Background
Studies on the influence of body mass index, smoking, and mode of delivery on the occurrence of urinary incontinence after hysterectomy are required to provide women with information about how these factors influence continence after a hysterectomy.
Objective
The aim was to assess the impact of lifestyle factors such as body mass index, smoking, and delivery mode (vaginal/cesarean) on the incidence and remission of urinary incontinence after hysterectomy.
Study Design
This was a cohort study based on pre-, per-, and postoperative (1 year) data retrieved from the Swedish National Register for Gynecological Surgery on 16,182 hysterectomies performed because of a benign indication between 2006 and 2013. Multivariable logistic regression analyses were used to identify independent risk factors for de novo urinary incontinence and postoperative remission of urinary incontinence, presented as adjusted odds ratios with 95% confidence intervals.
Results
De novo urinary incontinence was reported by 8.5%, remission of urinary incontinence by 13.3%, and residual urinary incontinence by 16.1% after the hysterectomy. A body mass index ≥30 kg/m 2 (odds ratio, 1.63, 95% confidence interval, 1.37–1.94), having undergone a vaginal delivery (odds ratio, 1.40, 95% confidence interval, 1.14–1.86), the presence of daily urge without incontinence prior to surgery (odds ratio, 1.77, 95% confidence interval, 1.47–2.13), and a uterine weight <500 g (odds ratio, 2.46, 95% confidence interval, 1.96–3.09) were associated with an increased risk of de novo urinary incontinence. A uterine weight >300 g (odds ratio, 1.98, 95% confidence interval, 1.69–2.33), body mass index <25 kg/m 2 (odds ratio, 1.22, 95% confidence interval, 1.01–1.47), prolapse (odds ratio, 2.25, 95% confidence interval, 1.60–3.18), or fibroids (odds ratio, 1.33, 95% confidence interval, 1.09–1.62) as indication for surgery and the absence of daily urge without incontinence preoperatively (odds ratio, 1.51, 95% confidence interval, 1.29–1.76) were associated with an increased remission of urinary incontinence. Vaginal compared with abdominal hysterectomy was associated with a decreased remission of urinary incontinence (odds ratio, 0.70, 95% confidence interval, 0.57–0.87). There was no effect of age or smoking or a difference between total and subtotal hysterectomy with regard to de novo urinary incontinence or remission of urinary incontinence after the hysterectomy. Residual urinary incontinence and de novo urinary incontinence significantly reduced satisfaction with surgery 1 year postoperatively compared with women without urinary incontinence.
Conclusion
Vaginal delivery, obesity, and daily urge symptoms without incontinence prior to surgery increased de novo urinary incontinence and had a negative influence on the rate of remission of urinary incontinence after hysterectomy, which in turn influenced patients’ satisfaction with surgery.
Even though the proportion of women undergoing hysterectomy has decreased in recent years, millions of otherwise healthy women throughout the world undergo hysterectomy each year. Urinary incontinence has been linked to prior hysterectomy, but studies show varying results regarding the association between the type of hysterectomy and urinary incontinence. In several studies vaginal hysterectomy has been associated with stress urinary incontinence and subsequent stress urinary incontinence surgery.
Divergent data have been published regarding the risk of urinary incontinence in women undergoing subtotal compared with total hysterectomy, and a Cochrane review comparing subtotal and total hysterectomy could not find evidence to support subtotal hysterectomy. Hysterectomy has also been reported to cause remission of urinary incontinence. Thus, this demonstrates the complexity of informing women undergoing hysterectomy about the risks of urinary incontinence.
Age, obstetric trauma, and obesity are known to be 3 of the most important risk factors for urinary incontinence and may also affect the association between urinary incontinence and hysterectomy. It has been debated whether smoking has a causal effect on urinary incontinence, but smoking is known to increase postoperative complications following surgery. The lifestyle factors of high body mass index and smoking are potentially modifiable factors preoperatively.
Studies regarding the influence of life style factors and mode of delivery are required to provide women undergoing hysterectomy with information about how these factors influence continence after a hysterectomy. The aim of this study was to evaluate the influence of mode of delivery, body mass index, and smoking on the incidence and remission of urinary incontinence after different types of hysterectomy while accounting for other variables that may influence urinary incontinence based on a logistic regression model.
Material and Methods
Data were collected from the Swedish National Register for Gynecological Surgery ( http://www.gynop.org ) in women who underwent hysterectomy for a benign reason between January 2006 and December 2013. Details about the hysterectomy register, consent, inclusion criteria, and patient characteristics have been published previously.
Data in the register were collected prospectively from patient questionnaires and doctors’ forms. Variables included in the analyses were age, body mass index, smoking status, parity, mode of delivery, hormonal status, comorbidities (eg, hypertension, diabetes), indication for surgery, hysterectomy route, urinary incontinence status pre- and postoperatively, symptoms of daily urinary urge, uterine size, and subtotal or total hysterectomy. Patient satisfaction with surgery and how the condition had improved after surgery was also analyzed. Preoperatively, the patient filled in a questionnaire including a health declaration and questions on subjective symptoms. Body height and weight were recorded and used for the calculation of body mass index.
The route of surgery was grouped by the primary incision into abdominal hysterectomy, laparoscopic hysterectomy, and vaginal hysterectomy. Subtotal or total hysterectomy was analyzed as separate variables. Patients with concomitant urinary incontinence or concomitant prolapse surgery were not included.
We also grouped the women according to mode of delivery defined as caesarean delivery only, at least 1 vaginal delivery, or nulliparous because previous studies have indicated that vaginal delivery compared with caesarean delivery increases the risk of urinary incontinence. Daily urinary urge symptoms were derived from the question, “Do you experience urge symptoms?”
Subjective symptoms of urinary incontinence were assessed by answers from the question, “Do you experience urinary leakage or involuntary emptying of the bladder?” Leakage 1–3 times/week or daily leakage was defined as urinary incontinence, and no troublesome urinary incontinence was defined by the following answers: no urinary leakage, almost never leakage, or 1–3 times per month.
A follow-up questionnaire was sent to the patient 8 weeks and 1 year after surgery, which was subsequently evaluated by the surgeon if there had been any short- or long-term complications or dissatisfaction with the result of the surgery. The same questions on urinary incontinence were used postoperatively for the assessment of urinary incontinence 1 year after hysterectomy. De novo urinary incontinence was defined if the woman had no urinary incontinence prior to hysterectomy but had a positive answer on the urinary incontinence questions in the 1 year follow-up questionnaire. The women with urinary incontinence preoperatively but who had no subjective urinary incontinence 1 year after surgery were defined as having had a remission of urinary incontinence.
Information on satisfaction with the procedure and how the condition was improved or not was obtained from the 1 year questionnaire. The answers from the question, “Are you satisfied with the result of the surgery,” were dichotomized into satisfied (very satisfied and satisfied) and not satisfied (neither satisfied nor unsatisfied, unsatisfied, and very unsatisfied). The responses to the patients condition after surgery were categorized into improved (much improved and improved), unchanged, and worsened (worsened or much worsened).
Ethical approval
Ethical approval was obtained from the Ethics Committee at Sahlgrenska Academy, Gothenburg University (061-13).
Statistical analyses
Categorical data were analyzed by a Pearson’s χ 2 or Fisher exact test. Continuous variables were analyzed using a Student t test or ANOVA. A value of P < .05 was considered to be statistically significant.
Previously reported risk factors for urinary incontinence were included in the logistic regression analysis for de novo urinary incontinence and remission of urinary incontinence: age, body mass index, smoking, mode of delivery, indication for surgery, comorbidities (hypertension and diabetes), type of hysterectomy (vaginal hysterectomy, laparoscopic hysterectomy, or abdominal hysterectomy), subtotal or total hysterectomy, uterine weight, and daily urge preoperatively. A stepwise approach was conducted to, one by one, exclude the variables demonstrated to be nonsignificant in multiple testing. Adjusted odds ratio and the 95% confidence interval were calculated.
Prior to conducting the logistic regression analysis, some of the independent variables were transformed. Body mass index was grouped according to the World Health Organization classification (underweight, <18.5 kg/m 2 ; normal, 18.5–24 kg/m 2 ; overweight, 25–29 kg/m 2 ; obesity I, 30–34 kg/m 2 ; and obesity II, >35 kg/m 2 ) and dichotomized into 3 groups; <25 kg/m 2 , 25–29.9 kg/m 2 , and ≥30 kg/m 2 .
Uterine weight was categorized into the following 3 weight groups: <300 g, 300–500 g, and >500 g. This classification was based on the findings that minimal invasive hysterectomy techniques are recommended and associated with less complications for a uterus size similar to <12–14 gestational weeks, which corresponds to a weight of 250–280 g.
Based on information about smoking in the health declaration, the participants were classified as smoker or nonsmoker (includes former smokers). All statistical analyses were performed using SPSS version 21 or 23 (SPSS Inc, Chicago, IL).
Results
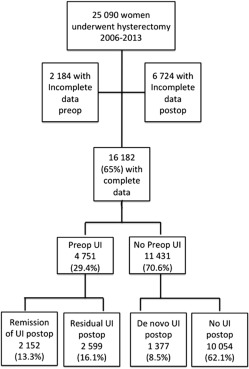
Of the 25,090 hysterectomized women between 2006 and 2013, a total of 16,182 women responded to both the preoperative and postoperative urinary incontinence questions ( Figure ). It was possible to perform an evaluation of the characteristics of the sample and analysis of the nonresponders.
The women who did not answer the questions on urinary incontinence preoperatively were younger (43.7 years vs 50.6 years), had less often had a vaginal delivery (60.7% vs 70.1%), smoked to a higher extent (23% vs 17%), had more often an abdominal hysterectomy (64% vs 57%) or subtotal hysterectomy (16% vs 14%), and had a lower uterine weight compared with the women who had answered the questions. There was no difference between responders and nonresponders regarding body mass index groups or the level of satisfaction with surgery.
When analyzing the group of women who had not responded to the urinary incontinence questions postoperatively, there was no difference in age or body mass index compared with the women who had responded. The women more often had a vaginal delivery (72.8% vs 67.9%), smoked to a greater extent (19.1% vs 17.3%), had more laparoscopic surgery (10.7% vs 6.4%), but less often subtotal hysterectomy (11.1% vs 14.9%).
The preoperative prevalence of urinary incontinence was 29.4%, and 75.4% of the cohort reported no urinary incontinence after surgery. 2152 women had a remission of urinary incontinence (13.3% of the total cohort), 8.5% developed de novo urinary incontinence and 16.1% women had unaltered, residual urinary incontinence ( Figure ). The majority of the women were premenopausal at the time of surgery and 75% of the women reported that they were still menstruating prior to surgery.
Women without preoperative urinary incontinence had lower parity, had been more often delivered by cesarean delivery only, or were nulliparous. They were also younger and had less comorbidities compared with the women with preoperative urinary incontinence. Prolapse and fibroids were more often the indication for hysterectomy, vaginal hysterectomy was more often performed, and uterine weight was more often >500 g among the women with preoperative urinary incontinence compared with the group with no preoperative urinary incontinence. Women with preoperative urinary incontinence were more frequently obese ( Table 1 ).
| No UI preoperatively, n, % (n = 11,431) (70.6) | UI preoperatively, n, % (n = 4751) (29.4) | P value | |
|---|---|---|---|
| Age mean [range] | 49.8 [22–91] | 52.7 [26–91] | < .001 |
| Parity mean [range] | 2.2 ± 1.2 [0–12] | 2.3 ± 1.1 [0–11] | < .001 |
| Estrogen substitution | 1251 (11.5) | 803 (17.5) | < .001 |
| Vaginal delivery ≥one | 7580 (83.8) | 3540 (93.3) | < .001 |
| Cesarean section only | 771 (8.5) | 179 (4.7) | |
| Nulliparous | 696 (7.7) | 77 (2.0) | |
| Diabetes | 370 (3.2) | 231 (4.9) | < .001 |
| Hypertension | 2346 (20.5) | 1248 (26.3) | < .001 |
| BMI, kg/m 2 (mean) | 25.9 | 26.7 | < .001 |
| <25 | 4837 (42.3) | 1600 (33.7) | < .001 |
| 25–29.9 | 4461 (39.0) | 1919 (40.4) | |
| ≥30 | 2133 (18.7) | 1232 (25.9) | |
| Smoker | 1971 (17.3) | 762 (16.0) | .061 |
| Daily urinary urge | 1653 (14.5) | 2045 (43.3) | < .001 |
| Main indication for surgery | |||
| Meno-/metrorrhagia | 3520 (30.8) | 1234 (29.9) | < .001 |
| Fibroids | 1977 (17.3) | 904 (21.9) | |
| Pain | 800 (7.0) | 250 (6.1) | |
| Prolapse | 1491 (13.0) | 1053 (25.5) | |
| Other | 1962 (17.2) | 687 (16.6) | |
| Type of hysterectomy | |||
| Abdominal | 6789 (59.4) | 2626 (55.3) | < .001 |
| Laparoscopic | 784 (6.9) | 256 (5.4) | |
| Vaginal | 3858 (33.8) | 1869 (39.3) | |
| Type of hysterectomy | |||
| Total | 1696 (14.8) | 662 (13.9) | .140 |
| Subtotal | 9735 (85.2) | 4089 (86.1) | |
| Uterine weight, g | |||
| <300 | 6459 (65.3) | 2207 (58.3) | < .001 |
| 300–500 | 1484 (15.0) | 600 (15.9) | |
| >500 | 1948 (19.7) | 976 (25.8) |
The group of women who developed de novo urinary incontinence (n = 1377) more often had undergone a vaginal delivery, were to a higher extent obese, had a lower uterine weight, had more daily urinary urge preoperatively, and were less satisfied with the result of surgery compared with the women with no urinary incontinence pre- and postoperatively. The proportion of women reporting de novo urinary incontinence and women with no urinary incontinence pre- and postoperatively did not differ between the different types of hysterectomy ( Table 2 ).
| De novo UI postop (n = 1377), n, % | No UI postop (n =10,054), n, % | P value | |
|---|---|---|---|
| Age mean [range] | 49.7 [24–87] | 49.9 [22–91] | .53 |
| Parity mean [range] | 2.3 [0–12] | 2.2 [0–11] | .019 |
| Estrogen substitution | 168 (12.8) | 1083 (11.3) | .47 |
| Vaginal delivery ≥1 | 984 (87.7) | 6596 (83.2) | < .001 |
| Cesarean delivery only | 82 (7.3) | 689 (8.7) | |
| Nulliparous | 56 (5.0) | 640 (8.1) | |
| Diabetes | 52 (3.8) | 318 (3.2) | .228 |
| Hypertension | 290 (21.1) | 2056 (20.4) | .599 |
| BMI (mean), kg/m 2 | 26.9 | 25.9 | < .001 |
| <25 | 486 (35.3) | 4351 (43.3) | < .001 |
| 25–29.9 | 548 (39.8) | 3913 (38.9) | |
| ≥30 | 343 (24.9) | 1790 (17.8) | |
| Smoker | 259 (18.8) | 1713 (17.0) | .103 |
| Daily urinary urge | 253 (18.7) | 1400 (14.1) | < .001 |
| Main indication for surgery | |||
| Meno-/metrorrhagia | 469 (39.8) | 3051 (35.6) | < .001 |
| Fibroids | 183 (15.5) | 1794 (20.9) | |
| Pain | 117 (9.9) | 683 (8.0) | |
| Prolapse | 155 (13.2) | 1336 (15.6) | |
| Other | 253 (21.5) | 1709 (19.9) | |
| Type of hysterectomy | |||
| Abdominal | 797 (57.9) | 5992 (59.6) | .335 |
| Laparoscopic | 91 (6.6) | 693 (6.9) | |
| Vaginal | 489 (35.5) | 3369 (33.5) | |
| Type of hysterectomy | |||
| Total | 201 (14.6) | 1495 (14.9) | .789 |
| Subtotal | 1176 (85.4) | 8559 (85.1) | |
| Uterine weight | |||
| <300g | 912 (75.2) | 5547 (63.9) | < .001 |
| 300–500g | 171 (14.1) | 1313 (15.1) | |
| >500g | 130 (10.7) | 1818 (20.9) | |
| Postop 1 year | |||
| Improved | 934 (87.4) | 7032 (92.6) | < .001 |
| Unchanged | 84 (6.1) | 448 (5.9) | |
| Worsened | 50 (7.9) | 112 (1.1) | |
| Satisfied | 1136 (84.1) | 9195 (93.2) | < .001 |
| Neither nor | 155 (11.5) | 514 (5.2) | |
| Dissatisfied | 58 (4.3) | 146 (1.5) |
The highest rate of de novo urinary incontinence was recorded in the group of women with a body mass index ≥30 kg/m 2 and after vaginal delivery ( P < .001) ( Table 3 ). Delivery mode, uterine weight, body mass index class, and preoperative daily urge were found to be predictors for de novo urinary incontinence in the multivariable regression analysis ( Table 4 ).
| BMI group and outcome | Vaginal delivery ≥1 | Cesarean delivery Only | Nulliparous | P value |
|---|---|---|---|---|
| <25 kg/m 2 | ||||
| De novo UI | 356 (11.4) | 24 (8.0) | 23 (7.1) | .02 |
| 25–29.9 kg/m 2 | ||||
| De novo UI | 387 (12.6) | 37 (13.0) | 17 (7.2) | .04 |
| >30 kg/m 2 | ||||
| De novo UI | 241 (17.3) | 21 (11.2) | 16 (11.6) | .03 |
| P value | < .001 | .14 | .25 | |
| <25 kg/m 2 | ||||
| Remission of UI | 565 (48.6) | 25 (52.1) | 33 (58.9) | .17 |
| 25–29.9 kg/m 2 | ||||
| Remission of UI | 622 (43.9) | 33 (46.5) | 28 (50.0) | .61 |
| >30 kg/m 2 | ||||
| Remission of UI | 357 (38.9) | 33 (55.0) | 30 (53.6) | .01 |
| P value | .001 | .59 | .66 |
| Variable | Crude OR (95% CI) | Adj OR (95% CI) |
|---|---|---|
| Body mass index, kg/m 2 | ||
| <25 | 1 | 1 |
| 25–29.9 | 1.25 (1.10–1.43) | 1.12 (0.96–1.31) |
| ≥30 | 1.72 (1.48–1.99) | 1.63 (1.37–1.94) |
| No daily urge preoperatively | 1 | 1 |
| Daily urge preoperatively | 1.41 (1.21–1.63) | 1.77 (1.47–2.13) |
| Uterine weight, g | ||
| <300 | 2.29 (1.90–2.78) | 2.60 (2.07–3.28) |
| 300–500 | 1.82 (1.43–2.31) | 1.93 (1.45–2.55) |
| >500 | 1 | 1 |
| Cesarean delivery | 1 | 1 |
| Nulliparous | 0.74 (0.52–1.05) | 0.93 (0.63–1.36) |
| Vaginal delivery ≥1 | 1.25 (0.99–1.59) | 1.40 (1.14–1.86) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


