Background
Evidence supports that surgeons are at high risk for work-related musculoskeletal disorders.
Objective
The objective of the study was to compare the effect of different chairs on work-related musculoskeletal discomfort for surgeons during vaginal operations.
Study Design
This crossover study randomly assigned 4 surgeons to 4 chair types using a 4 × 4 Latin square model: a conventional round stool, a round stool with a backrest, a saddle chair with a backrest, and a Capisco chair. Subjective assessments of surgeon discomfort were performed with a validated body discomfort survey, and workload was assessed with the surgical task load index. The objective postural load was quantified with inertial measurement units of the modified rapid upper limb assessment limits. Subjective and objective assessments of chair comfort were performed with an 11 point scale and seat interface pressure–mapped distributions, respectively. The primary outcome was the difference in body discomfort scores between pre- and postsurgery measurements. Secondary outcomes were the differences in chair comfort scores, postural load, and seating interface pressure–mapped distribution. For each outcome, comparisons among the chair types were based on fitting a linear mixed model that handled the surgeon as a random effect and the chair type as a fixed effect.
Results
Data were collected for 48 vaginal procedures performed for pelvic organ prolapse. Mean (SD) duration of surgery was 122.3 (25.1) minutes. Surgeons reported body discomfort during 31 procedures (67.4%). Subjective increase in discomfort from the preoperative state was noted most commonly in the lower back (n = 14, 30.4%), followed by right shoulder (n = 12, 26.1%), upper back (n = 8, 17.4%), hips and buttocks (n = 7, 15.2%), left shoulder (n = 6, 13.0%), right or left thigh (n = 6, 13.0%), and neck (n = 6, 13.0%). Pre- and postsurgery body discomfort scores did not differ with respect to chair type. Chair discomfort scores for the round stool and the saddle chair were significantly higher than the round stool with backrest and the Capisco chair ( P < .001). Although the average modified rapid upper limb assessment postural scores showed moderate to high musculoskeletal risk of neck and shoulder discomfort across the 4 surgeons; chair type did not affect postural scores. The saddle chair had significantly reduced dispersion of seated pressure vs the round stool with backrest ( P ≤ .001), depicted by the number of cells with pressure values >5 mm Hg. An increased dispersion of pressure across the chair surface was associated with increased comfort (Spearman correlation, 0.40, P = .006).
Conclusion
Musculoskeletal strain and associated discomfort for surgeons are very high during vaginal operations. Chair type can affect comfort, and chairs with more uniform distribution and fewer pressure points are more comfortable. However, the chair type used in surgery did not influence the musculoskeletal postural load findings.
Surgeons work in a high-performance environment that demands both physical and mental endurance. The increasing emphasis on patient safety, along with the tremendous cost of preventable adverse events in health care, has made the job of the surgeon further challenging. To adapt to the new challenges, surgeons have subjected themselves to work in poor ergonomic conditions for long periods in the operating room. The resulting fatigue and discomfort may impair their concentration and jeopardize their performance and thereby affect patient safety. A nonergonomic work environment also may result in occupational injuries to surgeons that may affect their career longevity.
Evidence supports that surgeons are at high risk for work-related musculoskeletal disorders. About 88% of surgeons and gynecologists who perform minimally invasive procedures have reported discomfort or pain after performing an operation.
In a survey-based study, Matern and Koneczny reported that 97% of surgeons expressed the need for ergonomic improvements in the operating room. With the prediction of a worsening shortage of surgeons in the United States, as well as an aging surgeon workforce, surgeons may be required to perform operations until older ages. These predictions further emphasize the need for strategies to improve the working environment for surgeons and help minimize occupational injuries.
Despite the extensive prevalence of musculoskeletal disorders among surgeons, the overall awareness of ergonomic techniques in operating rooms is low. The literature of evaluated ergonomic issues in obstetrics and gynecology is further limited. In gynecological surgery, the vaginal route is a traditional approach and involves working in a constrained space and in unfavorable postures for long durations. A survey of gynecological surgeons showed that 86.7% of surgeons performing vaginal surgery experienced work-related musculoskeletal discomfort.
In addition, performance of vaginal operations was the leading cause of backache among gynecologists. Zhu et al objectively measured and quantified postural load of surgeons during vaginal procedures and reported it to be great, especially during vaginal hysterectomy.
We assessed the magnitude of musculoskeletal disorders among gynecologists who perform vaginal surgery and compared the effect of different chair types on work-related musculoskeletal discomfort and load during a procedure.
Materials and Methods
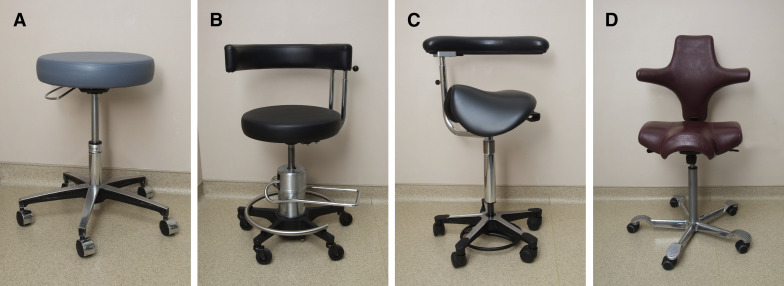
This crossover study randomly assigned 4 gynecologists to use 4 chair types while performing vaginal procedures for pelvic organ prolapse. The chairs studied were the round stool, the round stool with a backrest, the saddle chair with a backrest, and the Capisco chair ( Figure 1 ). The 4 types were randomly assigned to the surgeons using 3 separate 4 × 4 Latin squares. This strategy allowed us to block on surgeon and chair order and to have 3 replications per surgeon-chair combination.
Measurements
Demographic data collected for the participants included age, body mass index, years of surgical experience, handedness, previous injury or illness, average number of surgical operations performed per month, and percentage of time spent performing vaginal or abdominal procedures. The physical activity of an individual surgeon was assessed using the validated World Health Organization Global Physical Activity Questionnaire.
Each surgeon completed a presurgery questionnaire before procedure initiation. This step included a validated tool, the Cornell Musculoskeletal Discomfort Questionnaire, to assess the baseline discomfort status of the surgeon. Before surgery, pressure mats with pressure sensors were placed on the seat pan of each chair. We recorded body postures and movements in the operating room using inertial measurement units (12M, SXT version; APDM, Inc, Portland, OR)
Four inertial measurement units were attached to each surgeon’s body at the forehead, at the upper chest, and on bilateral arms above the elbows. Immediately after the procedures, the surgeons were asked to complete the first postsurgery questionnaire. The surgeons completed the second postsurgery questionnaire the day after the recorded surgery.
The first postsurgery questionnaire asked details of the surgery, including procedure type, duration, an 11 point visual analog scale assessment of comfort of the chair and chair seat pan, the Surgical Task Load Index (to measure the surgical workload), and the modified musculoskeletal discomfort questionnaire (Cornell Musculoskeletal Discomfort Questionnaire).
The Surgical Task Load Index index is a validated tool that measures surgery-specific workload. The second postsurgery questionnaire included the Cornell Musculoskeletal Discomfort Questionnaire.
When the surgeon performed >1 vaginal hysterectomy in a day, only the first case was included in the study. Similarly, when the surgeon performed a vaginal procedure for prolapse on 2 consecutive days, the procedure performed on the second day was not included. This inclusion strategy allowed for a washout period between the interventions and increased the study’s internal validity. When the surgeon performed a vaginal procedure on 2 consecutive days, the surgeon was asked to complete the postsurgery questionnaire early the second day before the upcoming procedure.
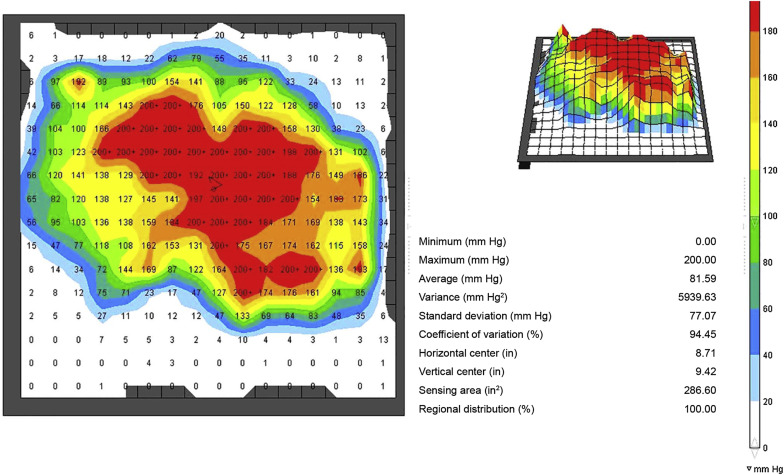
The primary outcome was the difference between the pre- and postsurgery Cornell Musculoskeletal Discomfort Questionnaire ratings that provided a subjective assessment of surgeon discomfort. Secondary outcomes were postural load as measured by inertial measurement units with modified rapid upper limb assessment limits ( Figure 2 ); difference in chair comfort scores as assessed by the 11 point visual analog scale; and seat interface distributions as assessed by pressure mapping ( Figure 3 ).

Postural load using inertial measurement units
Musculoskeletal postural load was objectively assessed and stratified into risk categories by calculating modified rapid upper limb assessment scores for each body part, with the data collected by the inertial measurement units ( Table 1 ). The body angles measured with inertial measurement units were neck flexion and extension, trunk flexion and extension, and bilateral shoulder elevation.
For each procedure, we calculated the percentage of time spent in a specified range of risk categories for each body part ( Table 1 ). These percentages of time were multiplied by the modified rapid upper limb assessment risk score for the specific category, and the products were summed to reach an overall risk score for each body part measured.
Seating interface pressures using pressure mapping
The pressure map reading for each surgical procedure was visually inspected by television for continuity or abnormal readings. The resolution of each mapping session was 256 cells; the range of pressure at each cell was 5–200 mm Hg. Data were extracted from 10 random frames of the final 10 minutes of the pressure mapping. The following values were calculated for each pressure map:
- •
Average pressure, defined as the average pressure of all cells with >5 mm Hg pressure.
- •
Frequency of pressure, defined as the total number of cells with pressure values ≥200 mm Hg.
- •
Surface area, defined as the total number of cells among 256 cells that have values >5 mm Hg. This measurement captures the dispersion of seated pressure across the chair seat pan surface.
- •
Percentage frequency, defined as the percentage of cells with values of ≥200 mm Hg in 1 frame.
The sample size for this project was chosen on the basis of feasibility. Given that 4 surgeons participated and the option of 4 or 5 chairs, we decided on 4 chairs to design the randomization using a 4 × 4 Latin square. The choice of replications per surgeon-chair combination was selected on the basis of the desired replications but without overburdening the participants.
Statistical methods
Statistical analysis was performed using a software package (SAS statistical software, version 9.3; SAS Institute Inc, Cary, NC). For each outcome measure, comparisons between chair types were based on fitting a linear mixed model that handled the individual surgeon as a random effect and the individual chair type as a fixed effect. A square root transformation was applied to the percentage of time spent in risk category 3 or 4 from the inertial measurement unit measurements, before fitting the models.
P values were 2 sided, and values of P < .05 were considered statistically significant. When the overall test for differences among chair types was statistically significant, pairwise comparisons between chair types were evaluated without adjusting for multiple comparisons.
Results
The mean (SD) age of surgeon participants was 43.8 (4.8) years. The 4 surgeons were right-handed and, per the baseline questionnaire, usually operated 2 or 3 days per week and for 5–8 hours on a typical surgery day. Two surgeons preferred the round stool when performing vaginal operations; the other 2 surgeons preferred the round stool with a backrest. Of the surgeons, 3 (75.0%) devoted more than one-half of their total surgical time toward performing vaginal procedures.
The 4 surgeons responded with a somewhat agree when asked whether they were exhausted when they got home from work, and they reported experiencing work-related musculoskeletal discomfort previously. The body parts most commonly involved were neck (100%), lower back (100%), shoulders (75.0%), upper back (75.0%), and fingers or thumb (75.0%).
Factors contributing to the musculoskeletal discomfort were open abdominal operations, vaginal procedures, surgery duration >2 hours, and operating days >6 hours. Although the surgeons denied having any medical condition that may contribute to the discomfort, they admitted seeking medical help for the musculoskeletal discomfort. As per the World Health Organization Global Physical Activity Questionnaire recommendations, the 4 surgeons reported engaging in physical activity of moderate and vigorous intensity for >600 metabolic equivalent minutes per week.
Data were collected on 48 operations performed by 4 surgeons. The mean (SD) case duration was 122.3 (25.1) minutes. The surgeries included vaginal hysterectomy and modified McCall’s culdoplasty (100%), along with anterior colporrhaphy (93.8%), posterior colporrhaphy (83.3%), midurethral sling (35.4%), and suprapubic catheter placement (68.8%). For all dimensions, the mean (SD) surgical task load index score was 39.6 (13.7) on a scale of 0–100.
Surgeons reported experiencing body discomfort (assessed by a modified Cornell Musculoskeletal Discomfort Questionnaire) while performing 31 of the 46 surgeries. (67.4%) Body discomfort was present both before and immediately after surgery ( Figure 4 ). A change in body discomfort score was assessed by calculating the difference between the reported body discomfort ratings from the preoperative state and from immediately after the procedure.
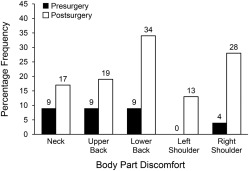
Overall, an increase in body discomfort immediately after the operation was noted most commonly in the lower back (n = 14, 30.4%), followed by right shoulder (n = 12, 26.1%), upper back (n = 8, 17.4%), hips and buttocks (n = 7, 15.2%), left shoulder (n = 6, 13.0%), right or left thigh (n = 6, 13.0%), and neck (n = 6, 13.0%).
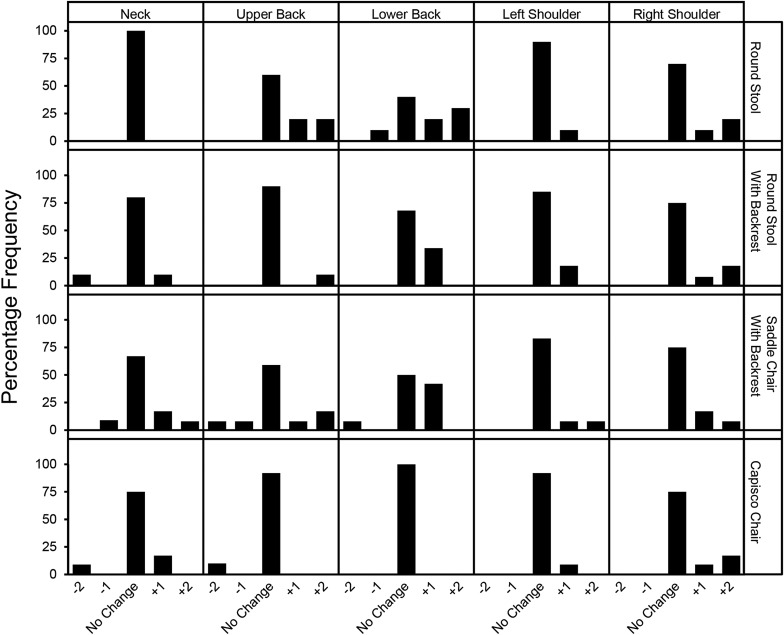
A tendency existed for surgeons to have increased upper back discomfort after using the round stool compared with the Capisco chair and increased lower back discomfort after using either of the round stools compared with the Capisco chair ( Figure 5 ). However, these comparisons, as well as all other chair comparisons, did not reach statistical significance.