Background
Vaginal delivery for the first birth is of great importance for further obstetric performance for the individual woman. Given the rising cesarean delivery rates worldwide over the past decades, a search for modifiable factors that are associated with cesarean delivery is needed. Exercise may be a modifiable factor that is associated with type of delivery, but the results of previous studies are not conclusive.
Objective
The purpose of this study was to investigate the association between exercise during pregnancy and cesarean delivery, both acute and elective, in nulliparous women.
Study Design
We conducted a population-based cohort study that involved 39,187 nulliparous women with a singleton pregnancy who were enrolled in the Norwegian Mother and Child Cohort Study between 2000 and 2009. All women answered 2 questionnaires in pregnancy weeks 17 and 30. Acute and elective cesarean delivery data were obtained from the Medical Birth Registry of Norway. Information on exercise frequency and type was assessed prospectively by questionnaires in pregnancy weeks 17 and 30. Generalized linear models estimated risk differences of acute and elective cesarean delivery for different frequencies and types of exercise during pregnancy weeks 17 and 30. We used restricted cubic splines to examine dose-response associations of exercise frequency and acute cesarean delivery. A test for nonlinearity was also conducted.
Results
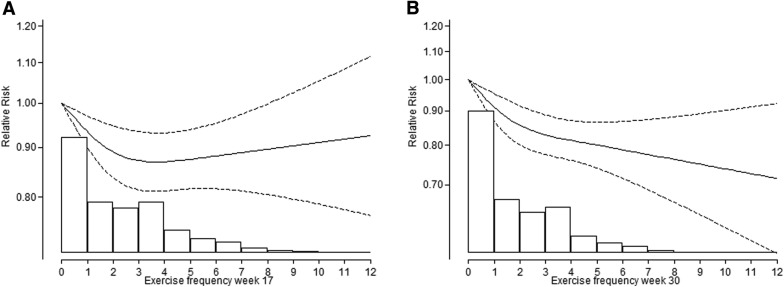
The total cesarean delivery rate was 15.4% (n=6030), of which 77.8% (n=4689) was acute cesarean delivery. Exercise during pregnancy was associated with a reduced risk of cesarean delivery, particularly for acute cesarean delivery. A nonlinear association was observed for exercise frequency in weeks 17 and 30 and risk of acute cesarean delivery (test for nonlinearity, P =.003 and P =.027, respectively). The largest risk reduction was observed for acute cesarean delivery among women who exercised >5 times weekly during weeks 17 (–2.2%) and 30 (–3.6%) compared with nonexercisers (test for trend, P <.001). Reporting high impact exercises in weeks 17 and 30 was associated with the greatest reduction in risk of acute cesarean delivery (–3.0% and –3.4%, respectively).
Conclusion
Compared with nonexercisers, regular exercise and high-impact exercises during pregnancy are associated with reduced risk of having an acute cesarean delivery in first-time mothers.
The rising rate of cesarean delivery (CD) in developed countries has been attributed partly to broadened medical indications and maternal request, such as fear of birth. Given the adverse effects of repeated cesarean deliveries, understanding factors that are associated with the decision to perform the first CD is vital.
Regular exercise during pregnancy is associated with a reduced risk of gestational diabetes mellitus, preeclampsia, and excessive birthweight, all of which are correlated highly with having a CD. Exercise during pregnancy may also influence the course of labor and mode of delivery by affecting metabolic and hormonal changes, uterine contractility, endurance, and strength. Results from both clinical and observational studies that have investigated the association between exercise during pregnancy and mode of delivery are inconclusive. However, existing studies are small, generally not population-based; some report unadjusted estimates, are not powered to study obstetric outcomes such as CD, or are unable to distinguish between elective and acute CD. Few studies have estimated the direct effect of pregnancy exercise at 2 different time points on the risk of CD.
Although randomized controlled trials are the most reliable method of determining the effect of pregnancy exercise on CD rates, it would require >900 participants in each group to detect a 5% difference in CD rate in a similar population. The feasibility of a randomized controlled trial with such sample size is, however, uncertain. Population-based observational studies that include women with varying exercise levels during pregnancy therefore may be useful. We used the Norwegian Mother and Child Cohort Study (MoBa), which is a large prospective population-based cohort in which data on various health topics and exposures were collected through questionnaires twice during pregnancy, to estimate the association between exercise during pregnancy and CD, both acute and elective, among nulliparous women who participated in the MoBa cohort. The MoBa dataset was also linked to records from the Medical Birth Registry of Norway (MBRN) to provide information about pregnancy, delivery, and birth outcomes.
Materials and Methods
MoBa is a prospective population-based pregnancy cohort study conducted by the Norwegian Institute of Public Health. More than 100,000 participants were recruited from all over Norway between 1999 and 2008, including both rural and urban areas. The study’s primary aim was to identify environmental and genetic factors that are associated with diseases in pregnancy and childhood. Methods and cohort characteristics have been reported elsewhere. The current study was based on the eighth version of the quality-assured data files that were released for research in April 2014. Informed consent was obtained from all participants before inclusion. The study was approved by the Regional Committees for Medical Research Ethics (S-95113) and The Norwegian Data Protection Authority.
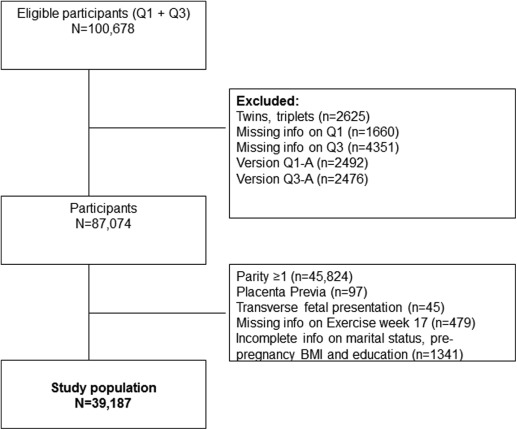
The target population in MoBa was all women in Norway who gave birth from 1999–2008. Fifty of 52 maternity units participated, and the total participation rate was approximately 44% of all invited pregnancies, with a follow-up rate of 93.6% in pregnancy week 30. Compared with nonparticipants, included women had lower parity, smoked less, and seemed to be older. In the current analysis, we first included all women with singleton pregnancies who were enrolled from 2000–2009 with available records from the MBRN who completed questionnaires at weeks 17 and 30 (n=87,074). Because delivery mode in first-time mothers is of great importance for further obstetric performance, we chose to address nulliparous women exclusively (n=41,149). We excluded pregnancies that were complicated by placenta previa (n=97) and transverse fetal presentation (n=45), the latter 2 conditions because they are absolute indications for elective CD. After omitting women with missing information on exercise in weeks 17 and 30 (n=479) and women with incomplete information on marital status, education, and prepregnancy body mass index (n=1341; 3.3%), the final sample consisted of 39,187 singleton pregnancies ( Figure 1 ). Two questionnaires that included items about maternal health, demographics, lifestyle behaviors, and medical history were completed during weeks 17 and 30. Questionnaire 2 was a food frequency questionnaire and not relevant for this study. All questionnaires are available at www.fhi.no/morogbarn .
Information about CD, which was indicated as acute, elective, or unspecified, was obtained from the MBRN. When the decision to do a CD is taken <8 hours before delivery, it was defined as an acute CD. Mode of delivery, as registered in the MBRN, is considered to be accurate with a 3% error rate when checked for completeness of CD notification against the birth protocols of the second largest obstetrics unit in Norway. Today, mode of delivery is registered electronically in the MBRN; hence, the error rate may even be lower than reported by Borthen et al (The MBRN web site, http://www.fhi.no/artikler/?id=94819 ).
The main exposure was exercise during pregnancy weeks 17 and 30, defined in terms of frequency and type. In the questionnaires, the participants reported how often they performed the following exercises: strolling, brisk walking, running (jogging or orienteering), bicycling, training in fitness centers, swimming, aerobic classes (low or high impact), prenatal aerobic classes, dancing (swing, rock, folkdance), skiing (cross-country skiing), ball games, horseback riding, and other. Because of the definition of exercise by Caspersen et al, strolling was categorized as nonexercise. We combined all exercises (excluding strolling) into an overall score. For each exercise, the following predefined frequencies were given: “never” (score: 0), “1–3 times per month” (score: 0.25), “once a week” (score: 1.0), “twice a week” (score: 2.0), and “≥3 times a week” (score: 3.0). The weekly frequency score were then summed across the 13 exercises and recoded into 5 categories that ranged from “never” to “≥6 times a week” to capture the most active women. “Nonexercisers” were those who responded “never” to all exercises or who reported strolling only. The same questions that were used to assess exercise frequency in our study have shown acceptable concurrent validity when compared with accelerometer in a subsample of pregnant women within the MoBa study.
We then grouped exercises based on type: nonexercisers (strolling and never), brisk walking, nonweightbearing (cycling and swimming), low-impact exercises (prenatal aerobics, low-impact aerobics, dancing, cross-country skiing, and fitness training), high-impact exercises (running, jogging, orienteering, and ball games), and other exercises (horseback riding and other). A mixed exercise group included those who did not have a single dominant exercise mode (eg, 1 session of jogging and 1 session of swimming per week).
Based on a review of previous studies and an assumed possible underlying mechanism, we assessed covariates and confounding factors using directed acyclic graphs. The following covariates were included in the final models: maternal age (years), prepregnancy body mass index (BMI), educational level (primary, secondary, college/university, and other), marital status (married, cohabitant, single, and other), fear of giving birth, pelvic girdle pain, and assisted reproduction before this pregnancy. Gestational weight gain, preeclampsia, pregnancy-induced hypertension, and gestational diabetes mellitus were not included as covariates because they might be on the causal pathway.
Analyses were performed using STATA software (version 13.0; Stata Corporation, College Station, TX). We explored the crude associations between a wide range of covariates and CDs using cross-tabulations. The same covariates were explored for associations with the exposure variable (exercise). Because of the high incidence of the outcome variables in our study, we used the generalized linear model with identity link function, Gaussian distribution, and robust variance to estimate the association between exercise during pregnancy and CD. We report crude and adjusted risk differences with 95% confidence intervals for different frequencies (Model 1) and types of exercise (Model 2) during pregnancy weeks 17 and 30. Vaginal delivery was the reference category in all models. Acute and elective CD was analyzed separately. When estimating the associations with acute CD, pregnancies that were terminated by an elective or unspecified CD were excluded (n=1341). Likewise, pregnancies that were terminated by an acute or unspecified CD (n=4745) were excluded in models that estimated the association with elective CD. We performed nonparametric tests for trend across ordered categories of exercise in both models.
Dose-response relationships between exercise frequency during pregnancy weeks 17 and 30 and risk of acute CD were investigated with the use of restricted cubic splines with 3 knots at fixed percentiles of the distribution. We conducted a test for nonlinearity by testing the coefficient of the second spline transformation equal to zero.
To investigate whether the association of pregnancy exercise with risk of having an acute or elective CD may be influenced by pregnancy-related morbidities or complications, we performed sensitivity analysis restricted to women without hypertension, preeclampsia, preexisting diabetes mellitus, gestational diabetes mellitus, obesity (morbidities inversely associated with exercise), and assisted reproduction.
Results
Among the 39,187 pregnancies in the cohort, 15.4% (n=6030) had a CD, of which more than three-quarters (77.8%, n=4689) were acute CD. Mean maternal age at delivery was 28.5±SD 4.4 years (range, 15–46 years). Mean prepregnancy BMI was 23.8±4.2 kg/m 2 , with 29.5% (n=11,569) of the women entering pregnancy being overweight or obese (prepregnancy BMI ≥25 kg/m 2 ). The mean gestational length was 39.6±1.8 completed weeks, and 7.4% (n=2913) of the pregnancies resulted from assisted reproduction. Mean birthweight was 3505±535 g). Sixteen percent of the women (n=6337) gave birth to a high-birthweight baby (≥4000 g), whereas 3.4% (n=1312) delivered a baby who weighed <2500 g ( Table 1 ). Breech presentation was observed in 4.9% of the pregnancies (n=1916).
| Maternal characteristics | Exercise frequency in week 17, n (%) | Total (N=39,187) | ||||
|---|---|---|---|---|---|---|
| Never (n=7215; 18.4%) | 1–3 Per mo (n=6833; 17.4%) | 1–2 Per wk (n=11,623; 29.7%) | 3–5 Per wk (n=10,831; 27.6%) | ≥6 Per wk (n=2685; 6.9%) | ||
| Age, y | ||||||
| <25 | 1988 (24.9) | 1611 (20.1) | 2,206 (27.6) | 1,797 (22.5) | 398 (5.0) | 8,000 (20.4) |
| 25–29 | 2912 (16.9) | 2978 (17.3) | 5,232 (30.4) | 4,877 (28.3) | 1209 (7.0) | 17,208 (43.9) |
| 30–34 | 1747 (16.0) | 1791 (16.4) | 3,284 (30.0) | 3,276 (29.9) | 856 (7.8) | 10,954 (28.0) |
| ≥35 | 568 (18.8) | 453 (15.0) | 901 (29.8) | 881 (29.1) | 222 (7.3) | 3,025 (7.7) |
| P =.000 | ||||||
| Education | ||||||
| Primary | 418 (31.6) | 257 (19.4) | 337 (25.5) | 252 (19.1) | 59 (4.5) | 1,323 (3.4) |
| Secondary | 3213 (24.8) | 2413 (18.6) | 3,542 (27.4) | 3,056 (23.6) | 720 (5.6) | 12,944 (33.0) |
| College/university | 3287 (14.0) | 3936 (16.7) | 7,359 (31.3) | 7,118 (30.3) | 1817 (7.7) | 23,517 (60.0) |
| Other | 297 (21.2) | 227 (16.2) | 385 (27.4) | 405 (28.9) | 89 (6.3) | 1,403 (3.6) |
| P =.000 | ||||||
| Marital status | ||||||
| Married | 2432 (17.7) | 2230 (16.2) | 4,148 (30.2) | 3,938 (28.7) | 980 (7.1) | 13,728 (35.0) |
| Single | 278 (24.0) | 187 (16.2) | 323 (27.9) | 294 (25.4) | 75 (6.5) | 1,157 (3.0) |
| Cohabitant | 4376 (18.5) | 4310 (18.2) | 6,993 (29.5) | 6,412 (27.1) | 1578 (6.7) | 23,669 (60.4) |
| Other | 129 (20.4) | 106 (16.8) | 159 (25.1) | 187 (29.5) | 52 (8.2) | 633 (1.6) |
| P =.000 | ||||||
| Prepregnancy body mass index, kg/m 2 | ||||||
| <18.5 | 277 (20.7) | 222 (16.6) | 368 (27.5) | 363 (27.1) | 110 (8.2) | 1,340 (3.4) |
| 18.5–24.9 | 4281 (16.3) | 4221 (16.1) | 7,756 (29.5) | 7,862 (29.9) | 2158 (8.2) | 26,278 (67.1) |
| 25–29.9 | 1725 (21.1) | 1618 (19.8) | 2,547 (31.1) | 1,964 (24.0) | 333 (4.1) | 8,187 (20.9) |
| 30–34.9 | 665 (26.9) | 561 (22.7) | 696 (28.2) | 488 (19.7) | 62 (2.5) | 2472 (6.3) |
| ≥35 | 267 (29.3) | 211 (23.2) | 256 (28.1) | 154 (16.9) | 22 (2.4) | 910 (2.3) |
| P =.000 | ||||||
| Smoking in pregnancy | ||||||
| No | 6241 (17.3) | 6241 (17.3) | 10,850 (30.1) | 10,230 (28.3) | 2548 (7.1) | 36,110 (92.7) |
| Yes | 905 (32.0) | 550 (19.5) | 716 (25.3) | 538 (19.0) | 117 (4.1) | 2,826 (7.3) |
| P =.000 | ||||||
| Preeclampsia | ||||||
| No | 6773 (18.2) | 6462 (17.4) | 11,045 (29.7) | 10,360 (27.8) | 2580 (6.9) | 37,220 (95.0) |
| Yes | 442 (22.5) | 371 (18.9) | 578 (29.4) | 471 (24.0) | 105 (5.3) | 1,967 (5.0) |
| P =.000 | ||||||
| Fear of giving birth | ||||||
| No | 4703 (20.3) | 4087 (17.7) | 6,728 (29.1) | 6,128 (26.5) | 1514 (6.5) | 23,160 (59.1) |
| Yes | 2512 (15.7) | 2746 (17.1) | 4,895 (30.5) | 4,703 (29.3) | 1171 (7.3) | 16,027 (40.9) |
| P =.000 | ||||||
| Preexisting high blood pressure | ||||||
| No | 7140 (18.4) | 6766 (17.4) | 11,508 (29.7) | 10,730 (27.6) | 2672 (6.9) | 38,816 (99.0) |
| Yes | 75 (20.2) | 67 (18.1) | 115 (31.0) | 101 (27.2) | 13 (3.5) | 371 (1.0) |
| P =.130 | ||||||
| Preexisting diabetes mellitus | ||||||
| No | 7161 (18.4) | 6788 (17.4) | 11,558 (29.7) | 10,781 (27.7) | 2674 (6.9) | 38,962 (99.4) |
| Yes | 54 (24.0) | 45 (20.0) | 65 (28.9) | 50 (22.2) | 11 (4.9) | 225 (0.6) |
| P =.078 | ||||||
| Gestational diabetes mellitus | ||||||
| No | 7125 (18.3) | 6770 (17.4) | 11,541 (29.7) | 10,775 (27.7) | 2668 (6.9) | 38,879 (99.2) |
| Yes | 90 (29.2) | 63 (20.5) | 82 (26.6) | 56 (18.2) | 17 (5.5) | 308 (0.8) |
| P =.000 | ||||||
| Pelvic girdle pain (week 30) | ||||||
| No | 6249 (17.8) | 6044 (17.2) | 10,467 (29.8) | 9,879 (28.1) | 2488 (7.1) | 35,127 (89.6) |
| Yes | 966 (23.8) | 789 (19.4) | 1,156 (28.5) | 952 (23.5) | 197 (4.9) | 4,060 (10.4) |
| P =.000 | ||||||
| Assisted reproduction | ||||||
| No | 6536 (18.0) | 6327 (17.4) | 10,769 (29.7) | 10,112 (27.9) | 2530 (7.0) | 36,274 (92.6) |
| Yes | 679 (23.3) | 506 (17.4) | 854 (29.3) | 719 (24.7) | 155 (5.3) | 2,913 (7.4) |
| P =.000 | ||||||
| Induction of labor | ||||||
| No | 6085 (18.2) | 5768 (17.3) | 9,932 (29.8) | 9,276 (27.8) | 2,323 (7.0) | 33,384 (85.2) |
| Yes | 1130 (19.5) | 1065 (18.4) | 1,691 (29.1) | 1,555 (26.8) | 362 (6.2) | 5,803 (14.8) |
| P =.009 | ||||||
| Birthweight, g | ||||||
| <2500 | 276 (21.0) | 217 (16.5) | 388 (29.6) | 348 (26.5) | 83 (6.3) | 1,312 (3.4) |
| 2500–4000 | 5700 (18.1) | 5456 (17.3) | 9,283 (29.5) | 8,836 (28.0) | 2238 (7.1) | 31,513 (80.4) |
| 4000–4500 | 992 (18.8) | 939 (17.8) | 1,630 (30.9) | 1,400 (26.5) | 316 (6.0) | 5,277 (13.5) |
| ≥4500 | 243 (22.9) | 219 (20.7) | 313 (29.5) | 239 (22.6) | 46 (4.3) | 1,060 (2.7) |
| Missing | 4 (16.0) | 2 (8.0) | 9 (36.0) | 8 (32.0) | 2 (8.0) | 25 (0.1) |
| P =.000 | ||||||
First-time mothers who were <25 years old had the highest proportion of nonexercisers at week 17 (24.9%) compared with women from 25–30 and 30–34 years old (16.9% and 16.0%, respectively; P =.000; Table 1 ). More women with a prepregnancy BMI within the normal range (18.5–24.9 kg/m 2 ) were exercising at least 3 times weekly compared with having a BMI of ≥30 kg/m 2 (38.1% and 21.5%, respectively; P =.000). It was more common to exercise at least weekly among women who reported fear of giving birth ( P =.000), being nonsmokers ( P =.000), without preeclampsia ( P =.000), without gestational diabetes mellitus ( P =.000), or pelvic girdle pain ( P =.000).
The crude and adjusted risk differences for having an acute CD in relation to frequency and type of exercise during pregnancy are summarized in Table 2 . Compared with nonexercisers, the negative risk differences of having an acute CD increased gradually from –1.2% to –2.2% with increasing frequency of exercise in week 17 ( P for trend <.001). Larger risk differences were observed for exercise frequency in week 30, ranging from –1.4% to –3.6% for exercising >5 times weekly ( P for trend <.001). High-impact exercise during pregnancy was associated with the lowest prevalence of acute CD giving the largest risk differences, particularly in week 30 ( P for trend =.008). Also low-impact exercises, brisk walking, nonweightbearing exercises (week 17), and horseback riding (week 30) were associated with a reduced risk of having an acute CD (Model 2). Maternal age and prepregnancy BMI were the most important confounders.
| Exercise | Acute cesarean delivery | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week 17 | Week 30 | |||||||||||
| % | Crude risk difference | Adjusted risk differences a | 95% Confidence interval | P value | P for trend | % | Crude risk difference | Adjusted risk differences a | 95% Confidence interval | P value | P for trend | |
| Model 1: frequency | .000 | .000 | ||||||||||
| Nonexerciser | 14.6 | 0 | 0 | 14.9 | 0 | 0 | ||||||
| 1–3 Times per mo | 13.0 | –1.6 | –1.2 | –2.3 to –0.01 | .049 | 12.7 | –2.1 | –1.4 | –2.4 to –0.3 | .011 | ||
| 1–2 Times per wk | 12.0 | –2.5 | –1.8 | –2.8 to –0.8 | .001 | 12.0 | –2.9 | –2.0 | –2.9 to –1.0 | .000 | ||
| 3–5 Times per wk | 11.4 | –3.2 | –2.0 | –3.1 to –1.0 | .000 | 10.6 | –4.3 | –2.9 | –3.8 to –1.9 | .000 | ||
| ≥6 Times per wk | 10.6 | –4.0 | –2.2 | –3.6 to –0.7 | .004 | 9.3 | –5.5 | –3.6 | –5.2 to –2.0 | .000 | ||
| Model 2: types | .133 | .008 | ||||||||||
| Nonexerciser | 14.6 | 0 | 0 | 14.9 | 0 | 0 | ||||||
| Brisk walking | 12.1 | –2.5 | –1.7 | –2.9 to –0.6 | .003 | 10.9 | –4.0 | –2.7 | –3.7 to –1.6 | .000 | ||
| Nonweightbearing b | 11.4 | –3.2 | –2.3 | –3.6 to –1.0 | .001 | 12.4 | –2.5 | –1.4 | –2.7 to 0.01 | .048 | ||
| Low-impact exercises | 11.8 | –2.8 | –1.7 | –2.9 to –0.5 | .005 | 10.7 | –4.2 | –2.9 | –4.0 to –1.8 | .000 | ||
| High-impact exercises | 9.6 | –5.1 | –3.0 | –4.4 to –1.5 | .000 | 8.9 | –5.9 | –3.4 | –6.0 to –0.8 | .011 | ||
| Horseback riding c | 12.0 | –2.6 | –1.7 | –3.3 to –0.1 | .037 | 11.5 | –3.4 | –2.5 | –3.8 to –1.2 | .000 | ||
| Mixed exercises | 12.7 | –1.9 | –1.4 | –2.4 to –0.3 | .011 | 12.4 | –2.5 | –1.6 | –2.6 to –0.7 | .001 | ||
a Adjusted for maternal age, prepregnancy body mass index, educational level, assisted reproduction, fear of giving birth, and pelvic girdle pain (week 30)
b Includes both swimming and bicycling
c Includes horseback riding and a nonclassifiable exercise category.
We also modelled exercise frequency (weeks 17 and 30, respectively) with risk of acute CD using restricted cubic splines ( Figure 2 ). The rate of change in the risk of acute CD seemed to decrease with increased frequency of exercise from 1–3 times a month and up to 5 times weekly in week 17 ( Figure 2 , A), after which no further decrease in risk of acute CD was observed ( P for nonlinearity=.003). The risk of acute CD seemed to rise with an exercise frequency >4 times weekly. However, the risk estimates are imprecise because of very few women in our study exercising at or above this level, which is reflected in the wide confidence intervals. In week 30 ( Figure 2 , B), the curve seemed to continue downwards but with a smaller rate of change in the risk of acute CD with increased exercise frequency ( P for nonlinearity=.027).
For elective CD, small risk differences were observed ( Table 3 ). A high exercise frequency in week 30 was associated with the greatest risk reduction for elective CD (–1.6%; P for trend=.189). Small risk differences were observed for exercise types during weeks 17 and 30 ( P for trend= .221 and .193, respectively). Overall, acute CD revealed the largest risk differences compared with elective CD at both time points in pregnancy (data not shown).
| Exercise | Elective cesarean delivery | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Week 17 | Week 30 | |||||||||||
| % | Crude risk differences | Adjusted risk differences a | 95% Confidence interval | P value | P for trend | % | Crude risk differences | Adjusted risk differences a | 95% Confidence interval | P value | P for trend | |
| Model 1: frequency | .441 | .189 | ||||||||||
| Nonexerciser | 4.8 | 0 | 0 | 4.8 | 0 | 0 | ||||||
| 1–3 Times per mo | 4.0 | –0.8 | –0.6 | –1.3 to –0.1 | .097 | 4.1 | –0.6 | –0.3 | –1.0 to 0.3 | .330 | ||
| 1–2 Times per wk | 3.5 | –1.3 | –1.1 | –1.7 to –0.5 | .001 | 3.2 | –1.4 | –1.2 | –1.8 to –0.7 | .000 | ||
| 3–5 Times per wk | 3.7 | –1.0 | –0.9 | –1.5 to –0.2 | .012 | 3.8 | –0.9 | –0.6 | –1.2 to –0.03 | .041 | ||
| ≥6 Times per wk | 3.4 | –1.3 | –1.0 | –1.9 to –0.1 | .023 | 2.8 | –1.8 | –1.6 | –2.5 to –0.6 | .001 | ||
| Model 2: types | .221 | .193 | ||||||||||
| Nonexerciser | 4.6 | 0 | 0 | 4.6 | 0 | 0 | ||||||
| Brisk walking | 3.2 | –1.4 | –1.2 | –1.9 to –0.5 | .000 | 3.2 | –1.4 | –1.0 | –1.7 to –0.4 | .001 | ||
| Nonweightbearing b | 3.4 | –1.2 | –1.0 | –1.8 to –0.2 | .016 | 3.7 | –0.9 | –0.6 | –1.4 to 0.2 | .147 | ||
| Low-impact exercises | 3.9 | –0.7 | –0.5 | –1.3 to 0.2 | .153 | 3.4 | –1.2 | –1.0 | –1.7 to –0.4 | .003 | ||
| High-impact exercises | 3.1 | –1.5 | –1.1 | –1.9 to –0.2 | .017 | 3.0 | –1.5 | –1.0 | –2.6 to 0.6 | .233 | ||
| Horseback riding c | 3.8 | –0.8 | –0.8 | –1.8 to 0.2 | .115 | 3.3 | –1.3 | –1.2 | –2.0 to –0.4 | .002 | ||
| Mixed exercises | 3.7 | –1.0 | –0.8 | –1.4 to –0.1 | .019 | 3.7 | –0.9 | –0.6 | –1.1 to 0.02 | .057 | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


