End-Tidal Carbon Dioxide Monitoring
Javier A. Gonzalez del Rey
Introduction
Measurement of variations in the respiratory cycle of expired carbon dioxide (CO2) by displayed waveform and by absolute numerical values is defined as capnography and capnometry, respectively. Measurement of exhaled CO2 at the level of the upper airway at the end of the expiration (when CO2 is at its maximum) is referred to as end-tidal CO2 (EtCO2) (1,2,3,4). This noninvasive measurement of blood gases has been used since the 1950s. Initially described by Luft in 1943 (5), it was not until this past decade that its clinical applications made this technique popular in the intensive care unit (ICU) and the operating room (OR). Primitive attempts at crude CO2 measurement were made in the anesthesia suite by the barium hydroxide agglutination reaction and the Einstein CO2 detector, which was capable of sensing 4 to 6 volume percentage (volume %) CO2 (6). Modern technology designed monitors that use infrared absorption spectroscopy to measure the amount of CO2 in an exhaled breath. These sensors may be located in the patient’s artificial breathing circuit (mainstream) or away from the patient as part of the CO2 monitoring circuit system (sidestream).
In the late 1980s, another practical method that documents concentrations of CO2 usually present in the trachea was introduced. It is based on a device that demonstrates colorimetric changes that reflect levels of carbon dioxide above 2%. This technique has been particularly useful for the documentation of endotracheal tube placement in emergency situations and for the assessment of a patient’s respiratory status. Recent studies in urban emergency medical services found that up to 25% of medical and trauma pediatric and adult patients had esophageal intubations on presentation to the emergency department (ED) (7,8). These devices have had a tremendous impact in the rapid detection of unrecognized esophageal intubations in prehospital and hospital settings. Although unrecognized esophageal placement may be rapidly fatal, it is not harmful if it is recognized quickly, especially in prehospital settings (9,10).
Transcutaneous CO2 monitoring, a technique developed in the 1970s primarily for the neonatal intensive care patient, has not proven useful in the ED setting. This is because transcutaneous CO2 measurements take time to calibrate, and skin thickness in older children and adults makes the test inaccurate.
With the development of emergency and transport medicine, EtCO2 measurement has become a very popular and useful tool for monitoring ventilated patients and for confirming endotracheal tube placement. Portable and disposable units have been designed, making the technology user-friendly and less costly.
All critically ill or injured children requiring ventilatory support, in particular where the outcome may be affected by the adequacy of ventilation or special techniques (e.g., cases of acute head trauma and status epilepticus and in the transport of ventilated patients), should ideally be monitored by pulse oximetry and capnography. Thus, physicians, nurses, and respiratory therapists managing these patients in the ED should be familiar with capnography. The American Academy of Pediatrics recommends this type of device to ensure correct placement of the endotracheal tube because other physical findings, such as breath sounds or condensation mist in the endotracheal tube, are more subjective to the clinician (11).
Anatomy and Physiology
Carbon dioxide (CO2), one of the waste products of cellular metabolism, is transported in blood predominantly in the form of bicarbonate ion (60%). One third of CO2 is bound to blood proteins, and the rest is carried as dissolved gas
in plasma (pCO2). The dissolved CO2 concentration in the arterial end of the skin capillaries approximates the pCO2 of an arterial sample. Carbon dioxide then diffuses in lung capillaries to the alveolar unit and enters the gaseous phase. During exhalation, the pCO2 concentration at the end of each breath will be nearly equal to the PaCO2, when the ventilation and perfusion (V/Q) are well matched. EtCO2 represents the approximation of pCO2 from all ventilated alveoli whether or not they are perfused. PaCO2 represents the pCO2 of perfused alveoli. In normal conditions, EtCO2 is 2 to 6 mm Hg less than arterial pCO2 (12).
in plasma (pCO2). The dissolved CO2 concentration in the arterial end of the skin capillaries approximates the pCO2 of an arterial sample. Carbon dioxide then diffuses in lung capillaries to the alveolar unit and enters the gaseous phase. During exhalation, the pCO2 concentration at the end of each breath will be nearly equal to the PaCO2, when the ventilation and perfusion (V/Q) are well matched. EtCO2 represents the approximation of pCO2 from all ventilated alveoli whether or not they are perfused. PaCO2 represents the pCO2 of perfused alveoli. In normal conditions, EtCO2 is 2 to 6 mm Hg less than arterial pCO2 (12).
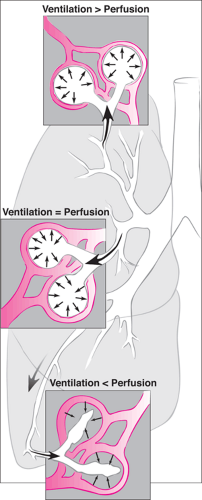
To further understand the EtCO2 concept, it is important to understand the physiology of lung ventilation and perfusion. In normal lungs, the apical segments have a tendency to be more aerated relative to perfusion (Fig. 76.1). At the base, secondary to the opposite phenomenon, the lung is more perfused and not as well aerated. The V/Q constant in most individuals is 0.8 (4 parts ventilation to 5 parts perfusion). The normal respiratory cycle has nonused (or wasted) ventilation. Some of this is alveolar gas that does not get exchanged (alveolar dead space). Other gas travels only within the large or conducting airways and also is not part of the CO2 exchange (large airway dead space). The sum of the alveolar dead space and the large airway dead space is the physiologic dead space. The EtCO2 concentration is related to the arterial carbon dioxide tension (PaCO2), the segmental perfusion of lung units, and the percentage of dead space ventilation.
For example, in cases when pulmonary capillary bed perfusion is less than normal but ventilation is normal, the EtCO2 may significantly underestimate PaCO2. In airways with no perfusion, CO2 will approach zero if ventilation is adequate, whereas perfused airways will diffuse CO2. The net effect is that the EtCO2 will represent the combination of normal and close to zero CO2 diffusion and thereby underestimate PaCO2. Conditions that affect a V/Q mismatch include shock, heart failure, pulmonary emboli or thrombi, cardiac arrest, pneumothorax or hydrothorax, and persistence in a lateral decubitus position. This V/Q mismatch develops because inadequate perfusion to well-ventilated areas results in a widened difference between the arterial pCO2 (PaCO2) and alveolar CO2. In these cases EtCO2 underestimates PaCO2 because of the effect of abnormal perfusion.
A different scenario occurs when the lung has adequate perfusion but inadequate ventilation (shunt perfusion). Conditions that reduce alveolar ventilation or increase the production of carbon dioxide will elevate the arterial CO2, decreasing the V/Q ratio. Although the EtCO2 rises as PaCO2 does from this state, EtCO2 may underestimate PaCO2 because the contribution of dead space ventilation makes it difficult to have a real-time steady-state EtCO2. This is frequently observed in patients with asthma, atelectasis, mucous plugging, right main stem bronchial intubation, emphysema, pneumonia, pleural effusion, and pneumothorax.
During normal respiration, some dead space ventilation travels through the esophagus instead of down the airway. In the proximal esophagus, the measured CO2 closely correlates with the concentration in inhaled air. In patients with tracheal trauma or tracheoesophageal fistulas measured CO2 at esophagus may show concentration closer to that in main airway.
Endotracheal intubation is associated with a complication rate reported to be as high as 26% (13). Unrecognized
esophageal intubation is probably the most serious complications. Utting et al. in 1979 reported that 15% of anesthesia-related accidents resulting in brain injury or death were the result of unrecognized esophageal intubation (14). In the prehospital setting, Stewart et al. and Shea et al. noted a 1.8% and 2% incidence of recognized esophageal intubation, respectively (15,16). In recent years, the colorimetric EtCO2 detector has become available, which indicates the presence of CO2 by a color change. The premise is that with intact pulmonary circulation, CO2 is present in the trachea but not in the esophageal gas reflux. Studies have revealed that the gastric CO2 expired is lower and usually less than 0.7 volume % (mL/100 mL) (17,18). Initially the waveform during esophageal intubations may appear normal, but with successive ventilations (three to six) it dissipates. This occurs even under the influence of carbonated beverage consumption or the presence of antacids in the stomach. Several studies have demonstrated the accuracy and convenient ease of use in animal models, children, and adults in the ED, ICU, and OR and in transport and prehospital settings (19,20,21,22,23).
esophageal intubation is probably the most serious complications. Utting et al. in 1979 reported that 15% of anesthesia-related accidents resulting in brain injury or death were the result of unrecognized esophageal intubation (14). In the prehospital setting, Stewart et al. and Shea et al. noted a 1.8% and 2% incidence of recognized esophageal intubation, respectively (15,16). In recent years, the colorimetric EtCO2 detector has become available, which indicates the presence of CO2 by a color change. The premise is that with intact pulmonary circulation, CO2 is present in the trachea but not in the esophageal gas reflux. Studies have revealed that the gastric CO2 expired is lower and usually less than 0.7 volume % (mL/100 mL) (17,18). Initially the waveform during esophageal intubations may appear normal, but with successive ventilations (three to six) it dissipates. This occurs even under the influence of carbonated beverage consumption or the presence of antacids in the stomach. Several studies have demonstrated the accuracy and convenient ease of use in animal models, children, and adults in the ED, ICU, and OR and in transport and prehospital settings (19,20,21,22,23).
Indications
Indications and uses of capnography are multiple and based on the determination of EtCO2. In the OR, it is used primarily to monitor intubated patients during anesthesia, alerting physicians to inadequate ventilation, ventilatory circuit disconnection, or airway leaks. Most importantly, it can detect inadvertent placement of the endotracheal tube in the esophagus. In the ED, it is used to confirm the proper placement of the endotracheal tube, assess the effectiveness of cardiopulmonary resuscitation, and monitor patients ventilated due to trauma, respiratory failure, or status epilepticus (24). It is important during the delivery of special ventilatory therapy, such as controlled hyperventilation in head trauma. Most recently, esophageal EtCO2 monitoring has been used in the monitoring of patients under conscious sedation for a procedure or diagnostic study and in the evaluation of patients in impending respiratory failure from pneumonia, asthma, and neurologic illness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree