Background
Cesarean scar pregnancy (CSP) is a serious complication of pregnancy, which consists of implantation of the gestational sac in the hysterotomy scar. This condition is increasing in frequency and often poses a diagnostic challenge. Its diagnosis is dependent on visual assessment of the uterus on the longitudinal sagittal ultrasound plane. Misdiagnosing a low intrauterine chorionic sac as a CSP, or a true scar pregnancy as an intrauterine pregnancy (IUP), may lead to adverse outcomes including hysterectomy.
Objective
The objective of the study is to describe a sonographic method for the differential diagnosis of CSP vs IUP in early gestation. The current study tests the hypothesis that on a first-trimester ultrasound performed between 5-10 weeks of gestation, the relative location of the center of gestational sac to the midpoint of the uterus along a longitudinal line between the external cervical os and the fundus can be used for early detection of CSPs.
Study Design
This is a retrospective review of electronically archived ultrasound images of IUP and CSP between 5-10 weeks of gestation. A total of 242 ultrasound images were analyzed: 185 cases of normal IUPs (including 128 in anteverted uteri, 31 in retroverted uteri, and 26 IUPs with history of cesarean delivery) and 57 cases of CSPs diagnosed from 2004 through 2015 in a single institution. The following measurements were made for each case: distance from the external cervical os to the uterine fundus, the midpoint axis of the uterus, the distance from the external cervical os to the center of gestational sacs, and the distance from the external cervical os to the most distant edge of the gestational sacs from the cervix.
Results
The location of the center of the gestational sac relative to the midpoint axis of the uterus between 5-10 weeks of gestation differentiated between IUP and CSP (mean 17.8 vs –10.6 mm, respectively, P = .0001), indicating that most CSPs are located proximally to the midpoint axis of the uterus whereas most normal IUPs are located distally from the midpoint of the uterus. Using location of the center of the gestational sac as a marker of CSPs between 5-10 weeks of gestation yielded the following characteristics of diagnostic accuracy: sensitivity 93.0% and specificity 98.9%. The likelihood ratio of the positive test was 84.5. The likelihood ratio of the negative test was 0.07.
Conclusion
The location of the center of the gestational sac relative to the midpoint axis of the uterus can be used as an easy method for sonographic differentiation of IUP and CSP between 5-10 weeks of gestation.
Introduction
The cesarean delivery (CD) rate in the United States has increased by approximately 40% in the last 2 decades, and in 2014 the Centers for Disease Control and Prevention reported a CD rate of 32.2%. A serious complication of pregnancy after CD is the implantation of the gestational sac in the hysterotomy scar, known as a cesarean scar pregnancy (CSP). CSP is increasing in frequency and is often difficult to diagnose. A scar pregnancy often invades the myometrium and morphs into the known clinical expression of morbidly adherent placenta such as placenta accreta, increta, and percreta. The progressive deep invasion of the placenta is life-threatening and may lead to severe obstetrical complications such as profuse hemorrhage, uterine dehiscence/rupture, or premature delivery throughout all 3 trimesters of the gestation. The early diagnosis of this life-threatening obstetrical complication would be valuable to adequately manage patients.
The current criteria for diagnosing a CSP are: an empty uterus and cervical canal with a clearly demonstrated endometrium; and a gestational sac located at the anterior wall of the uterine isthmic portion surrounded by the myometrium and fibrous tissue of the scar and separated from the endometrial cavity or fallopian tube. In a commentary within an article by Comstock and Bronsteen, El Refaey et al point to “fundal vs nonfundal or low pregnancy implantation” of the CSP and call for universal first-trimester sonographic scan in patients with previous CD for early detection of CSP.
The current study addressed the hypothesis that on a first-trimester ultrasound performed between 5-10 completed weeks of gestation, the relative location of the center of gestational sac to the midpoint of the uterus along a longitudinal line between the external cervical os and the fundus can be used for early detection of CSP. The purpose of the study is to describe a sonographic method for the differential diagnosis of CSP vs intrauterine pregnancy (IUP) in early gestation.
Materials and Methods
This is a retrospective review of images and medical records to assess the previously recorded and electronically archived images of IUPs and CSPs between 5-10 weeks of gestation. Our sonographic and clinical criteria for the diagnosis of CSP were previously published and applied to the CSP cases in this study. The diagnosis of CSP was made at the first ultrasound scan of the referred patients in both centers. The diagnosis of CSP was made at the first ultrasound scan of the referred patients in both centers. Longitudinal sagittal images of each uteri were selected and the following eligibility criteria had to be met: (1) the entire uterus with its fundal and cervical contour as well as the gestational/chorionic sac clearly visible on the ultrasound image; and (2) adequate follow-up period at least to the end of the first trimester proving that their diagnosis was subsequently confirmed as an IUP or in the case of a CSP, until the diagnosis was confirmed by the accepted sonographic criteria. The study was approved by the New York University Institutional Review Board.
A total of 242 ultrasound images were analyzed: 185 cases of normal IUPs (including 128 in anteverted uteri, 31 in retroverted uteri, and 26 IUPs with history of CD) collected in 2014 and 57 consecutive cases of CSP diagnosed at the New York University Medical Center and at Arnas Civico Hospital, Palermo, Italy, between January 2004 and December 2015.
Once the images were assigned to the respective groups, paper prints were obtained and their evaluation was as follows:
- 1.
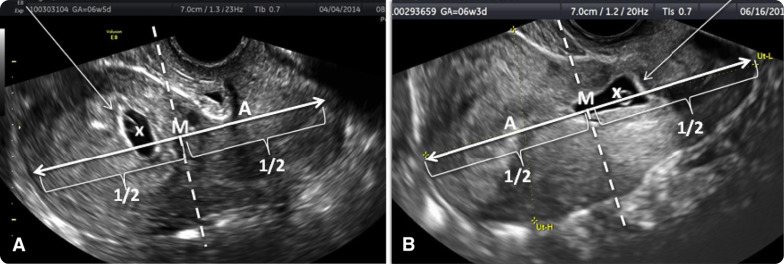
On each image of uteri a straight longitudinal line was drawn connecting the external os of the cervix and the uterine fundus. The distance between the cervix and the fundus was measured (in millimeters) using a protractor. This measurement represented the uterine size (distance A). On the same image the midpoint section of the uterine size was marked by a line that transected the above line by half (M = A/2) at 90 degrees. This point was called midpoint of uterus ( Figure 1 ).
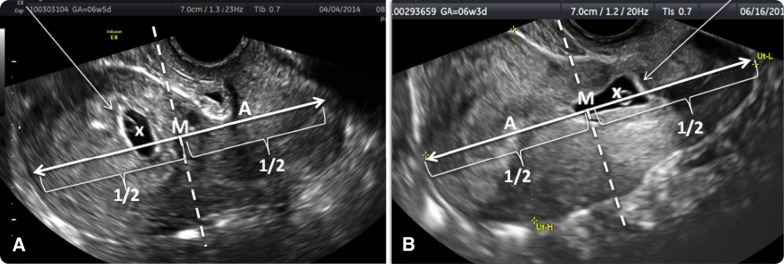
Figure 1
Sonographic differential diagnosis of intrauterine and cesarean scar pregnancy
Proposed method to differentiate intrauterine pregnancy (IUP) from cesarean scar pregnancy (CSP) based on study. Dotted line represents uterine size (distance A). Solid line drawn at right angle to dotted line marks middle of uterine size (M). Gestational sac (arrow) is between midpoint of A , uterus and uterine fundus, indicating IUP, or B , uterine size and cervix, indicating CSP.
Timor-Tritsch et al. Differential diagnosis of cesarean scar pregnancy. Am J Obstet Gynecol 2016 .
- 2.
The external cervical os and the center of all gestational sacs were visually determined and marked.
- 3.
The distance from the external cervical os to the center of the gestational sac (distance B) was measured (in millimeters) using the protractor. This represented the distance and the location of the sac in relation to the cervix and was termed “cervix-to-center-of-sac distance” ( Figures 2 and 3 ). The distance between the center of gestational sac and the midpoint axis of the uterus was calculated (B-M).
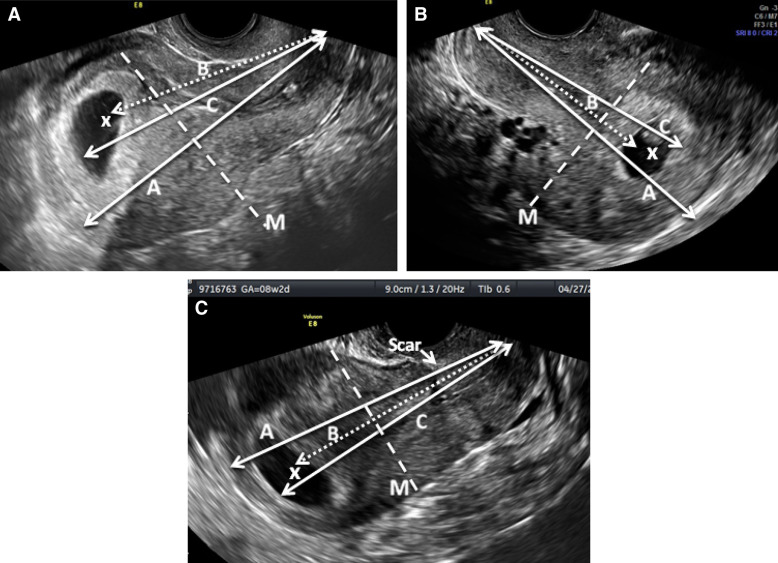
Figure 2
Use of three different measurements to define the gestational sac in intrauterine pregnancies
Measurements in normal intrauterine pregnancies. Anteverted uterus A , without and C , with previous cesarean delivery (CD). B , Retroverted uterus without previous CD. Solid lines A defines the uterine size in the sagittal view from the cervix to the uterine fundus. Dotted lines represent distance from cervix to center of gestational sac (x) (distance B). Solid lines represent distance from cervix to most distant edge of gestational sac (distance C).
Timor-Tritsch et al. Differential diagnosis of cesarean scar pregnancy. Am J Obstet Gynecol 2016 .
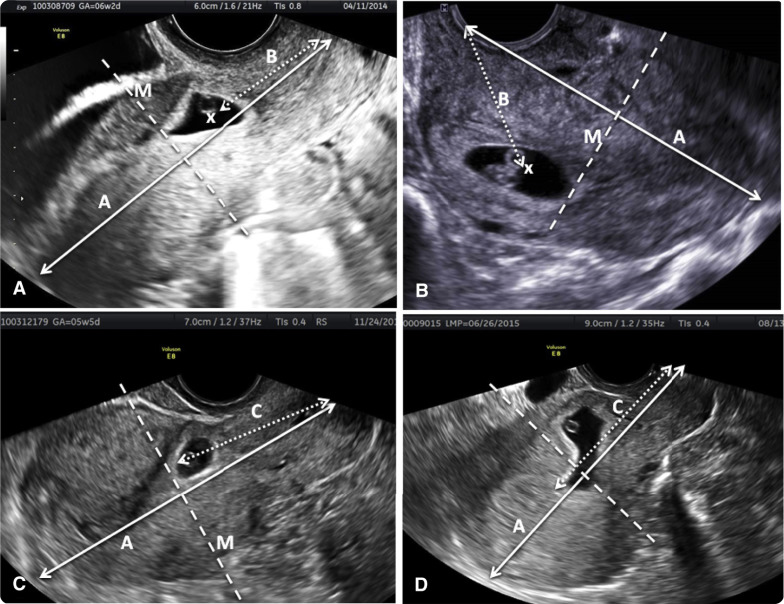
Figure 3
Use of 2 different measurements to define the gestational sac in cesarean scar pregancies
Measurements in cesarean scar pregnancies. Solid line represents distance between external cervical os and uterine fundus on sagittal longitudinal ultrasound image of uterus (uterine size) (distance A). A and C , Anteverted uterus. B and D , Retroverted uterus. Dotted line represents distance from cervix to: A and B , center of gestational sac (x) (distance B); or C and D , distal edge of gestational sac (distance C).
Timor-Tritsch et al. Differential diagnosis of cesarean scar pregnancy. Am J Obstet Gynecol 2016 .
- 4.
The most distant edge of the gestational sac from the external cervical os was also marked to calculate the distance from the external cervical os to the most distant edge of the gestational sac.
- 5.
The distance from the external cervical os to the most distant edge of the gestational sac (distance C) was measured (in millimeters) using the protractor. This represented the furthest boundary of the sac in relation to the cervix and was termed “cervix-to-most-distant-edge-of-sac distance” ( Figures 1 and 2 ).
- 6.
The distance between the most distal edge of the gestational sac and the midpoint axis of the uterus was calculated (C-M).
The above-mentioned distances were determined for each group and subgroups. The gestational ages of each pregnancy were recorded in weeks and days from the last menstrual period.
Statistical analysis
The differences between comparison groups were assessed using analysis of variance test and nonparametric Kruskal-Wallis test for continuous variables. The sensitivity, specificity, and likelihoods of positive and negative test for CSP were calculated separately based on the location of the center of gestational sac and the most distal edge of the gestational sac relative to the midpoint axis of the uterus. The statistical analyses were performed using statistical software (SPSS, Version 21.0; IBM Corp, Armonk, NY).
Materials and Methods
This is a retrospective review of images and medical records to assess the previously recorded and electronically archived images of IUPs and CSPs between 5-10 weeks of gestation. Our sonographic and clinical criteria for the diagnosis of CSP were previously published and applied to the CSP cases in this study. The diagnosis of CSP was made at the first ultrasound scan of the referred patients in both centers. The diagnosis of CSP was made at the first ultrasound scan of the referred patients in both centers. Longitudinal sagittal images of each uteri were selected and the following eligibility criteria had to be met: (1) the entire uterus with its fundal and cervical contour as well as the gestational/chorionic sac clearly visible on the ultrasound image; and (2) adequate follow-up period at least to the end of the first trimester proving that their diagnosis was subsequently confirmed as an IUP or in the case of a CSP, until the diagnosis was confirmed by the accepted sonographic criteria. The study was approved by the New York University Institutional Review Board.
A total of 242 ultrasound images were analyzed: 185 cases of normal IUPs (including 128 in anteverted uteri, 31 in retroverted uteri, and 26 IUPs with history of CD) collected in 2014 and 57 consecutive cases of CSP diagnosed at the New York University Medical Center and at Arnas Civico Hospital, Palermo, Italy, between January 2004 and December 2015.
Once the images were assigned to the respective groups, paper prints were obtained and their evaluation was as follows:
- 1.
On each image of uteri a straight longitudinal line was drawn connecting the external os of the cervix and the uterine fundus. The distance between the cervix and the fundus was measured (in millimeters) using a protractor. This measurement represented the uterine size (distance A). On the same image the midpoint section of the uterine size was marked by a line that transected the above line by half (M = A/2) at 90 degrees. This point was called midpoint of uterus ( Figure 1 ).