RISK FACTORS FOR ANTERIOR CRUCIATE LIGAMENT INJURY
In order to understand the risk factors for pediatric and adolescent ACL injury, one must evaluate elements that are both intrinsic to the patient as well as external factors.10,11 Although some intrinsic risk factors are not controllable by the adolescent, many intrinsic and all extrinsic risk factors are modifiable to some extent.
Intrinsic Risk Factors
Intrinsic risk factors are variables that are inherent to the patient and include factors that are both controllable (e.g., playing style, training and preparation, skill) as well as those that are not under the athlete’s control (e.g., age, previous ACL reconstruction, mechanical alignment, soft tissue laxity, hormonal differences, anatomic variation in ACL morphology and intercondylar notch geometry).9–15 Risk for ACL injury is increased by athletic activity that requires pivoting, deceleration, and landing and can be in part related to biomechanical forces including posture, alignment, and differential muscle activation.16 These have led to the development of strength and conditioning programs, which have been designed to mitigate these risk factors and prevent ACL injury and are discussed later in this chapter.12,17–24
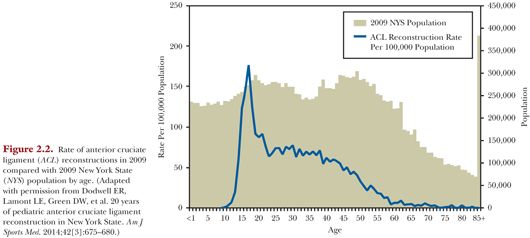
Of the intrinsic risk factors, gender differences have drawn the most interest in the scientific literature. Clinical studies have noted increased rates of ACL tears in young female athletes when compared with males, in the order of 2 to 10 times greater.25–29 Recent large cohort and population-based studies, however, have noted a greater frequency of ACL reconstruction surgery in males compared to females, with a rate of ACL reconstruction up to 15% higher in boys than in girls.9,30 Although the absolute number of males with ACL reconstruction is greater than that of females, females have a higher rate of injury per athletic exposure.1,27–29,31 On average, males experience more athletic exposures than girls, thus leading to a greater number of ACL injuries despite a lower risk per athletic exposure.27,32–36
The cause for females’ higher rate of ACL injury per athletic exposure remains uncertain. Potential explanations include sex hormone receptors located on ACL tissue as well as “quadriceps dominant” muscle activation. Previous studies have shown associations between timing of ACL injury and phase of menstrual period, further implicating hormonal risk factors.37–39 Anatomic risk factors placing girls at higher risk than boys include excessive femoral anteversion, increased Q angle, decreased intercondylar notch width, knee valgus, and increased posterior tibial slope.40–42
Higher socioeconomic status has been associated with increased rates of ACL reconstruction.9 This may be due to differential access to “at-risk” sports or, potentially, may be related to disparities in access to specialist medical care including high-technology imaging such as magnetic resonance imaging (MRI).9 Further study is needed to elucidate specific differences in ACL injury and access to care that may be affected by socioeconomic status.
Extrinsic Risk Factors
Extrinsic risk factors are those that are external to the patient. These include weather conditions, athletic equipment, and footwear–surface interaction. Harder and dryer playing surfaces, cleat configuration, and synthetic playing surfaces can lead to increased strain on the ACL due to an increased coefficient of friction between the shoe and playing surface interface.43,44
Although ACL injury may occur with non–sport-related trauma, 90% of injuries occur during athletic activity.45 Therefore, another modifiable risk factor that places the adolescent athlete at greater risk of ACL injury is participation in competitive sports year-round.46,47 In combination with increased levels of competition and sports specialization as well as improved recognition of ACL injury, this has led to a significant increase in the number of ACL injuries diagnosed in skeletally immature patients.1,2 Additionally, certain sports that involve cutting and pivoting (e.g., American football, wrestling, basketball, soccer) have been found to have higher rates of ACL injury than other sports (e.g., swimming, golf, baseball, softball, volleyball) and therefore patients can decrease their risk by participating in lower risk sports.12,48
EPIDEMIOLOGY OF ANTERIOR CRUCIATE LIGAMENT INJURY COST AND PREVENTION
ACL injury represents a large economic burden with nearly $1.4 billion spent annually on care for these patients. In addition to the financial costs, there are social and emotional hardships as well. Only 40% to 60% of patients of all ages undergoing ACL reconstruction are able to get back to asymptomatic competition, with 10% to 20% unable to return to any competitive sports activity.49–54 Inability to participate in athletic activity can lead to both physical deconditioning as well as negative social and emotional consequences. Prevention of ACL injury may be categorized into two main approaches: screening programs55–59 and preventive training programs.12,17–23,59
Recent meta-analyses evaluated the effectiveness of ACL injury prevention training programs. Those who undergo formal ACL injury prevention training experience an overall ACL injury risk reduction of 62% compared to those who do not participate.17 When stratified by gender, the ACL injury risk reduction was 85% for males and 52% for females.17 The cost of such prevention programs have been estimated to be approximately $1.25 per player per year.18–24,54 Screening tests have also been developed in order to evaluate athletes and stratify them as either high or low risk of injury. Sensitivity and specificity of these tests range from 61% to 78% and 56% to 73%, respectively.54–59 Cost of screening tests for players may be as expensive as $15 per test.54
In a recent cost-effectiveness analysis by Swart et al.,54 it was noted that training all pediatric and adolescent athletes, rather than screening for those at high risk of injury and training only those athletes, was highly cost-effective. They cited the significantly large risk reduction for ACL injury with minimal cost compared to higher costs for imperfect screening tests as the driving force for this finding over such a wide range of clinical scenarios. In the interests of public health and ACL injury prevention, they argue that future resources should be geared toward universally implementing similar training programs rather than screening protocols.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


