Aetiology
Endometriosis in the pelvis is probably a result of retrograde menstruation. More distant foci may result from mechanical, lymphatic or blood-borne spread. As retrograde menstruation is common, but is not always associated with endometriosis, unknown individual factors appear to determine whether the retrograde menstrual endometrium implants and grows. Genetic linkage studies suggest a degree of inherited predisposition (Nat Genet 2011; 43: 51–4). A currently less popular theory is that endometriosis is the result of metaplasia of coelomic cells. It is also not understood why symptoms correlate poorly with the extent of the disease.
Clinical Features
History:
Symptoms are often absent, but endometriosis is an important cause of chronic pelvic pain. This is usually cyclical. Presenting complaints include dysmenorrhoea before the onset of menstruation, deep dyspareunia, subfertility, pain on passing stool (dyschezia) during menses, and, occasionally, menstrual problems. Rupture of a chocolate cyst causes acute pain, and this may be the first symptom. Cyclical haematuria, rectal bleeding or bleeding from the umbilicus are uncommon and suggest severe disease.
Examination:
Common findings on vaginal examination are tenderness and/or thickening behind the uterus or in the adnexa. In advanced cases, the uterus is retroverted and immobile (due to adhesions) and a rectovaginal nodule of endometriosis may be apparent on digital examination and even visible on speculum examination posterior to the cervix if full-thickness vaginally. With mild endometriosis the pelvis often feels normal.
Investigations
Laparoscopy:
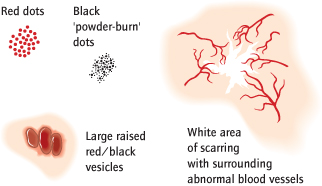
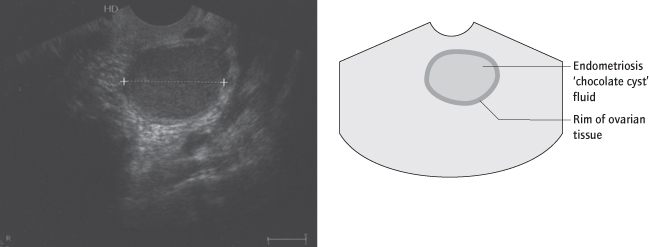
The diagnosis is only made with certainty after visualization ± biopsy, usually at laparoscopy. Active lesions are red vesicles or punctate marks on the peritoneum. White scars or brown spots (‘powder burn’) represent less active endometriosis (Figs 9.2, 9.3), while extensive adhesions and ovarian endometriomas (endometriosis cysts) indicate severe disease. Transvaginal ultrasound is useful to make and to exclude the diagnosis of an ovarian endometrioma (Fig. 9.4) and may also suggest the presence of adenomyosis (although magnetic resonance imaging [MRI] is a better investigation if adenomyosis is suspected). Peritoneal endometriosis will not be visualized on ultrasound scan but may be on MRI. If there is clinical evidence of deeply infiltrating endometriosis, ureteric, bladder and bowel involvement should be assessed with an MRI ± intravenous pyelogram (IVP) and barium studies (RCOG Guideline No. 24, 2006). Serum cancer antigen 125 (CA 125) levels [→ p.44] are sometimes raised but have little diagnostic value.
Fig. 9.3 Laparoscopic view of peritoneal endometriosis: scarring with surrounding abnormal blood vessels.
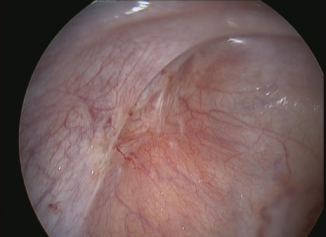
Fig. 9.4 Transvaginal ultrasound photograph of an ovarian endometrioma. The ‘ground glass’ appearance of the altered blood is typical.
The revised American Fertility Society (rev-AFS) grading system is used. At laparoscopy, points are scored dependent on the presence and position of endometriosis deposits and adhesions. The sum of the points allocates the disease extent to one of four grades: Grade 1 (minimal); Grade 2 (mild); Grade 3 (moderate) or Grade 4 (severe). The relationship between disease severity (grade) and symptoms such as pain or infertility is limited. It also takes time to undertake scoring during surgery. Consequently many gynaecologists do not use the system during routine clinical practice, reserving it for research studies.
Symptoms of Endometriosis
None
Dysmenorrhoea
Chronic pelvic pain
Deep dyspareunia
Subfertility
Cyclical bowel or bladder symptoms including pain and/or bleeding
Dyschezia (pain on defaecation)
Dysuria
Differential Diagnosis of Endometriosis
Adenomyosis
Chronic pelvic inflammatory disease [→ p.78]
Chronic pelvic pain [→ p.71]
Other causes of pelvic masses
Irritable bowel syndrome
Management
Endometriosis is a common incidental finding at laparoscopy. In more than 50% of women the disease regresses or does not progress. Asymptomatic endometriosis does not require treatment although consideration should be given to removing endometriomas in view of the (very low) risk of misdiagnosing ovarian cancer. Symptoms should be ascribed to endometriosis with caution and the diagnosis reviewed if treatment does not relieve the patient’s symptoms. Pain that is suggestive of endometriosis can be treated with a therapeutic ‘trial’ of a hormonal drug to suppress ovarian activity and is appropriate without a definitive diagnosis.
Medical
Some women prefer to avoid hormonal therapy and can manage pain symptoms effectively with analgesia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree