Chapter 23
Epidural and Spinal Analgesia /Anesthesia for Labor and Vaginal Delivery
Cynthia A. Wong MD
Chapter Outline
PREPARATION FOR NEURAXIAL ANALGESIA
INITIATION OF EPIDURAL ANALGESIA
INITIATION OF SPINAL ANALGESIA
ANALGESIA/ANESTHESIA FOR VAGINAL DELIVERY
SIDE EFFECTS OF NEURAXIAL ANALGESIA
COMPLICATIONS OF NEURAXIAL ANALGESIA
EFFECTS OF NEURAXIAL ANALGESIA ON THE PROGRESS OF LABOR
EFFECTS OF NEURAXIAL ANALGESIA ON THE FETUS AND NEONATE
CONCLUSIONS AND RECOMMENDATIONS
Epidural analgesia and spinal analgesia are the most effective methods of intrapartum pain relief in contemporary clinical practice.1,2 During the first stage of labor, pain results primarily from distention of the lower uterine segment and cervix (see Chapter 20). Painful impulses are transmitted by means of visceral afferent nerve fibers, which accompany sympathetic nerve fibers and enter the spinal cord at the 10th, 11th, and 12th thoracic and 1st lumbar spinal segments. As labor progresses and the fetus descends in the birth canal, distention of the vagina and perineum results in painful impulses that are transmitted via the pudendal nerve to the 2nd, 3rd, and 4th sacral spinal segments. Neuraxial analgesia is the only form of analgesia that provides complete analgesia for both stages of labor. During the first stage of labor, visceral pain impulses entering the spinal cord at T10 to L1 must be blocked. During the late first stage of labor and the second stage of labor, somatic impulses entering the spinal cord from S2 to S4 must also be blocked (see Chapter 20).
In a survey of 1000 consecutive women who chose a variety of analgesic techniques for labor and vaginal delivery (including nonpharmacologic methods, transcutaneous electrical nerve stimulation, intramuscular meperidine, inhalation of nitrous oxide, epidural analgesia, and a combination of these techniques), pain relief and overall satisfaction with the birth experience were greater in patients who received epidural analgesia.2 Similarly, randomized studies that have compared epidural analgesia with systemic opioids and/or inhalation analgesia (i.e., nitrous oxide) have shown that pain scores are lower and patients are more satisfied with neuraxial analgesia.3
The provision of analgesia for labor may result in other benefits. Effective epidural analgesia reduces maternal plasma concentrations of catecholamines (Figure 23-1).4 Decreased alpha- and beta-adrenergic receptor stimulation may result in better uteroplacental perfusion and more effective uterine activity.5,6 Painful uterine contractions result in maternal hyperventilation. The hyperventilation, in turn, leads to maternal respiratory alkalosis, a leftward shift of the oxyhemoglobin dissociation curve, increased maternal hemoglobin affinity for oxygen, and reduced oxygen delivery to the fetus.7 Hypocarbia also leads to hypoventilation between contractions, which may cause a decrease in maternal PaO2. Effective epidural analgesia blunts this “hyperventilation-hypoventilation” cycle.8 Additionally, one study showed that paternal anxiety levels were lower, and both paternal involvement in the childbirth process and paternal satisfaction were greater, in men whose partners received epidural analgesia than in those whose partners did not.9 Finally, the presence of an epidural catheter and effective epidural analgesia facilitate the rapid initiation of epidural anesthesia for emergency cesarean delivery. Neuraxial anesthesia for cesarean delivery is associated with greater overall maternal safety than emergency administration of general anesthesia (see Chapter 26).10
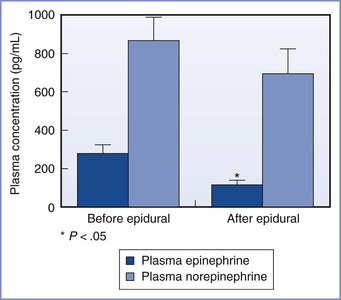
FIGURE 23-1 Influence of epidural analgesia on maternal plasma concentrations of catecholamines during labor. *P < .05 compared with before initiation of epidural analgesia. (Modified from Shnider SM, Abboud TK, Artal R, et al. Maternal catecholamines decrease during labor after lumbar epidural anesthesia. Am J Obstet Gynecol 1983; 147:13-5.)
Neuraxial analgesia is not used by all laboring women, although surveys of obstetric anesthesia practice in the United States have shown that the use of neuraxial analgesia has grown over the past three decades.11 Data collected from the U.S. Standard Certificate of Live Birth in 27 states in 2008 indicated that 61% of women who had a singleton vaginal delivery received neuraxial analgesia.12 The rate was higher among white women than in women of other races/ethnicities, and it was also higher in larger maternal units than in smaller units.11,12 In the United Kingdom, the National Health Service Maternity Statistics for 2010-2011 indicated that approximately one third of parturients chose to receive neuraxial analgesia during childbirth.13
The availability of skilled anesthesia providers influences the neuraxial analgesia rate.11 Other factors include the information and advice provided to pregnant women by obstetricians, nurses, and childbirth education instructors. The personal and cultural expectations of a laboring woman, as well as obstetric complications,2 also affect the childbirth experience and the use of neuraxial analgesia (see Chapters 20 and 21).
In contemporary clinical practice, health care costs have assumed significant importance. Studies using 1998 data estimated that the incremental cost to society for providing epidural labor analgesia was $260 to $340 per parturient (approximately $367 to $481 in 2012 dollars).14,15 A major problem with such analyses is the difficulty of determining the total value of neuraxial analgesia. For example, the ability to rapidly convert epidural analgesia to surgical anesthesia may also have value.
Ideally, the anesthesia provider should tailor the analgesic technique to meet the individual parturient’s needs. Factors that should be considered in formulating an analgesic plan for individual parturients include coexisting maternal disease, the airway examination, fetal status, spontaneous versus induced labor, stage of labor, and anticipated risk for operative delivery. The risks and benefits of the various epidural and spinal analgesic techniques should be assessed for each parturient. Good technique requires thoughtful preparation and meticulous attention to detail to ensure maternal and fetal safety.
The ideal labor analgesic technique is safe for both the mother and the infant, does not interfere with the progress of labor and delivery, and provides flexibility in response to changing conditions. In addition, the ideal technique provides consistent pain relief, has a long duration of action, minimizes undesirable side effects (e.g., motor block), and minimizes ongoing demands on the anesthesia provider’s time. No single technique or anesthetic agent is ideal for all parturients during labor. The American Society of Anesthesiologists (ASA) has published practice guidelines for obstetric anesthesia (see Appendix B),16 as well as guidelines for neuraxial anesthesia in obstetric patients (see Appendix A). Guidelines promulgated by professional organizations in other countries also address obstetric anesthesia care. All obstetric anesthesia providers should review their country’s respective guidelines. Specific neuraxial techniques for labor analgesia, including their advantages, disadvantages, side effects, and complications, are considered in this chapter.
Preparation for Neuraxial Analgesia
Indications and Contraindications
Epidural analgesia is indicated to treat the pain experienced by a woman in labor. In 2008 and 2010, respectively, the American College of Obstetricians and Gynecologists (ACOG)17 and the ASA18 reaffirmed an earlier, jointly published opinion that stated that “in the absence of a medical contraindication, maternal request is a sufficient medical indication for pain relief during labor.” Furthermore, the ACOG19 has stated that “decisions regarding analgesia should be closely coordinated among the obstetrician, the anesthesiologist, the patient, and skilled support personnel.” Neuraxial analgesia is an appropriate treatment for the pain of labor, including early labor (defined as regular uterine contractions that cause progressive effacement and dilation of the uterine cervix). Randomized controlled trials20–24 and a meta-analysis25 have confirmed that initiation of neuraxial analgesia in early labor does not increase the risk for cesarean delivery (see later discussion).
Epidural analgesia may facilitate an atraumatic vaginal breech delivery, the vaginal delivery of twin infants, and vaginal delivery of a preterm infant (see Chapters 34 and 35). By providing effective pain relief, epidural analgesia facilitates blood pressure control in preeclamptic women (see Chapter 36). Epidural analgesia also blunts the hemodynamic effects of uterine contractions (e.g., sudden increase in cardiac preload) and the associated pain response (tachycardia, increased systemic vascular resistance, hypertension, hyperventilation) in patients with other medical complications (e.g., mitral stenosis, spinal cord injury, intracranial neurovascular disease, asthma; see Chapters 42, 49, and 53).
Box 23-1 lists the contraindications to administration of epidural or spinal analgesia. Some anesthesiologists have suggested that systemic maternal infection, preexisting neurologic disease, or severe stenotic heart lesions are relative contraindications to neuraxial analgesia. However, most cases of systemic infection (especially if properly treated), or neurologic or cardiac disease, do not contraindicate the administration of neuraxial analgesia (see Chapters 37, 42, and 49). It is also controversial whether mild or isolated abnormalities in tests of blood coagulation preclude the use of neuraxial analgesia. The dose and timing of administration of drugs administered for thromboprophylaxis must also be considered (see Chapter 44).26 The anesthesia provider should consider the risks and benefits of neuraxial analgesia for each patient individually.
Thorough preparation for neuraxial labor analgesia involves several steps (Box 23-2). These include (1) a review of the parturient’s obstetric history; (2) a focused preanesthetic evaluation that includes maternal obstetric, anesthetic, and health history; and (3) a brief physical examination (i.e., vital signs, airway, heart, lungs, and back).16 Routine measurement of the platelet count is not necessary; however, assessment of the platelet count and other laboratory measurements may be indicated in selected patients.16 Similarly, routine intrapartum blood typing and screening or crossmatching is not necessary in healthy parturients, although consideration should be given to sending a blood sample to the blood bank (to facilitate the rapid availability of blood products in case of emergency need).16 For parturients at increased risk for hemorrhage, intrapartum typing, and screening or crossmatching should be performed. Fetal well-being should be assessed by a skilled provider, and equipment (including resuscitation equipment) should be checked by the anesthesia provider (see Box 12-1). Informed consent should be obtained (see Chapters 12 and 33). Early and ongoing communication among the obstetric and anesthesia providers, nursing staff, and other members of the multidisciplinary team is encouraged.
Types of Neuraxial Analgesia
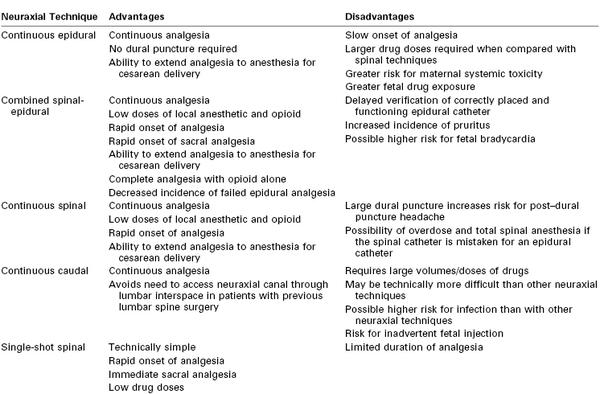
The technical aspects of neuraxial analgesic/anesthetic techniques are discussed in detail in Chapter 12. These techniques include continuous epidural, combined spinal-epidural, and caudal analgesia and continuous and single-shot spinal analgesia. Continuous epidural and combined spinal-epidural analgesia are the most common techniques used for neuraxial labor analgesia. There are advantages and disadvantages to each technique (Table 23-1).
Epidural Analgesia
Continuous lumbar epidural analgesia has been the mainstay of neuraxial labor analgesia for several decades. Placement of an epidural catheter allows analgesia to be maintained until after delivery. No dural puncture is required. The presence of a catheter and effective analgesia allow the conversion to epidural anesthesia should cesarean delivery be necessary. Injection of a local anesthetic in the lumbar epidural space allows both cephalad and caudad spread of the anesthetic solution.
Analgesia is initiated by bolus injection of drug(s) through the epidural needle, catheter, or both. Analgesia is maintained with anesthesia provider- or patient-administered intermittent bolus injections or a continuous epidural infusion, or both. The catheter is removed after delivery when there is no further need for analgesia or anesthesia.
Combined Spinal-Epidural Analgesia
Combined spinal-epidural (CSE) analgesia has become increasingly popular in the past 15 years. Onset of complete analgesia is significantly faster than with epidural techniques (2 to 5 minutes versus 10 to 15 minutes, respectively).27 In a meta-analysis of the onset time of CSE compared with low-dose epidural analgesia,27 the mean difference in onset was −5.4 minutes (95% confidence interval [CI], −7.3 to −3.6). More women with spinal analgesia than with epidural analgesia had effective analgesia at 10 minutes (relative risk [RR], 1.9; 95% CI, 1.5 to 2.5). In particular, the onset of sacral analgesia is significantly slower after the initiation of lumbar epidural analgesia than with spinal analgesia. It may take several hours of lumbar epidural infusion, or several bolus injections of local anesthetic into the lumbar epidural space, to achieve sacral analgesia. Rapid onset of sacral analgesia is advantageous in the parturient in whom analgesia is initiated late in the first stage of labor or in a parous parturient with rapid progress of labor. Spinal analgesia requires significantly lower drug doses to attain effective analgesia than does epidural analgesia; therefore, the risk for local anesthetic systemic toxicity is decreased. In addition, there is less systemic absorption of spinal anesthetic agents into the maternal circulation, so maternal and fetal plasma drug concentrations are lower with spinal than with epidural analgesia.
An additional advantage of spinal analgesia is that complete analgesia for early labor can be accomplished with the intrathecal injection of a lipid-soluble opioid without the addition of a local anesthetic. Thus, motor blockade is avoided and the risk for hypotension is lower.28 This method is ideal for patients who wish to ambulate or for those with preload-dependent cardiac conditions such as stenotic heart lesions. Finally, use of the CSE technique may lower the incidence of failure of epidural analgesia (e.g., a nonfunctioning epidural catheter).29,30 The likelihood of an epidural catheter placed for labor analgesia failing to provide satisfactory anesthesia for a subsequent cesarean delivery was more than five times higher for catheters placed as part of an epidural technique than for catheters placed as part of a CSE technique.31
Cappiello et al.32 have described a technique in which a dural puncture is made with a small-gauge spinal needle but no drug is injected into the subarachnoid space. After injection of epidural local anesthetic and opioid, blockade of sacral dermatomes occurred more frequently in parturients with a dural puncture than in those without, presumably because of enhanced anesthetic solution migration across the dural puncture site.
CSE analgesia has several possible undesirable side effects. Dural puncture is required to initiate CSE analgesia, although puncture with a small-gauge pencil-point needle does not appear to increase the risk for post–dural puncture headache.27 A more serious concern, however, is that dural puncture during labor may be a risk factor for postpartum neuraxial infection, a rare but potentially life-threatening complication (see Chapter 32).
The incidence of pruritus is higher with intrathecal opioid administration than with epidural opioid administration.27 Another potential drawback of CSE analgesia is that it is not clear for 1 to 2 hours after initiation of analgesia whether the epidural catheter is properly sited in the epidural space. Thus, CSE analgesia may not be the technique of choice if a functioning epidural catheter is critical to the safe care of the patient (e.g., a mother with an anticipated difficult airway or a worrisome fetal heart rate [FHR] tracing).
The most common CSE technique for labor analgesia is the needle-through-needle technique in a midlumbar interspinous space (see Chapter 12). Analgesia is maintained via the epidural catheter, as with traditional epidural analgesia.
Continuous Spinal Analgesia
Continuous spinal analgesia is used occasionally for labor analgesia but is not practical for most parturients. Because the available catheters require dural puncture with a large-gauge introducer needle, the technique is associated with an unacceptably high incidence of post–dural puncture headache. However, continuous spinal analgesia is a management option in patients with unintentional dural puncture. Continuous spinal analgesia can readily be converted to surgical anesthesia if necessary.
Caudal Analgesia
Continuous caudal epidural analgesia is used infrequently in modern obstetric anesthesia practice. It is technically more difficult to place a caudal catheter than a lumbar epidural catheter. Large volumes of anesthetic solution are required to extend neuroblockade to the low thoracic spinal segments, resulting in higher maternal plasma concentrations of drug. There is a risk for needle/catheter misplacement and direct injection into the fetus. However, this technique is useful for parturients in whom access to the lumbar spinal canal is not possible (e.g., because of a fused lumbar spine).
Single-Shot Techniques
In general, single-shot techniques (spinal, lumbar epidural, or caudal) are not useful for most laboring women because of their limited duration of action. These techniques may be indicated for parturients who require analgesia or anesthesia shortly before anticipated vaginal delivery or in settings in which continuous epidural analgesia is not possible.33
Informed Consent
Informed consent is an important aspect of preparation for neuraxial labor analgesia (see Chapters 12 and 33). The preanesthetic evaluation and informed consent process allow the physician to allay the patient’s concerns and to demonstrate a commitment to her care. Most laboring women understand the need for informed consent and appreciate the opportunity to participate in decisions about their care.
Equipment and Monitors
Resuscitation equipment, drugs, and supplies must be immediately available for the management of serious complications of neuraxial analgesia (e.g., hypotension, total spinal anesthesia, systemic local anesthetic toxicity) (see Box 12-1).16 Emergency airway equipment should be checked before the administration of neuraxial analgesia.
During the initiation of neuraxial analgesia, the parturient’s oxygen saturation is measured continuously and the blood pressure is assessed every 2 to 3 minutes for 15 to 20 minutes after the neuraxial anesthetic administration, or until the mother is hemodynamically stable (see Chapter 12). The FHR should be monitored before and after the initiation of neuraxial analgesia; it may be difficult to monitor the FHR during the actual procedure.16 During maintenance of neuraxial analgesia, maternal blood pressure is measured every 15 to 30 minutes, or more frequently if hypotension ensues. The sensory level of analgesia and the intensity of motor block (Box 23-3) are assessed after the administration of the test and therapeutic doses of local anesthetics. Subsequently, sensory level, motor block, and pain control are assessed at regular intervals.
Intravenous Hydration
Placement of an intravenous catheter (preferably 18-gauge or larger) and correction of hypovolemia with intravenous hydration are necessary before the initiation of neuraxial analgesia to mitigate hypotension that can result from sympathetic blockade. Data from small studies are conflicting as to whether a fluid bolus administered immediately before the initiation of analgesia decreases the risk for nonreassuring FHR patterns.34–36 Most anesthesia providers administer approximately 500 mL of lactated Ringer’s solution (without dextrose), although the ASA Task Force on Obstetric Anesthesia has stated that a fixed volume of intravenous fluid is not required before neuraxial analgesia is initiated.16 Severe hypotension is less likely with the contemporary practice of administering a dilute solution of local anesthetic for epidural analgesia or an intrathecal opioid for spinal analgesia.
Studies of intravenous hydration and spinal anesthesia for cesarean delivery suggest that there is no advantage to administering the fluid before the initiation of anesthesia (preload) compared with administering the fluid at the time of initiation of anesthesia (co-load).37 Rarely, hydration should be guided by serial assessment of intravascular fluid volume (e.g., central venous pressure, transthoracic echocardiography). Fluid administration should be judicious in parturients at risk for pulmonary edema (e.g., women with severe preeclampsia).
A balanced electrolyte solution (e.g., lactated Ringer’s solution) without dextrose is the most commonly used intravenous fluid for bolus administration. Data are conflicting as to whether the maintenance intravenous infusion of dextrose-containing fluid during labor is associated with a lower incidence of umbilical cord blood acidemia.38,39 One randomized controlled trial demonstrated shorter labor in women who received an intravenous solution of normal saline with dextrose compared with saline without dextrose.40 However, anesthesia and obstetric providers should avoid the bolus administration of dextrose-containing solutions in laboring women.
Maternal Positioning
Either the lateral decubitus or the sitting position can be used during initiation of neuraxial analgesia (see Chapter 12). Factors to consider when positioning the parturient for the procedure include patient comfort, avoidance of aortocaval compression, ability to monitor the FHR, provider comfort and experience, and optimal positioning of the spine and palpation of landmarks. Patient position relative to the baricity of the anesthetic solution should be considered during initiation of spinal analgesia/anesthesia. There is little evidence that patient position influences the extent of neuroblockade during initiation of epidural analgesia/anesthesia. After completion of the procedure, parturients should be assisted to the lateral position for the first 15 to 30 minutes after the neuraxial injection to alleviate aortocaval compression.
Initiation of Epidural Analgesia
A procedure for initiating epidural labor analgesia is outlined in Box 23-4. Commonly, after siting the epidural catheter in the epidural space, a test dose is administered to rule out intrathecal or intravascular placement of the epidural catheter. After a negative test, epidural analgesia is established with the incremental injection of a local anesthetic, usually in combination with a lipid-soluble opioid. Maternal vital signs are monitored and clinical analgesia is verified.
Epidural Test Dose
The purpose of the test dose is to help identify unintentional cannulation of a vein or the subarachnoid space. The test dose should contain a dose of local anesthetic and/or another marker sufficient to allow the recognition of intravenous or subarachnoid injection but not so large as to cause systemic toxicity or total spinal anesthesia. The most common intravascular test dose contains epinephrine (see Chapter 12).
The use of the epinephrine test dose in obstetrics is not without detractors. Some anesthesia providers fear that intravenous injection of epinephrine may decrease uteroplacental perfusion and precipitate fetal compromise. However, there has been no report of adverse neonatal outcome after intravenous injection of an epinephrine-containing test dose. Another argument against routine use of a test dose is that aspiration of multi-orifice catheters is 98% sensitive in identifying their intravascular location.41 (The sensitivity of aspiration is significantly lower for single-orifice catheters.) The epidural test dose contributes to undesirable motor blockade.42,43 Finally, because modern epidural labor analgesia involves the infusion of a low concentration of local anesthetic solution, unintentional intravascular or intrathecal administration is not likely to result in cardiovascular collapse or total spinal anesthesia.
Others argue that the test dose still has a role in obstetric anesthesia practice.44 Large volumes of a concentrated local anesthetic solution are still routinely administered for emergency cesarean delivery. Although not a safety issue, it is easier for the parturient and anesthesia provider to identify a misplaced catheter at the time of initial placement and to replace the catheter at that time rather than identify the misplaced catheter after the sterile field has been breached and the parturient repositioned.
The epinephrine test dose is less specific in laboring women because cyclic changes in maternal heart rate complicate interpretation of its effects.45 For this reason, if used, the test dose should be given immediately after a uterine contraction so there is less confusion as to whether tachycardia is caused by pain or intravenous epinephrine. Other methods of detecting intravascular injection are discussed in Chapter 12.
No matter whether a formal test dose is used or not, it is imperative that the anesthesia provider take the time to look for evidence of unintentional intrathecal injection of local anesthetic. Finally, every anesthesia provider should remember that no single test dose regimen can exclude every case of unintentional intravenous or subarachnoid injection. Box 12-3 summarizes steps that may be taken to decrease the risk for unintentional intravenous or subarachnoid injection of local anesthetic.
Choice of Drugs
The ideal analgesic drug for labor would provide rapid onset of effective analgesia with minimal motor blockade, minimal risk for maternal toxicity, and negligible effect on uterine activity and uteroplacental perfusion. It would undergo limited transplacental transfer and thus have minimal direct effect on the fetus. Finally, this ideal agent would have a long duration of action. Although this perfect analgesic drug does not exist, the combination of a local anesthetic with an opioid allows us to approach this goal.
Traditionally, local anesthetics were administered to block both the visceral pain of labor (lower uterine segment distention and cervical dilation) and the somatic pain (descent of the fetus in the birth canal). Almost 40 years ago, investigators identified dense concentrations of opioid receptors in the dorsal horn of the spinal cord.46 The application of small doses of an opioid to these receptor sites generates a specific and profound opioid response.46 The introduction of neuraxial opioids to the armamentarium of the obstetric anesthesia provider moved us closer to the prediction made by Benjamin Rush in 1805: “A medicine would be discovered which should suspend sensibility altogether and leave irritability or powers of motion unimpaired.”47 Intrathecal opioids effectively relieve the visceral pain of the early first stage of labor, although they must be combined with a local anesthetic to effectively relieve the somatic pain of the late first stage and the second stage of labor. The combination of a local anesthetic with a lipid-soluble opioid allows for the use of lower doses of each agent, thus minimizing undesirable side effects. For example, when used alone without an opioid, the local anesthetic dose required for effective epidural analgesia is associated with an unacceptably high incidence of motor blockade. Similarly, used alone, high doses of epidural opioid are required for satisfactory analgesia during early labor, and such doses are associated with significant systemic absorption and systemic side effects. The addition of an opioid to the local anesthetic also shortens latency,48 an important aspect of labor analgesia, especially with the use of long-acting (and therefore, long-latency) local anesthetics. Thus, contemporary epidural labor analgesia practice most often incorporates low doses of a long-acting local anesthetic combined with a lipid-soluble opioid.
Local Anesthetics
Bupivacaine.
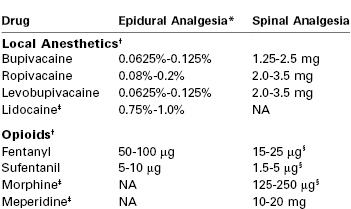
Traditionally, the amide local anesthetic bupivacaine has been the most commonly used agent for epidural labor analgesia. Bupivacaine is highly protein-bound, a feature that limits transplacental transfer. The umbilical vein–to–maternal vein concentration ratio is approximately 0.3.49 After epidural administration of bupivacaine (without opioid) during labor, the patient first perceives pain relief within 8 to 10 minutes,50 but approximately 20 minutes is required to achieve the peak effect. Duration of analgesia is approximately 90 minutes. Bupivacaine 6.25 to 12.5 mg (e.g., 10 to 20 mL of a 0.0625% solution, or 5 to 10 mL of a 0.125% solution) combined with fentanyl or sufentanil is adequate to initiate labor analgesia in most parturients (Table 23-2).
The potency of local anesthetics for neuraxial labor analgesia is often assessed by determining the median effective concentration of local anesthetic solution when administered as a 20-mL epidural bolus (this concentration is often referred to as the minimum local anesthetic concentration [MLAC]). It is lower for women in early labor than in late labor,51 and it is also lower when the local anesthetic is combined with a lipid-soluble opioid.52
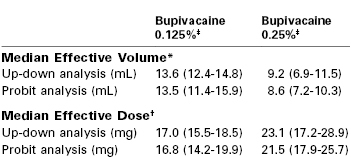
It is important to consider both the local anesthetic dose and concentration for initiation and maintenance of epidural analgesia. Christiaens et al.53 randomly assigned parturients to receive epidural bupivacaine 20 mg diluted in 4 mL, 10 mL, or 20 mL (0.5%, 0.2%, and 0.1% solutions, respectively). Analgesia in the 10-mL and 20-mL groups was superior to that in the 4-mL group, and duration of analgesia was longest in the 20-mL group. Lyons et al.54 compared the minimum local anesthetic volume (MLAV) and minimum local anesthetic dose (MLAD) for 0.125% and 0.25% bupivacaine for epidural labor analgesia. Bupivacaine 0.125% produced analgesia equivalent to that provided by bupivacaine 0.25%, with a 50% increase in required volume and a 25% reduction in dose (Table 23-3). Stated differently, a dose-sparing effect is achieved by administering a 0.125% solution of bupivacaine rather than a 0.25% solution. Ginosar et al.55 randomized parturients to receive maintenance of analgesia with an epidural infusion of either bupivacaine 0.25% at 5 mL/h or bupivacaine 0.0625% at 20 mL/h (10 mg/h in both groups). The median bupivacaine dose was lower and patient satisfaction was greater with bupivacaine 0.0625% than with bupivacaine 0.25%. Together, these data suggest that epidural analgesia and safety are improved with the use of low concentration–high volume local anesthetic solutions.
Ropivacaine.
Ropivacaine, a relatively newer amide local anesthetic, is similar to bupivacaine in structure and pharmacodynamics.56 It is a homologue of bupivacaine and mepivacaine, but unlike these other local anesthetics it is formulated as a single-levorotary enantiomer rather than a racemic mixture (see Chapter 13). Studies of pregnant sheep have demonstrated that clinically relevant plasma concentrations of ropivacaine do not adversely affect uterine blood flow.57
Studies in vitro and in vivo have shown that ropivacaine is less cardiodepressant and arrhythmogenic than bupivacaine when doses of equal mass are compared.58,59 Ropivacaine is cleared more rapidly than bupivacaine after intravenous administration in both pregnant and nonpregnant sheep. Consequently, a larger dose of drug—but not a higher plasma concentration—is required to produce systemic toxicity.60 These findings suggest that ropivacaine may have a greater margin of safety than bupivacaine if unintentional intravenous injection occurs in pregnant women. However, many early investigations assumed that ropivacaine and bupivacaine are equipotent; subsequent studies have demonstrated that ropivacaine is 25% to 40% less potent than bupivacaine.61–63 In one study that characterized the full dose-response curves, the slope of the bupivacaine and ropivacaine curves were similar, suggesting that the nature of the drug-receptor interaction is not different between the two drugs.63 When ropivacaine concentrations are adjusted for this difference in potency, there is a less clear advantage for ropivacaine in terms of the risk for systemic toxicity.61 In reality, systemic toxicity is not a major concern with the contemporary administration of a dilute solution of local anesthetic for epidural labor analgesia.
Several studies that compared equal concentrations of ropivacaine and bupivacaine given by patient-controlled epidural analgesia (PCEA) have not found any significant difference in clinical efficacy between the two local anesthetics.64–68 Other studies that adjusted for the potency difference and compared equipotent concentrations (e.g., 0.0625% bupivacaine versus 0.1% ropivacaine) also found no difference in clinical efficacy.69,70 It is important to recognize that potency is an unchanging property of a drug, whereas clinical efficacy is influenced by multiple variables. For example, ropivacaine has a longer duration of analgesia than bupivacaine,61 which may offset its lesser potency when it is administered by continuous epidural infusion.
Early clinical studies suggested that ropivacaine is associated with less motor block than bupivacaine71,72; avoidance of motor blockade is a desirable characteristic of a local anesthetic used for epidural analgesia during labor. However, these studies also compared equal concentrations of ropivacaine and bupivacaine, and the observed lower degree of motor blockade may reflect the lesser potency of ropivacaine. A study of the relative motor-blocking potencies of epidural ropivacaine and bupivacaine showed that ropivacaine was less potent than bupivacaine in terms of motor blockade,73 a finding that corresponded to the relative analgesic potencies of the two drugs.61,62 The differences in potency of motor blockade may not be relevant with the use of low concentrations of local anesthetic. Several clinical studies64,66,74 and a well-conducted meta-analysis of studies that compared epidural ropivacaine and bupivacaine75 did not demonstrate an advantage for ropivacaine in terms of outcome of labor (see later discussion), although the incidence of motor blockade was less in the ropivacaine groups.66,74,75
There is no clear evidence of greater patient safety, lower risk for instrumental vaginal delivery, or other improved outcomes when ropivacaine is used to provide epidural labor analgesia.74,76 A 2010 review concluded that there is no advantage to the routine use of ropivacaine compared with bupivacaine for labor analgesia.76 In contrast, ropivacaine offers greater patient safety in settings in which high concentrations and greater volumes of drugs are administered (e.g., brachial plexus blockade or epidural anesthesia for cesarean delivery).77
Like bupivacaine, ropivacaine is often combined with fentanyl or sufentanil for labor analgesia. Ropivacaine concentrations used to initiate epidural analgesia range from 0.08% to 0.2% (see Table 23-2). Higher concentrations are used if the drug is administered without an opioid.
Levobupivacaine.
Levobupivacaine is the levorotary enantiomer of bupivacaine (which is a racemic mixture). It is not available in the United States. Both preclinical and clinical studies have suggested that, like ropivacaine, levobupivacaine has less potential for cardiotoxicity than bupivacaine when equal doses of the two drugs are compared.78,79 One study found that levobupivacaine was essentially equipotent to bupivacaine with a potency ratio of 0.98; however, the 95% CI was wide (0.67 to 1.41).80 Other studies have suggested that levobupivacaine and ropivacaine have similar potency.81,82 In an MLAC study that compared the motor blocking potency of bupivacaine and levobupivacaine,83 levobupivacaine was less potent than bupivacaine (potency ratio, 0.87; 95% CI, 0.77 to 0.98).83 Beilin et al.66 compared epidural bupivacaine, ropivacaine, and levobupivacaine (0.0625% with fentanyl 2 µg/mL) for labor analgesia. There were no differences among groups in obstetric outcomes, although the incidence of motor blockade was lower in the ropivacaine and levobupivacaine groups. Therefore, although epidural bupivacaine is more potent than ropivacaine for both sensory and motor blockade during labor, and may be more potent than levobupivacaine, there do not appear to be any clinical advantages of one drug over the other two drugs for epidural labor analgesia.
Lidocaine.
Lidocaine is an amide local anesthetic with a duration of action intermediate between those of bupivacaine and 2-chloroprocaine. During labor, the administration of a 0.75% to 1.0% solution of lidocaine typically provides satisfactory analgesia. Lidocaine is not commonly used for initiation or maintenance of epidural labor analgesia, in part because of its shorter duration of action in comparison with bupivacaine, ropivacaine, and levobupivacaine. Lidocaine is less protein-bound than these other amide local anesthetics, and at delivery, the umbilical vein–to–maternal vein lidocaine concentration ratio is approximately twice that of bupivacaine.84 Early studies discouraged the epidural administration of lidocaine in pregnant women because epidural lidocaine was associated with abnormal neonatal neurobehavioral findings.85
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree