Background
Intrapericardial teratoma is a rare, lethal tumor often detected in fetal life. Tumor mass and pericardial effusion cause cardiac tamponade that, if relieved, could be life-saving. Optimal timing of intervention and methods for effective fetal treatment are unknown.
Objective
We describe our single-center experience with fetal intrapericardial teratoma including the first report of successful in utero surgical resection with survival to term.
Study Design
We reviewed our database for suspected fetal intrapericardial teratoma. On fetal ultrasound and echocardiography tumor size was estimated by calculation of an ellipse and analyzed in relation to Doppler-derived fetal cardiac output, venous flow patterns, hydrops, and outcome.
Results
Eight fetuses with suspected intrapericardial teratoma were seen from 2009 through 2015. Gestational age at initial presentation ranged from 21-34 (median 26) weeks. Two cases mimicked the appearance of intrapericardial teratoma, but had no serial change in cardiac output over time and were ultimately determined to be other types of tumor. In 6 cases of true intrapericardial teratoma, tumor growth was extremely rapid and associated with progressive decline in cardiac output (to <400 mL/kg/min) manifesting in hydrops and death if left untreated. One case was treated successfully at 31 weeks through ex utero intrapartum delivery with tumor resection while on placental support. Another case underwent open fetal surgery and resection at 24 weeks, with resumption of gestation until delivery at 37 weeks with excellent outcome.
Conclusion
Fetal intrapericardial teratoma can be successfully managed utilizing serial surveillance and by treatment in a timely manner prior to the predictable onset of hydrops, determined through increasing tumor size and a declining cardiac output. Surgical resection in utero is possible, with good results.
Click Video under article title in Contents at ajog.org
Introduction
Teratoma arising from the pericardium is an extremely rare tumor composed of endodermal, mesodermal, and ectodermal germinal cell lines. Treatment is readily achieved through surgical resection with low incidence of recurrence. However, when intrapericardial teratoma is detected in fetal life, mortality is high. Tumor size can be large and associated with pericardial effusion, the combination of which leads to progressive constraint of filling, cardiac tamponade, fetal hydrops, and death.
Treatment of fetal intrapericardial teratoma before birth is a challenge. To date, management most often includes observation with temporizing measures of pericardial fluid drainage or delivery, once the fetus reaches a viable gestational age for postnatal surgical resection. Prenatal resection, if possible, would be an ideal means of treatment. Open fetal surgery for resection of lung lesions is feasible with good results, when performed for impending hydrops prior to onset of severe hemodynamic compromise. A previous attempt at removal of a intrapericardial teratoma in a hydropic fetus did not result in survival. Markers characterizing the course and predicting in utero deterioration would be helpful in guidance and timing of effective treatment strategies.
The aims of this study are to report our experience with fetal intrapericardial teratoma, offer insight into monitoring by fetal echocardiography, and report on the application of innovative treatment strategies to deal with this lethal condition, including successful in utero surgical resection.
Materials and Methods
The database at the Fetal Heart Program and Center for Fetal Diagnosis and Treatment at the Children’s Hospital of Philadelphia was searched. The diagnosis of intrapericardial teratoma was suspected through ultrasound assessment when a large, irregularly shaped mass of heterogeneous echo-texture appeared to arise from outside of the cardiac chambers and from within the pericardial sac lining. Intrapericardial teratoma is defined as a teratoma arising from within the pericardial sac, with parietal pericardium covering, to be distinguished from other masses such as mediastinal teratoma, or other lung lesions, which may share similar physiological consequences but by nature may have a different course and prognosis. Obstetrical ultrasound, fetal echocardiography, and clinical course were reviewed for each case along with pathology data.
All patients underwent detailed obstetrical ultrasound and fetal echocardiography. Notation was made of presence of fluid in body cavities. Fetal hydrops was defined as significant fluid accumulation in ≥2 locations, and in at least 1 additional space besides the pericardium such as ascites, scalp edema, abdominal wall edema, or skin edema. Tumor location was characterized and dimensions measured. As tumor shape was irregular but mostly round or oval, estimate of size was obtained by measuring orthogonal maximum length and maximum width and calculating the area of an ellipse [area (cm 2 ) = 3.14 × ½ maximum long axis diameter × ½ maximum short axis diameter].
Doppler echocardiography was performed and tracings were obtained in the ductus venosus (DV) and umbilical vein (UV) as measures reflecting impediment to forward venous flow. Abnormal DV flow pattern was defined as near absent or reversed flow with atrial contraction; abnormal UV flow pattern was defined as presence of venous pulsations. Cardiac output was estimated for right and left ventricle by pulsed-wave Doppler interrogation across the pulmonic and aortic valves, respectively, using the formula: flow = [3.14 × semilunar valve radius 2 × velocity-time integral × heart rate]/estimated weight in kilograms. Normal combined right and left cardiac output in the fetus is 400-500 mL/kg/min.
Quantitative data are described as range (median) values. Pearson correlation coefficient was used to assess relationship of tumor size to cardiac output.
Materials and Methods
The database at the Fetal Heart Program and Center for Fetal Diagnosis and Treatment at the Children’s Hospital of Philadelphia was searched. The diagnosis of intrapericardial teratoma was suspected through ultrasound assessment when a large, irregularly shaped mass of heterogeneous echo-texture appeared to arise from outside of the cardiac chambers and from within the pericardial sac lining. Intrapericardial teratoma is defined as a teratoma arising from within the pericardial sac, with parietal pericardium covering, to be distinguished from other masses such as mediastinal teratoma, or other lung lesions, which may share similar physiological consequences but by nature may have a different course and prognosis. Obstetrical ultrasound, fetal echocardiography, and clinical course were reviewed for each case along with pathology data.
All patients underwent detailed obstetrical ultrasound and fetal echocardiography. Notation was made of presence of fluid in body cavities. Fetal hydrops was defined as significant fluid accumulation in ≥2 locations, and in at least 1 additional space besides the pericardium such as ascites, scalp edema, abdominal wall edema, or skin edema. Tumor location was characterized and dimensions measured. As tumor shape was irregular but mostly round or oval, estimate of size was obtained by measuring orthogonal maximum length and maximum width and calculating the area of an ellipse [area (cm 2 ) = 3.14 × ½ maximum long axis diameter × ½ maximum short axis diameter].
Doppler echocardiography was performed and tracings were obtained in the ductus venosus (DV) and umbilical vein (UV) as measures reflecting impediment to forward venous flow. Abnormal DV flow pattern was defined as near absent or reversed flow with atrial contraction; abnormal UV flow pattern was defined as presence of venous pulsations. Cardiac output was estimated for right and left ventricle by pulsed-wave Doppler interrogation across the pulmonic and aortic valves, respectively, using the formula: flow = [3.14 × semilunar valve radius 2 × velocity-time integral × heart rate]/estimated weight in kilograms. Normal combined right and left cardiac output in the fetus is 400-500 mL/kg/min.
Quantitative data are described as range (median) values. Pearson correlation coefficient was used to assess relationship of tumor size to cardiac output.
Results
From 2009 through 2015, 8 cases of suspected fetal intrapericardial teratoma were identified ( Table ). Gestational age at initial presentation ranged from 21-34 (median 26) weeks. Serial fetal evaluations with ≥2 assessments were made in 5 patients; only 1 evaluation was performed in each of 3 patients (cases 2, 7, 8) presenting with severe hydrops.
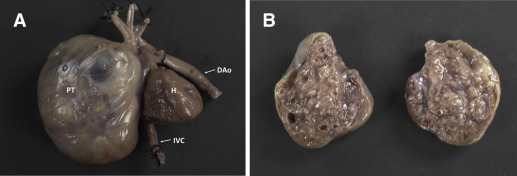
All cases had moderate to large circumferential pericardial effusion at initial presentation. In 7 cases, tumor mass appeared to compress the right atrium and impair filling of the right ventricle. In one (case 5), the tumor appeared to arise from the pericardium adjacent to the left atrium, extending leftward and cephalad into the upper mediastinum. Pathology diagnosis confirmed mature teratoma with multiple germinal cell lines in 6 of 8 patients. The masses in cases 5 and 6 mimicked the fetal echocardiographic appearance of intrapericardial teratoma by exhibiting characteristics of irregular shape, and heterogeneous echotexture, however on postnatal pathology were determined to be an ascending aortic teratoma and an intracardiac atrial hemangioma, respectively.
Clinical course, management strategies, and outcomes
Case 1 presented at 22 weeks’ gestation in a 27-year-old woman with morbid obesity, hypertension, and gestational diabetes. A rapidly progressive increase in tumor size was noted, with a large cystic component. At 26 weeks’ gestation, fetal pericardiocentesis was performed and 4 mL of serous fluid removed. Tumor growth continued unabated, with onset of hydrops at 28 weeks and fetal demise at 30 weeks ( Figure 1 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


