Micturition
Micturition results when bladder pressure exceeds urethral pressure. This is achieved voluntarily by a simultaneous drop in urethral pressure (partly due to pelvic floor relaxation) and an increase in bladder pressure due to a detrusor muscle contraction.
Incontinence
Essentially there are two main causes of female incontinence:
Uncontrolled increases in detrusor pressure increasing bladder pressure beyond that of the normal urethra. ‘Overactive bladder’ (OAB) or ‘urinary urge incontinence’, previously called ‘detrusor instability’, is the most common cause of this mechanism.
Increased intra-abdominal pressure transmitted to bladder but not urethra, because the upper urethra neck has slipped from the abdomen. Bladder pressure therefore exceeds urethral pressure when intra-abdominal pressure is raised, for example when coughing. ‘Urinary stress incontinence’ is the most common cause of this mechanism.
Rarer causes include urine bypassing the sphincter through a fistula or the pressure of urine overwhelming the sphincter due to overfilling of the bladder due to neurogenic causes or outlet obstruction: ‘overflow incontinence’.
Common Urinary Symptoms
Urinary incontinence is the complaint of involuntary urinary leakage, which can be divided, broadly, into stress incontinence and urge incontinence.
Daytime frequency is the number of times a women voids during her waking hours. This should normally be between 4 and 7 voids per day. Increased daytime frequency is defined as occurring when a patient perceives that she voids too often by day.
Nocturia is the complaint of having to wake at night one or more times to void. Up to the age of 70 years, more than a single void is considered abnormal.
Nocturnal enuresis is urinary incontinence occurring during sleep.
Urgency is the sudden compelling desire to pass urine, which is difficult to defer. Urgency is most frequently secondary to detrusor overactivity, although inflammatory bladder conditions such as interstitial cystitis may also present with this.
Bladder pain is felt suprapubically or retropubically. Typically, pain occurs with bladder filling and is relieved by emptying it. Pain is indicative of an intravesical pathology, such as interstitial cystitis or malignancy, and warrants further investigation.
Urethral pain is pain felt in the urethra.
Dysuria is pain experienced in the bladder or urethra on passing urine. It is most frequently associated with urinary tract infections.
Haematuria is the presence of blood in the urine. This can be microscopic or macroscopic (frank). It is always significant and always warrants further investigation.
Investigation of the Urinary Tract
Urine Dipstick Tests:
Urine dipstick testing for blood, glucose, protein leucocytes and nitrites is essential whenever a patient presents with urinary symptoms. Nitrites suggest the presence of infection: if positive, a urine sample is sent for microscopy and culture to confirm infection and the type and antibiotic sensitivity of the organism(s). Glycosuria suggests diabetes; haematuria suggests bladder carcinoma or calculi.
Urinary Diary:
The patient keeps a record for a week of the time and volume of fluid intake and micturition. This gives invaluable information about drinking habits, frequency and bladder capacity.
Postmicturition Ultrasound or Catheterization:
These exclude chronic retention of urine.
Urodynamic Studies, Cystometry:
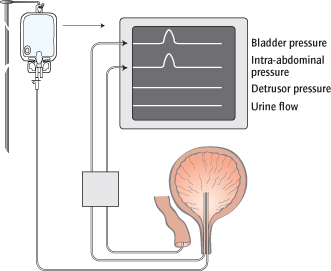
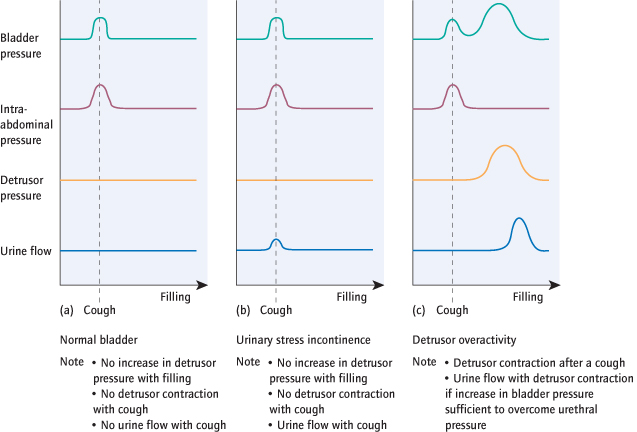
These are necessary prior to surgery for stress incontinence or for women whose overactive bladder symptoms do not respond to medical therapy. Urodynamics may be performed with or without video imaging. Cystometry directly measures, via a catheter, the pressure in the bladder (vesical pressure) whilst the bladder is filled and provoked with coughing. A pressure transducer is also placed in the rectum (or vagina) to measure abdominal pressure (Fig. 8.2). The true detrusor pressure (i.e. the pressure generated by true contraction of the detrusor muscle) can be automatically calculated by subtracting the abdominal pressure from the vesical pressure. The detrusor pressure does not normally alter with filling or provocation (raised intra-abdominal pressure). If leaking occurs with coughing, in the absence of a detrusor contraction, then the problem is likely to be ‘urodynamic stress incontinence’ (USI). If an involuntary detrusor contraction occurs, ‘detrusor overactivity’ is diagnosed. Initially, the patient experiences urgency and then incontinence if bladder pressure is increased beyond that of the urethra. Cystometry is widely used to investigate symptoms of urinary incontinence as both USI and detrusor overactivity can cause leakage with exertion, but their treatments are very different.
Ultrasonography:
excludes incomplete bladder emptying, check for congenital abnormalities, calculi, tumours and detects cortical scarring of the kidneys.
Abdominal X-ray diagnoses conditions such as foreign bodies and calculi.
Computed Tomography (CT) Urogram:
With the use of contrast, the integrity and route of the ureter is examined.
Methylene Dye Test:
Blue dye is instilled into the bladder. Leakage from places other than the urethra, i.e. fistulae, can be seen.
Cystoscopy:
Inspection of the bladder cavity is useful to exclude tumours, stones, fistulae and interstitial cystitis but gives little indication of bladder performance.
Urinary Stress Incontinence
Definition
Urinary stress incontinence is a complaint of involuntary leakage of urine on effort or exertion, or on sneezing or coughing. When confirmed on urodynamic studies it is called urodynamic stress incontinence (USI). It is commonly arises as a result of urethral sphincter weakness. The diagnosis can only be made with certainty after excluding an overactive bladder using cystometry (Fig. 8.3).
Epidemiology
Stress incontinence accounts for almost 50% of causes of incontinence in the female and occurs to varying degrees in more than 10% of all women.
Aetiology
Important causes of stress incontinence include pregnancy and vaginal delivery, particularly prolonged labour and forceps delivery, obesity and age (particularly postmenopausal). Prolapse commonly coexists but is not always related. Previous hysterectomy (not for prolapse or urine symptoms) may predispose to USI (Lancet 2007; 370: 1494).
Mechanism of Incontinence
When there is an increase in intra-abdominal pressure (‘stress’), the bladder is compressed and its pressure rises. In the normal woman, the bladder neck is equally compressed so that the pressure difference is unchanged. However, if the bladder neck has slipped below the pelvic floor because its supports are weak, it will not be compressed and its pressure remains unchanged (Fig. 8.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree