Facial Trauma
Paul N. Manson
Craig A. Vander Kolk
Craig DuFresne
Johns Hopkins Out-patient Center, Baltimore, Maryland 21205.
Johns Hopkins Out-patient Center, Baltimore, Maryland 21205.
Aesthetic, Plastic and Reconstructive Surgery, Chevy Chase, Maryland 20815.
Aesthetic, Plastic and Reconstructive Surgery, Chevy Chase, Maryland 20815.
Facial fractures are uncommon in children younger than 5 years of age (1,2). They begin to resemble those of adults in pattern, frequency, mechanism, and treatment at puberty (3). Children are exposed to a different spectrum of injury mechanisms and forces (4,5,6). In general, smaller traumatic forces are involved than are seen in adults.
The basic principles of management of facial trauma in children differ from those in adults in the potential influence of injury and treatment on growth and development; the different patterns of facial skeletal injuries in children; the anatomic, physiologic, and psychological factors related to the various periods of childhood; the presence of tooth buds; and the marked potential for restitutional remodeling in children (7,8,9,10,11,12,13). Special considerations relate to difficulties with obtaining an adequate history, performing a thorough physical examination, and enlisting cooperation, and with the developing nature of physical structures and the rapidity of healing (13,14,15,16,17).
Posttraumatic facial deformities in children may result from injuries to bone or soft-tissue structures, uncorrected displacement of structures, or arrested development. Although most children grow and develop normally after injury (18), developmental malformations in adolescents and adults are occasionally the result of early trauma (19,20,21). Therefore, the parents of injured children must be informed that asymmetric or incomplete development or growth may occur, especially if an injury involves the nasomaxillary complex (22) or the mandibular condyles at an early age (23,24).
POSTNATAL GROWTH OF THE FACE
The early growth of the face is rapid (18). The face reaches 40% of adult size at 3 months of age, 70% at 2 years of age, and 80% at 5.5 years of age. The proportions of the face change dramatically during growth (15,16). At birth, the skull demonstrates a relatively large cranium and a smaller facial component. The ratio of the skull to the face is 8:1 at birth, 4:1 at 5 years of age, and 2:1 in adulthood. These changes are attributed to growth of the facial complex and modification of facial proportions (15). Facial proportions also differ with regard to sex and genetic heritage. In infants, the frontal lobes are large and the forehead is high and protrusive. Children’s heads are proportionately much larger than those of adults. This heavier head mass may explain in part the high frequency of head injuries, especially involving the frontal bone. The frontal skull forms a prominent portion of the protuberant area of the face, making it susceptible to trauma (15).
Half the postnatal increase in brain volume occurs during the first year of life, and the brain attains 75% of its adult size by 2 years of age. Compared with adults, the brain case seems disproportionately large, even in children 7 to 8 years of age. Growth of the brain case and face progresses through rapid and slow periods rather than as a steady progression.
The facial skeleton contains cavities for the eyes, nose, and mouth. In the infant facial skeleton, the nasal cavity is small, the perinasal sinuses are almost absent, and the mouth is small. The lower jaw is often diminutive. The nose and sinuses are essentially a single structure in infants, but the sinuses then increase in size, starting with the ethmoid and maxillary sinuses, which begin to develop from the nasal cavity during the latter part of pregnancy. The growth of the maxillary sinuses parallels that of the face. The maxillary sinuses are narrow in newborns and do not reach the level of the orbit. The floor of the maxillary sinuses does not reach the level of the floor of the piriform aperture until at least 7 years of age. It extends below the level of the floor of the nose only after the eruption of the permanent dentition and the increased development of the alveolar process of the maxilla. The maxillary sinuses are not fully developed until 16 years of age; as the sinuses
develop, they permit growth of the orbit and fractures of the orbital floor.
develop, they permit growth of the orbit and fractures of the orbital floor.
 FIGURE 23-1. The relative dimensions of the various portions of the face are seen in these skulls, which range in age from infancy to adulthood. |
The frontal sinus develops as an evagination from the nasal cavity and the ethmoid during the latter portion of pregnancy, and cannot be distinguished from the ethmoid sinuses until after 5 years of age. The frontal sinuses are usually asymmetric; vary greatly in size, shape, and septation; and grow slowly and reach adult size only in late puberty.
The frontal cranium, in contrast, has a major growth increase within the first 2 years of life. The first 6 months of life are characterized by a period of rapid growth. A period of slower growth follows from 6 months to 4 years of age. An increase in the vertical dimension of the face results from the development and eruption of the dentition and the growth of the sinuses (18). Rapid growth in the face occurs between 4 and 7 years of age; a slower period of growth extends from 9 to 15 years of age. A final period of rapid growth occurs from 15 to 19 years of age. The facial bones continue to grow until 21 years of age (Fig. 23-1).
Most facial growth is complete before puberty. The orbits attain adult size by 7 years of age. By 6 years of age, the palate and maxilla are two-thirds of adult size. In contrast, the nasal bones exhibit major growth during adolescence. The increase in facial height is greater in the middle third of the face than in the lower third. The increase in the anterior and posterior dimensions of the face is greater in the mandible than in the maxilla. The face often widens more in the mandibular area than in the maxillary region. From a surgical standpoint, growth of the nose may be considered relatively complete by 16 years of age (Fig. 23-1).
The mandible develops by condensation and proliferation from the first pharyngeal arch. It grows by development of the teeth and alveolar processes, and by growth of the bone. Further projection of the mandible is a consequence of growth in the ramus and condylar regions. The mandible is constantly undergoing remodeling, resorption, and deposition, with resultant changes in form and growth (25,26,27,28).
Growth in the condylar region is a result of endochondral ossification. The condyle is capped by a narrow zone of fibrovascular tissue that contains connective tissue cells and cartilage cells. The inner layer of this zone is chondrogenic and gives rise to hyaline cartilage cells that form the cartilaginous zone. Condylar cartilage differs from long-bone cartilage by virtue of the fibrous tissue cover. Trauma, particularly before the age of 5 years, may damage the fibrous tissue cover and result in hypoplasia of the mandible. Early trauma to the area of the condyle can result in overgrowth, undergrowth, or no disturbance in subsequent growth of the mandible.
Facial growth is controlled by a “functional matrix” (29,30,31,32) composed of the nonskeletal elements of the face, including spaces, muscles, soft tissue, and surrounding ligaments. The relation between trauma and the growth and development of the face remains unclear, although the septum has long been considered to be an important growth force in the midface (22,32,33), as has the condyle in the mandible (19,20,21,34,35). Damage to the septum and nasoethmoidal area during childhood can contribute to hypoplasia of the midface (32,36,37,38,39,40).
CLINICAL EXAMINATION
Clinical examination of a facial injury often reveals the pathology with surprising accuracy. The clinical examination of a child is often difficult. The patient frequently is unable or unwilling to provide a history. The parents may not be present or may not volunteer detailed information of use to the examining physician. The history should indicate the mechanism of injury and can provide clues to other areas that might have been injured.
Children frequently are uncooperative, and easily become frightened and apprehensive. Their fears and anxiety may be heightened by the presence of parents, who often unwittingly add to the confusion. The participation of parents is an individual choice of the examining physician and depends on the particular circumstances. The assessment of the patient demands individual consideration, patience, psychiatric education, and gentle but firm determination. Children should always be dealt with truthfully. Sedation may be considered if head injury observation is not indicated. In some cases, general anesthesia is required in children for examination and treatment of injuries that might be accomplished without such measures in adults.
Associated injuries in children are common (41,42). Skull fractures (35,43,44,45,46), brain injuries (14,47,48,49,50), and cervical spine injuries are common in patients with facial injuries. They should be suspected as “geographic
injuries” to the head and neck region. The subtle symptoms and signs of head injury can be masked by the emotional response to the accident, and the initial symptoms of cerebral compression are often anxiety and a subtle confusion.
injuries” to the head and neck region. The subtle symptoms and signs of head injury can be masked by the emotional response to the accident, and the initial symptoms of cerebral compression are often anxiety and a subtle confusion.
An orderly clinical examination should be initiated and progress through the face using the techniques of observation, palpation, and functional evaluation. Lacerations, contusions, and bruises are soft tissue injuries that identify specific areas of concern. A fracture or damage to deep soft tissue elements (e.g., nerves) may be present (Fig. 23-2). Palpation of all bony surfaces begins in the skull and forehead, and includes the rims of the orbits, the nose, and the zygomatic arches. The dentition should be assessed for tenderness or instability, fractured teeth, or mucosal lacerations. Signs such as tenderness, bone irregularity, step or level discrepancies in the alignment of teeth, crepitus, lacerations, or bleeding may be present. These provide clues to the presence of fractures. The surfaces of the mandible and maxilla are palpated both outside and inside the mouth. Intraoral lacerations, hematomas, and fractured, loose, or missing teeth provide clues to the presence of alveolar, mandibular, or maxillary fractures (1,51,52,53,54,55,56,57,58). Lateral pressure on the mandibular and maxillary dental arches determines instability or pain.
RADIOLOGIC EVALUATION
Radiographic evaluation of fractures in children is difficult and often requires sedation (59). Children’s bones are cancellous, and fractures are more difficult to observe on plain radiographs (59). Movement blurs the radiographs, further increasing the difficulty of interpretation. Plain films largely have been replaced by computed tomography (CT) scans (Fig. 23-3). The use of multiarray CT scanners allows the opportunity to have a three-dimensional construction of the bony structures. The one exception is the Panorex examination of the mandible (Fig. 23-4), which requires patient cooperation and is often unobtainable. In some cases, undisplaced fractures are difficult to delineate on CT scans or plain films, and these usually are the fractures that produce minimal symptoms. Suspected fractures may be treated without absolute radiographic confirmation.
Imaging studies such as CT scans may require sedation. The newer generation scanners can often take the required images in less than 5 to 10 seconds, thereby decreasing considerably the amount of sedation required. Care must be exercised in sedating patients with suspected brain injury. Early bone healing in children does not permit delay in diagnosis because treatment must be instituted. The clinician is challenged to achieve a rapid, accurate assessment, and to provide alignment and fixation of facial bones to minimize functional disturbances and maximize future growth potential and development.
AIRWAY MANAGEMENT IN CHILDREN
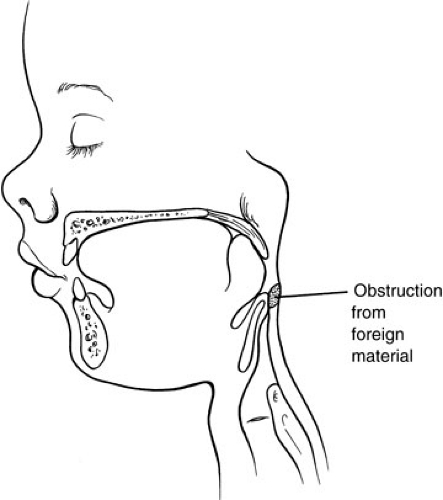
The pharynx and trachea in children are small and easily obstructed by blood, secretions, mucus, fractured teeth, or foreign objects (60,61,62,63,64) (Fig. 23-5). When the mandible is fractured bilaterally, it may fall backward, producing pharyngeal obstruction (Fig. 23-6). Forward traction on the mandible in these situations or use of the prone position can improve respiration. Usually, respiratory obstruction can be managed by orotracheal or nasotracheal intubation.
The endotracheal tubes used in children frequently are not “cuffed,” so a throat pack should be used to protect the respiratory tree from aspiration. The small size of the trachea makes obstruction a genuine concern after intubation. Specific attention to the humidification of inspired air, use of tracheal suction, and administration of mucolytic agents is required in the management of tracheostomies. Some surgeons believe that one-half of all children undergoing tracheostomies have related complications, most of which occur in patients younger than
5 years of age. Such complications include pneumothorax, emphysema, bleeding, infection, tracheal erosion or stenosis, occlusion of the cannula, displacement of the tube, and difficulty in decannulation. The prolonged use of an endotracheal tube allows the development of tracheal stenosis. Stenosis is minimized by attention to hygiene and positioning, and possibly by the use of stents and corticosteroids in appropriate patients. Radiographic studies of the airway can be used to identify patients with constriction of the tracheal lumen. Patients with identified tracheal narrowing are treated by endoscopic removal of granulation tissue, administration of corticosteroids, and placement of an endotracheal stent.
5 years of age. Such complications include pneumothorax, emphysema, bleeding, infection, tracheal erosion or stenosis, occlusion of the cannula, displacement of the tube, and difficulty in decannulation. The prolonged use of an endotracheal tube allows the development of tracheal stenosis. Stenosis is minimized by attention to hygiene and positioning, and possibly by the use of stents and corticosteroids in appropriate patients. Radiographic studies of the airway can be used to identify patients with constriction of the tracheal lumen. Patients with identified tracheal narrowing are treated by endoscopic removal of granulation tissue, administration of corticosteroids, and placement of an endotracheal stent.
 FIGURE 23-3. Multi array CT scan with a 3D reconstruction showing right orbital fractures. Note also arch bars in place. |
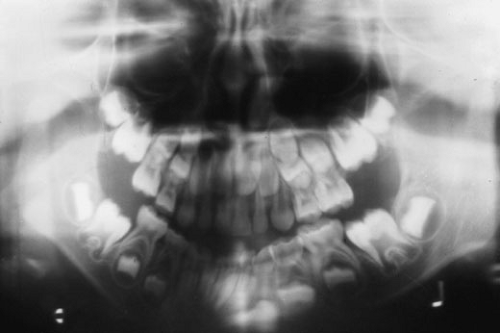 FIGURE 23-4. The Panorex examination allows visualization of the entire mandible. This examination usually requires that the patient be cooperative and able to sit upright safely. |
BLEEDING IN CHILDREN
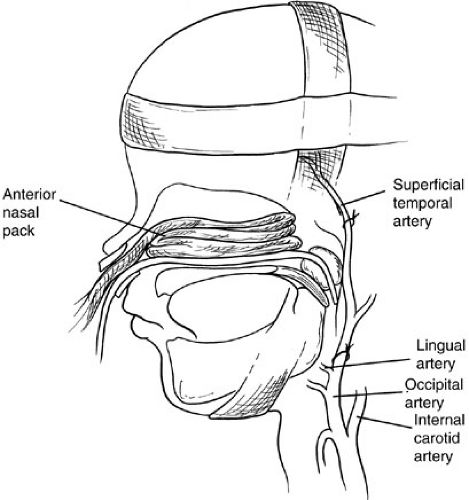
Hemorrhage accompanies most facial fractures, usually presenting through the nose and mouth. Hemorrhage tends to be most severe in fractures of the maxilla. It also can be profuse when the basal skull is fractured, lacerating the major dural veins or carotid artery. The blood volume in children is small, and circulatory compromise can occur rapidly. Profuse nasopharyngeal bleeding usually responds to anteroposterior nasal packing (Fig. 23-7). If it does not, manual reduction of the maxilla with maxillomandibular fixation usually rapidly improves nasopharyngeal bleeding from LeFort fractures. Sometimes, a soft compressive bandage wrapped around the face is helpful. Rarely, angiography is indicated and selective embolization or, even more rarely, ligation of the superficial temporal and external carotid artery on the affected side is necessary.
INCIDENCE OF FRACTURES IN CHILDREN
Children are protected from fractures by environmental and anatomic factors. As they grow, their environment
changes and so do the types of injuries and patterns of fractures. In general, the incidence of fractures is lower in children than adults because of the large cancellous structural ratio, which renders the bones relatively supple. The more solid structure of the maxilla in children, with the absent sinuses and the presence of developing dentition, changes the usual pattern of LeFort fractures. Once the sinuses develop, the pattern resembles that of adults. Young children are subject to falls in which the forces involved are much smaller than those sustained in the bicycle or automobile accidents that older children experience. The prominent forehead in young children is the area usually injured in a fall. Incomplete or “greenstick” fractures are relatively common in children because of the cancellous structure of the bone and its elasticity. The protruding frontal skull in young children serves to protect the face, which is smaller and relatively recessed (Fig. 23-8). In addition, the soft tissues in children are proportionately thick and padded by layers of fat, which also protect the bones from injury. Frontal skull and supraorbital fractures are common in young children, whereas fractures in the middle and lower facial areas are more common in older children. Because patterns of exposure to environmental factors change during childhood, it is appropriate to consider an age-grouped analysis of injury patterns.
changes and so do the types of injuries and patterns of fractures. In general, the incidence of fractures is lower in children than adults because of the large cancellous structural ratio, which renders the bones relatively supple. The more solid structure of the maxilla in children, with the absent sinuses and the presence of developing dentition, changes the usual pattern of LeFort fractures. Once the sinuses develop, the pattern resembles that of adults. Young children are subject to falls in which the forces involved are much smaller than those sustained in the bicycle or automobile accidents that older children experience. The prominent forehead in young children is the area usually injured in a fall. Incomplete or “greenstick” fractures are relatively common in children because of the cancellous structure of the bone and its elasticity. The protruding frontal skull in young children serves to protect the face, which is smaller and relatively recessed (Fig. 23-8). In addition, the soft tissues in children are proportionately thick and padded by layers of fat, which also protect the bones from injury. Frontal skull and supraorbital fractures are common in young children, whereas fractures in the middle and lower facial areas are more common in older children. Because patterns of exposure to environmental factors change during childhood, it is appropriate to consider an age-grouped analysis of injury patterns.
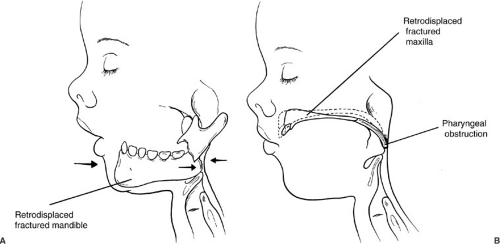 FIGURE 23-6. The mandible (A) or maxilla (B), if fractured and displaced posteriorly, can produce pharyngeal obstruction. |
PRENATAL AND BIRTH INJURIES
Skull Fracture and Hematoma
Intrauterine compression can cause some prenatal facial deformities. Birth injuries also can result in facial fractures (65,66). Prolonged labor, difficult passage through the birth canal and the use of obstetric forceps are known to induce certain injuries (e.g., nasal fractures, facial nerve or brachial plexus traction injuries) (67). Most injuries from obstetric forceps create hematomas over the skull; recovery usually occurs without residual problems, but patients must be observed for the development of a chronic cavity or the need for evacuation or aspiration. Infant skulls are pliable and their segmental arrangement, flexibility, resiliency, and softness contribute to a great tolerance to deformity and fracture. Skull fractures may be seen after forcible delivery or other birth injuries. Skull fractures may be suspected on the basis of a hematoma. A shallow groove may be present after resolution of the hematoma. An elliptic or round depression sometimes occurs posterior to the coronal suture. These injuries are “growing skull fractures” (Fig. 23-9) and should be diagnosed by serial radiographs (68,69). Children with skull fractures should be followed up with plain radiographs 1 year later, at which time growing skull fractures can be recognized easily as radiolucent areas. The components necessary to create a growing skull fracture include a skull fracture that is treated by closed reduction and a dural
laceration (which permits cerebral tissue to press on the bone edges, promoting resorption). Repair of the dura is usually all that is necessary because the bone often regenerates spontaneously in young patients.
laceration (which permits cerebral tissue to press on the bone edges, promoting resorption). Repair of the dura is usually all that is necessary because the bone often regenerates spontaneously in young patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree