person-time in each category for the study question and represented 2 screening intervals, which was regarded as a reasonable time frame for inference on results following the original index smear.
Further assessment
To assess the risk of incident cervical cancer following different diagnostic work-up options, we classified different strategies for further assessment within 25 months following an atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion diagnosis into the following categories: (1) histology, which was any histology from the cervix was taken; (2) cytology only, which was follow-up only with repeated cytology test(s); or (3) no morphological follow-up, which was neither histology nor cytology registered.
In this analysis, we excluded all histology procedures registered within 60 days prior to a cervical cancer diagnosis because this test was likely to have led to the detection of a prevalent cancer. For the same reason, we also excluded all cytologies recorded within 6 months prior to a cancer diagnosis. If the registration dates of cytology and histology were <8 days apart, they were considered to belong to the same visit and were categorized as assessed with histology.
The group followed up with cytology only was further subdivided according to in which time window the repeated smear occurred: 0–6 months or 7–25 months and whether the repeat smear was recorded as cytologically normal or abnormal.
Statistical analyses
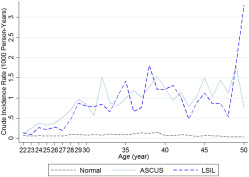
Descriptive data showed that the risk of cervical cancer after atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion cytology increased sharply after age 27 years ( Figure 1 ). We thus defined women aged 22-27 years at the index cytology as a younger group, whereas women ages ≥28 years were considered as belonging to an older group.
All analyses were performed separately for these 2 age groups. First, we examined the risk of subsequent cervical cancer among women with an atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion diagnosis, compared with women with normal cytology. Women were considered to be unexposed for 5 years after each normal cytology, and the age at entry (in years) in the unexposed group for each woman who had a normal cytology was randomly selected to avoid oversampling of unexposed compared with exposed risk-time. Women who received a first diagnosis of atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion contributed to the exposed group thereafter.
We estimated crude incidence rates and 95% confidence intervals of cervical cancer using the number of cancer cases divided by the accumulated person-years in each of these groups, respectively. Using Poisson regression, we then estimated the incidence rate ratios of subsequent cervical cancer among exposed women, compared with women with normal cytology.
Incidence rate ratios were estimated separately for the 2 age groups (age 22–27 and age 28–50 years) and stratified on prevalent or incident cancer status. Furthermore, we investigated the associations between further assessment options and subsequent incident cancer among women with an atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion diagnosis, again using Poisson regression.
Histological assessment was used as the gold standard reference group. We included an interaction term between further assessment strategy and age group and reported the P value for this interaction term as a statistical significance test of the difference between the incidence rate ratios.
We also performed these analyses using the incidence rate in women with normal cytology as the reference group instead to show the risk elevation parametrized according to the baseline incidence rate in a cytologically normal population of women. Finally, we summarized the absolute number of atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion diagnoses as well as results from repeat cytologies obtained in Sweden during 2010.
All statistical models were adjusted for age at smear and all statistical tests were two sided. A value of P < .05 was considered as statistically significant. We used SAS version 9.3 (SAS Institute, Cary, NC) for all statistical analyses.
The study was approved by the Regional Ethical Committee in Stockholm, Sweden, which also waived the requirement of obtaining informed consent from the study participants.
Results
In total, we included 2,466,671 women with a median follow-up of 9.9 years. During the study, 2,415,269 of these women had ≥1 normal cytology registered. Of these, 190,977 women received a first cytological diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion during the study period, 71,449 of which were aged 22-27 years at the index cytology and 119,528 of which were aged 28-50 years at the index cytology ( Table 1 ).
| Characteristics | Normal a | ASCUS/LSIL, younger | ASCUS/LSIL, older |
|---|---|---|---|
| Participants, n | 2,415,269 | 71,449 | 119,528 |
| Diagnosis of cytology | |||
| ASCUS | 0 | 33,764 (47.3) | 63,009 (52.7) |
| LSIL | 0 | 37,685 (52.7) | 56,519 (47.3) |
| Age at entry | |||
| 22–24 | 768,773 (27.4) | 40,767 (57.1) | — |
| 25–27 | 287,710 (10.3) | 30,682 (42.9) | — |
| 28–30 | 261,751 (9.3) | — | 23,624 (19.8) |
| 31–35 | 408,897 (14.6) | — | 29,566 (24.7) |
| 36–40 | 385,374 (13.7) | — | 22,887 (19.2) |
| 41–45 | 381,949 (13.6) | — | 22,237 (18.6) |
| 46–50 | 315,791 (11.2) | — | 21,214 (7.4) |
| Calendar periods at entry | |||
| 1989–1994 | 1,258,897 (44.8) | 13,241 (18.5) | 24,728 (20.7) |
| 1995–2000 | 621,311 (22.1) | 15,176 (21.2) | 31,205 (26.1) |
| 2001–2006 | 478,013 (17.0) | 19,070 (26.7) | 31,655 (26.5) |
| 2007–2011 | 452,024 (16.1) | 23,962 (33.5) | 31,940 (26.7) |
a Women were considered to be unexposed for 5 years after each normal cytology. Therefore, one woman could contribute multiple normal periods to the normal group.
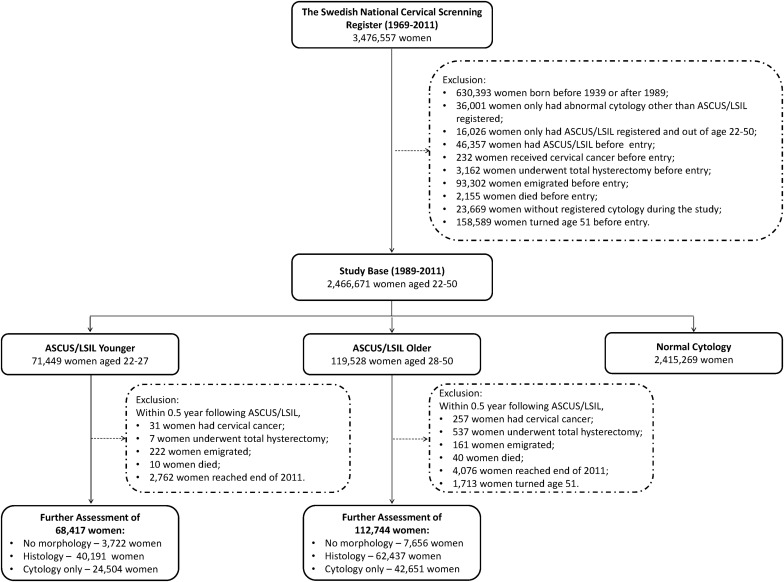
Among these 2 groups, 68,417 younger and 112,744 older women, respectively, were eligible for the analysis of further assessment ( Figure 2 ). In total, 222 invasive cancers occurred within 0–6.5 years in women aged 22–27 years: 151 squamous cell carcinomas (68%), 49 adenocarcinomas (22%), and 22 tumors of other histological type such as adenosquamous carcinomas (10%). Among women aged 28–50 years, 715 cancers occurred within 0–6.5 years: 504 squamous cell carcinomas (70.5%), 172 adenocarcinomas (24%), and 39 of other histological type such as adenosquamous carcinomas (5.5%).
Prevalent invasive cervical cancer was very uncommon among young women with normal cytology but was more common in women with atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion: 18 prevalent cases among women with an atypical squamous cells of undetermined significance diagnosis and 13 among women with low-grade squamous intraepithelial lesion. Among these, all 18 who were followed up with cytology first were diagnosed as cytologically abnormal upon the repeat smear. In the older age group, however, the prevalent case load was higher (for frequencies of prevalent and incident cancer, see Table 2 ).
| Time since cytology | Normal | ASCUS | LSIL | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC | P-Ys | Crude IR | IRR | CC | P-Ys | Crude IR | IRR (95% CI) | CC | P-Ys | Crude IR | IRR (95% CI) | |
| Age 22-27 y | ||||||||||||
| 0–6.5 y | 222 | 3,806,604 | 0.06 | Ref. | 48 | 156,028 | 0.31 | 5.5 (3.9–7.5) | 37 | 196,210 | 0.19 | 3.4 (2.3–4.7) |
| 0–0.5 y a | 4 | 297,821 | 0.01 | Ref. | 18 | 16,379 | 1.10 | 106.7 (39.3–372.5) | 13 | 18,479 | 0.70 | 68.9 (24.1–246.8) |
| 0.5–6.5 y | 218 | 3,508,783 | 0.06 | Ref. | 30 | 139,649 | 0.21 | 3.5 (2.3–5.0) | 24 | 177,731 | 0.14 | 2.2 (1.4–3.3) |
| 0.5–1.5 y | 9 | 607,552 | 0.01 | Ref. | 8 | 30,075 | 0.27 | 16.7 (6.1–45.0) | 9 | 34,995 | 0.26 | 16.2 (6.1–42.6) |
| 1.5–2.5 y | 30 | 629,248 | 0.05 | Ref. | 6 | 26,971 | 0.22 | 4.9 (2.0–11.9) | 0 | 32,529 | 0.00 | — |
| 2.5–3.5 y | 41 | 621,855 | 0.07 | Ref. | 6 | 24,265 | 0.25 | 3.4 (1.3–7.5) | 6 | 30,410 | 0.20 | 2.7 (1.0–6.0) |
| 3.5–4.5 y | 55 | 594,166 | 0.09 | Ref. | 2 | 21,741 | 0.09 | 1.0 (0.2–3.2) | 2 | 28,407 | 0.07 | 0.8 (0.1–2.5) |
| 4.5–5.5 y | 40 | 549,711 | 0.07 | Ref. | 4 | 19,342 | 0.21 | 2.8 (0.8–7.0) | 2 | 26,498 | 0.08 | 1.0 (0.2–3.3) |
| 5.5–6.5 y | 43 | 506,251 | 0.08 | Ref. | 4 | 17,254 | 0.23 | 3.2 (1.0–8.1) | 5 | 24,891 | 0.20 | 2.8 (1.0–6.6) |
| Age 28-50 y | ||||||||||||
| 0–6.5 y | 715 | 9062,936 | 0.08 | Ref. | 284 | 272,513 | 1.04 | 13.0 (11.3–14.9) | 260 | 276,588 | 0.94 | 11.6 (10.0–13.4) |
| 0–0.5 y a | 34 | 690,254 | 0.05 | Ref. | 140 | 30,355 | 4.61 | 94.1 (65.5–139.0) | 117 | 27,581 | 4.24 | 87.3 (60.3–129.9) |
| 0.5–6.5 y | 681 | 8,372,682 | 0.08 | Ref. | 144 | 242,158 | 0.59 | 7.1 (5.9–8.4) | 143 | 249,006 | 0.57 | 6.7 (5.6–8.0) |
| 0.5–1.5 y | 61 | 1,424,414 | 0.04 | Ref. | 74 | 54,557 | 1.36 | 31.8 (22.7–44.7) | 68 | 51,366 | 1.32 | 31.1 (22.0–44.1) |
| 1.5–2.5 y | 82 | 1,455,800 | 0.06 | Ref. | 12 | 47,694 | 0.25 | 4.4 (2.3–7.7) | 10 | 46,787 | 0.21 | 3.7 (1.8–6.8) |
| 2.5–3.5 y | 154 | 1,460,080 | 0.11 | Ref. | 15 | 42,527 | 0.35 | 3.3 (1.9–5.4) | 19 | 43,075 | 0.44 | 4.1 (2.5–6.4) |
| 3.5–4.5 y | 161 | 1,441,999 | 0.11 | Ref. | 13 | 37,232 | 0.35 | 2.9 (1.6–5.0) | 17 | 39,397 | 0.43 | 3.6 (2.1–5.7) |
| 4.5–5.5 y | 114 | 1,350,258 | 0.08 | Ref. | 15 | 32,162 | 0.47 | 4.9 (2.8–8.2) | 13 | 35,754 | 0.36 | 3.7 (2.0–6.4) |
| 5.5–6.5 y | 109 | 1,240,131 | 0.09 | Ref. | 15 | 27,986 | 0.54 | 5.3 (2.9–8.8) | 16 | 32,627 | 0.49 | 4.7 (2.7–7.7) |
a For the time interval 0–0.5 years after diagnosis, prevalent rates and prevalence rate ratios for cervical cancer are presented.
Among the women aged 28–50 years who were diagnosed with prevalent cancer within 6 months, 11 of 123 of those who underwent repeat smear (9%) first had been diagnosed as cytologically normal on the repeat smear ( Supplemental Table 1 ).
The risk for incident cervical cancer during the 0.5–6.5 years after the index cytology was 2–4-fold increased for women with atypical squamous cells of undetermined significance (incidence rate ratio, 3.5, 95% confidence interval, 2.3–5.0 among women aged 22–27 years, and incidence rate ratio, 2.2, 95% confidence interval, 1.4–3.3 among women aged 28–50 years) and even higher for women with low-grade squamous intraepithelial lesion (incidence rate ratio, 7.1, 95% confidence interval, 5.9–8.4, and incidence rate ratio, 6.7, 95% confidence interval, 5.6–8.0, respectively).
These risks were consistently elevated, regardless of the time window since index cytology but were greatest in the first 0.5–1.5 years ( Table 2 ). The incidence rate ratio for cancer after atypical squamous cells of undetermined significance in young women further assessed with repeat cytology only was similar to that in women assessed with histology (incidence rate ratio, 1.1, 95% confidence interval, 0.4–2.5). Whether the repeat cytology occurred within 0–6 or 7–25 months did not change this estimate. However, having no further follow-up assessment recorded after an atypical squamous cells of undetermined significance smear was associated with an increased risk compared with being assessed with histology (incidence rate ratio, 5.1, 95% confidence interval, 1.9–12.4) ( Table 3 ).
| Cytology | Further assessment | Subsequent CC among women aged 22–27 y | Subsequent CC among women aged 28–50 y | P value for difference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obs. | Exp. | P-Ys | Crude IR | IRR (95% CI) | Obs. | Exp. | P-Ys | Crude IR | IRR (95% CI) | |||
| Any | Histology | 19 | 19 | 181,440 | 0.10 | Ref. | 84 | 84 | 273,185 | 0.31 | Ref. | |
| No follow-up | 15 | 2 | 15,450 | 0.97 | 9.3 (4.6–18.2) | 97 | 9 | 27,801 | 3.49 | 11.4 (8.5–15.3) | .002 | |
| Cytology only | 20 | 12 | 120,419 | 0.17 | 1.6 (0.8–3.0) | 105 | 59 | 190,063 | 0.55 | 1.8 (1.4–2.4) | < .0001 | |
| Abnormal | 7 | 3 | 27,294 | 0.26 | 2.5 (1.0–5.6) | 48 | 9 | 30,539 | 1.57 | 5.1 (3.6–7.3) | < .0001 | |
| Normal | 13 | 10 | 93,126 | 0.14 | 1.3 (0.6–2.7) | 57 | 49 | 159,524 | 0.36 | 1.2 (0.8–1.6) | .006 | |
| Repeat 0–6 mo | 14 | 10 | 96,513 | 0.15 | 1.4 (0.7–2.8) | 96 | 50 | 162,291 | 0.59 | 1.9 (1.4–2.6) | < .0001 | |
| Repeat 7–25 mo | 6 | 2 | 23,906 | 0.25 | 2.4 (0.9–5.7) | 9 | 8 | 27,771 | 0.32 | 1.1 (0.5–2.0) | .776 | |
| ASCUS | Histology | 13 | 13 | 76,947 | 0.17 | Ref. | 39 | 39 | 127,275 | 0.31 | Ref. | |
| No follow-up | 7 | 1 | 8194 | 0.85 | 5.1 (1.9–12.4) | 49 | 5 | 16,519 | 2.97 | 9.8 (6.4–15.0) | .039 | |
| Cytology only | 10 | 9 | 54,475 | 0.18 | 1.1 (0.5–2.5) | 56 | 31 | 98,304 | 0.57 | 1.9 (1.3–2.8) | .0004 | |
| Abnormal | 3 | 2 | 10,572 | 0.28 | 1.7 (0.4–5.3) | 26 | 4 | 12,521 | 2.08 | 6.8 (4.1–11.0) | .002 | |
| Normal | 7 | 7 | 43,903 | 0.16 | 1.0 (0.4–2.3) | 30 | 27 | 85,782 | 0.35 | 1.1 (0.7–1.8) | .101 | |
| Repeat 0–6 mo | 8 | 7 | 44,766 | 0.18 | 1.1 (0.4–2.5) | 53 | 26 | 84,862 | 0.62 | 2.1 (1.4–3.1) | .0005 | |
| Repeat 7–25 mo | 2 | 2 | 9709 | 0.21 | 1.2 (0.2–4.5) | 3 | 4 | 13,442 | 0.22 | 0.7 (0.2–2.0) | .918 | |
| LSIL | Histology | 6 | 6 | 104,494 | 0.06 | Ref. | 45 | 45 | 145,910 | 0.31 | 1.0 | |
| No follow-up | 8 | 0 | 7256 | 1.10 | 19.2 (6.7–58.2) | 48 | 4 | 11,282 | 4.25 | 13.7 (9.1–20.7) | .016 | |
| Cytology only | 10 | 4 | 65,944 | 0.15 | 2.6 (1.0–7.8) | 49 | 28 | 91,759 | 0.53 | 1.7 (1.1–2.6) | .0007 | |
| Abnormal | 4 | 1 | 16,722 | 0.24 | 4.2 (1.1–14.7) | 22 | 6 | 18,017 | 1.22 | 4.0 (2.3–6.5) | .006 | |
| Normal | 6 | 3 | 49,223 | 0.12 | 2.1 (0.7–6.8) | 27 | 23 | 73,742 | 0.37 | 1.2 (0.7–1.9) | .024 | |
| Repeat 0–6 mo | 6 | 3 | 51,747 | 0.12 | 2.0 (0.6–6.5) | 43 | 24 | 77,430 | 0.56 | 1.8 (1.2–2.7) | .005 | |
| Repeat 7–25 mo | 4 | 1 | 14,197 | 0.28 | 4.9 (1.3–17.2) | 6 | 4 | 14,329 | 0.42 | 1.4 (0.5–3.0) | .607 | |
For young women diagnosed with low-grade squamous intraepithelial lesion, the incidence rate ratio for assessment with cytology only was weakly associated with an increased risk for subsequent cancer overall, but this risk increase was derived from the group with repeat cytology only after 7–25 months (incidence rate ratio, 4.9, 95% confidence interval, 1.3–17.2), whereas the risk did not differ significantly from the assessment with histology if the repeat cytology was registered within 6 months (incidence rate ratio, 2.0, 95% confidence interval, 0.6–6.5). Young women with no morphology after a low-grade squamous intraepithelial lesion smear were at greatly increased risk (19-fold) for incident cancer ( Table 3 ).
For women aged 28–50 years, the incidence rates for incident cancer were higher than in younger women, with similar rates after different further assessment options, regardless of whether having received an atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion diagnosis in the index cytology ( Table 2 ).
Compared with women assessed with histology, the risk of incident cancer was doubled among older women with repeat cytology within 6 months of the index diagnosis. Similar to younger women, women aged 28–50 years who did not have any morphology after the index diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion were at greatly elevated risk ( Table 3 ).
Compared with women with normal index cytology, risks for incident cancer after an atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion diagnosis were consistently elevated across age groups and further assessment options, with incidence rate ratios following the same pattern as described above ( Supplemental Table 2 ). When results were stratified by decade of follow-up/diagnosis (1989–1999 and 2000–2011, respectively), there were no major differences according to time period in terms of baseline incidence rates, incidence rate ratios, or risks for incident cancer by further assessment option, although there were slight variations in some estimates because of smaller numbers ( Supplemental Tables 3 and 4 ).
Finally, a cut point for repeat cytology of 12 months instead of 6 months was investigated in women aged 22–27 years. Whereas a time window of 0–6 months was not associated with a statistically significantly increased risk for incident cancer (incidence rate ratio, 2.0, 95% confidence interval, 0.6–6.5), a time window for repeat cytology of 7–12 months’ assessment was found to result in statistically significantly increased risks for cancer in younger women after low-grade squamous intraepithelial lesion compared with those with further assessment with histology (incidence rate ratio, 5.3, 95% confidence interval, 1.1–20.0, Supplemental Table 5 ).
Among women aged 22–27 years with atypical squamous cells of undetermined significance/low-grade squamous intraepithelial lesion in 2010, a total of 5139 women had a repeat cytology, without any preceding biopsy procedure, within 6 months from the index smear. Of these, a total of 1391 women (27%) had their repeat cytology diagnosed as normal ( Table 4 ).
| Cytology | Age 22–27 y | Age 28–50 y | ||
|---|---|---|---|---|
| ASCUS | LSIL | ASCUS | LSIL | |
| Total number | 2887 | 2252 | 4541 | 2407 |
| Within 6 mo a | ||||
| No repeat cytology, n, % | 956 (33.1) | 827 (36.7) | 1892 (41.7) | 903 (37.5) |
| Repeat normal cytology, n, % | 900 (31.2) | 491 (21.8) | 1540 (33.9) | 559 (23.2) |
| Repeat abnormal cytology, n, % | 1031 (35.7) | 934 (41.5) | 1109 (24.4) | 945 (39.3) |
a Numbers presented indicate only repeated cytology without biopsy before repeated smear.
Results
In total, we included 2,466,671 women with a median follow-up of 9.9 years. During the study, 2,415,269 of these women had ≥1 normal cytology registered. Of these, 190,977 women received a first cytological diagnosis of atypical squamous cells of undetermined significance or low-grade squamous intraepithelial lesion during the study period, 71,449 of which were aged 22-27 years at the index cytology and 119,528 of which were aged 28-50 years at the index cytology ( Table 1 ).
| Characteristics | Normal a | ASCUS/LSIL, younger | ASCUS/LSIL, older |
|---|---|---|---|
| Participants, n | 2,415,269 | 71,449 | 119,528 |
| Diagnosis of cytology | |||
| ASCUS | 0 | 33,764 (47.3) | 63,009 (52.7) |
| LSIL | 0 | 37,685 (52.7) | 56,519 (47.3) |
| Age at entry | |||
| 22–24 | 768,773 (27.4) | 40,767 (57.1) | — |
| 25–27 | 287,710 (10.3) | 30,682 (42.9) | — |
| 28–30 | 261,751 (9.3) | — | 23,624 (19.8) |
| 31–35 | 408,897 (14.6) | — | 29,566 (24.7) |
| 36–40 | 385,374 (13.7) | — | 22,887 (19.2) |
| 41–45 | 381,949 (13.6) | — | 22,237 (18.6) |
| 46–50 | 315,791 (11.2) | — | 21,214 (7.4) |
| Calendar periods at entry | |||
| 1989–1994 | 1,258,897 (44.8) | 13,241 (18.5) | 24,728 (20.7) |
| 1995–2000 | 621,311 (22.1) | 15,176 (21.2) | 31,205 (26.1) |
| 2001–2006 | 478,013 (17.0) | 19,070 (26.7) | 31,655 (26.5) |
| 2007–2011 | 452,024 (16.1) | 23,962 (33.5) | 31,940 (26.7) |
a Women were considered to be unexposed for 5 years after each normal cytology. Therefore, one woman could contribute multiple normal periods to the normal group.
Among these 2 groups, 68,417 younger and 112,744 older women, respectively, were eligible for the analysis of further assessment ( Figure 2 ). In total, 222 invasive cancers occurred within 0–6.5 years in women aged 22–27 years: 151 squamous cell carcinomas (68%), 49 adenocarcinomas (22%), and 22 tumors of other histological type such as adenosquamous carcinomas (10%). Among women aged 28–50 years, 715 cancers occurred within 0–6.5 years: 504 squamous cell carcinomas (70.5%), 172 adenocarcinomas (24%), and 39 of other histological type such as adenosquamous carcinomas (5.5%).




