Disorders of the Breast
Mary L. Gemignani
Breast cancer remains the most common cancer in women and is second only to lung cancer as the leading cause of cancer-related death in the United States. It is estimated that in 2006, there will be 212,920 new cases of breast cancer diagnosed in women and 40,970 cancer-related deaths. The lifetime risk among women of developing breast cancer is 12.5% (1 in 8); the lifetime risk of dying from breast cancer is 3.6% (1 in 28). Although breast cancer remains a serious health concern in the United States, as well as in other countries, breast cancer mortality is declining. This decline is thought to be secondary to increased use of mammographic screening and early detection of breast cancer.
Obstetricians and gynecologists are commonly the primary care physicians for many women. According to the American College of Obstetricians and Gynecologists (ACOG), the diagnosis of breast disease, as well as the education of women on breast self-examination and their referral for mammographic screening, is central to the obstetrician–gynecologist’s role in women’s health care.
This chapter presents an overview of breast cancer screening, benign and malignant conditions of the breast, and the role of the obstetrician–gynecologist in the diagnosis of and education of women about breast disease.
Anatomy of the Breast
The adult breast lies between the second and sixth ribs in the vertical plane and between the sternal edge (medially) and midaxillary line (laterally). The average breast measures 10 to 12 cm in diameter and is 5 to 7 cm in thickness. It is concentric, with a lateral projection into the axilla named the axillary tail of Spence.
The breast consists of three major structures: skin, subcutaneous fatty tissue, and breast tissue (parenchyma and stroma). The skin contains hair follicles, sebaceous glands, and eccrine sweat glands. The glandular breast is divided into 15 to 20 segments (lobes) that are separated by connective tissue and converge at the nipple in a radial arrangement. These lobes are made up of 20 to 40 lobules, which in turn consist of 10 to 100 alveoli (tubulosaccular secretory units). Five to ten major collecting milk ducts drain each segment and open at the nipple into subareolar lactiferous sinuses.
A superficial pectoral fascia envelops the breast; the undersurface of the breast lies on the deep pectoral fascia. Between these two fascial layers are fibrous bands known as Cooper suspensory ligaments, which provide support for the breast. The space between the deep layers of the superficial fascia of the breast and the deep investing fascia of the pectoralis is the retromammary bursa.
The epidermis of the nipple (mammary papilla) and areola is pigmented and wrinkled and consists of keratinized, stratified squamous epithelium that contains smooth muscle fibers in dense connective tissue. These fibers are responsible for the erection of the nipple. Two receptor-type nerve endings (Ruffini-like bodies and end bulb of Krause) are present on the nipple and are associated with the tactile reception of stretch and pressure.
The areola has no hair follicles; it has sebaceous glands (at its margin), apocrine sweat glands, and accessory areolar glands (Montgomery glands) that open on the surface of the areola as small elevations called Morgagni tubercles.
The blood supply of the breast is mostly from superficial vessels. The principal blood supply is derived from the internal thoracic (mammary) and lateral thoracic artery and their tributaries. The posterior intercostal arteries of the second to fourth intercostal spaces also give off tributaries known as the mammary branches.
The superficial veins follow the arteries and drain through perforating branches of the internal thoracic vein, tributaries of the axillary vein, and perforating branches of posterior intercostal veins. The veins anastomose circumferentially around the nipple, which is named the circulus venosus.
Epidemiology of Breast Cancer
Risk Factors and Assessment
Age
The incidence of breast cancer increases with age. Age is the most significant risk factor for breast cancer.
Family History
Hereditary breast cancers account for 5% to 10% of all breast cancers and are thought to be attributable to highly penetrant mutations in breast cancer–susceptibility genes. Two such tumor-suppressor genes, BRCA1 and BRCA2, have been well characterized. Breast cancer has also been noted to occur in association with other cancers, such as in Li-Fraumeni syndrome and Cowden syndrome.
Personal History
A patient’s history of prior breast biopsy is important. Although the number of breast biopsies undergone does not increase a woman’s risk of breast cancer, certain pathologic entities do play a role. Atypical ductal or lobular hyperplasia and lobular carcinoma in situ (LCIS) are considered markers of increased risk of developing invasive breast cancer. A personal history of breast cancer increases the risk for development of another breast cancer. Women treated for breast cancer are at risk for the development of a contralateral breast cancer. Various studies have shown this risk to be between 0.5% and 1.0% per year. In addition, patients treated with breast conservation (lumpectomy and radiation therapy) are at risk for an ipsilateral recurrence. In these women, this risk could be 10% or higher at 10 years post-treatment.
Reproductive History
Early menarche, late menopause, and nulliparity are thought to be risk factors for breast cancer. Age at first pregnancy is also thought to be a relative risk (RR) factor for breast cancer. Early age at first pregnancy is often associated with a lower risk for breast cancer; pregnancy by the age of 30 may reduce risk by up to 30%, and a full-term pregnancy by the age of 20 reduces risk by 50%. Breast-feeding has been reported to reduce risk of breast cancer, and the greatest effect is seen when cumulative times exceed 24 months. The effect of menopause as it relates to breast cancer risk has been examined. Late menopause poses an increase in risk of breast cancer. Bilateral oophorectomy before natural menopause has been reported to reduce risk of breast cancer.
Exogenous Hormone Use
The role of exogenous estrogens in the promotion of breast cancer is still controversial. Studies of oral contraceptive pills (OCPs) and hormone replacement therapy (HRT) have yielded conflicting results. Studies of HRT and breast cancer risk indicate that women who are currently using HRT are at increased risk for breast cancer development. A meta-analysis of the largest studies, however, suggests that the increased risk is only about 10%. Women who have taken HRT in the past but are not currently using HRT are not at increased risk. Long-term use of HRT (>10 years) has been associated with relative increase in breast cancer risk, and the highest risk was noted in those patients using HRT with progestins (RR 1.41). Of note, multiple studies have shown that patients who develop breast cancer while on HRT have smaller, less aggressive cancers and a lower risk of death from breast cancer.
Recently, results from the Women’s Health Initiative (WHI) randomized controlled trial were reported. Between 1993 and 1998, 16,609 women with an intact uterus were randomized to receive combination HRT (0.625 mg per day of conjugated equine estrogens and 2.500 mg per day of medroxyprogesterone acetate) versus placebo. The planned duration of the trial was 8.5 years; however, the data and safety monitoring board of the committee recommended halting the trial because the incidence of invasive breast cancer had exceeded the stopping boundary that had been set at the initiation of the trial. This occurred after a mean of 5.2 years of follow-up. The increased risk of breast cancer–reported hazard ratio (HR) was 1.25 (95% confidence interval [CI] 1.00 to 1.59). There was also a reported increased risk of coronary heart disease (HR 1.29; 95% CI 1.02 to 1.63), and stroke (HR 1.41; 95% CI 1.39 to 3.25). Beneficial effects included decreased risk of colorectal cancer (HR 0.63; 95% CI 0.43 to 0.92) and hip fracture (HR 0.66; 95% CI 0.45 to 0.98). Based on the data, the safety monitoring board initially did not recommend stopping the estrogen-alone arm in women who had had a hysterectomy. Results of the estrogen-only arm of the WHI study have been reported. The study included 10,739 postmenopausal women (aged 50 to 79 years) with prior hysterectomy. These women were randomized to receive 0.625mg per day of conjugated equine estrogen or placebo. In February 2004, the National Institutes of Health (NIH) decided to terminate the intervention phase of the estrogen-only study, which had been scheduled for a close-out interval of October 2004 to March 2005. With an average follow-up of 6.8 years, there was an increased risk of stroke (HR 1.39; 95% CI 1.10 to 1.77), a decreased risk of hip fracture (HR 0.61; 95% CI 0.41 to 0.91), and no effect on coronary heart disease incidence (HR 0.91; 95% CI 0.75 to 1.12). The investigators noted a possible reduction in breast cancer risk (HR 0.77; 95% CI 0.59 to 1.01) that warrants further investigation.
The annual increased risk for an individual woman is still relatively small. The increased risk for breast cancer is apparent after 4 years of HRT use. The ACOG stresses the importance of addressing the reasons for initiating or continuing on HRT. It is no longer recommended to prevent heart disease in healthy women (primary prevention) or to protect women with pre-existing heart disease
(secondary prevention). In addition, it is no longer recommended solely for prevention of osteoporosis.
(secondary prevention). In addition, it is no longer recommended solely for prevention of osteoporosis.
HRT is highly effective in treating vasomotor symptoms with limited effective alternative therapies. In this setting, short-term use (<5 years) can be considered, as data on short-term use does not show an increased association with breast cancer. A recent study surveyed attitudes of obstetricians and gynecologists toward hormone therapy after the WHI results were published. Respondents to the survey remained skeptical of the results; 49.1% did not find them convincing. There was strong support for the use of HRT for vasomotor symptoms, vaginal dryness, and osteoporosis, but most of the physicians that were surveyed did not find it useful for prevention of cardiovascular disease or dementia.
In the past, most studies addressing OCP use and breast cancer risk concluded that there was a significant increase in risk associated with OCP use. However, the majority of studies regarding OCP use and breast cancer risk have demonstrated little association with breast cancer incidence rates. In women who have used OCP for extended periods of time (>10 years), a minimal, nonsignificant increase in breast cancer cases has been reported, seen most commonly in the group of women who began using OCP at a young age (<20 years). Past or present use of OCP at the time of diagnosis of breast cancer does not affect mortality from breast cancer. The presence of a family history of breast cancer does not appear to further increase the risk of breast cancer associated with either OCP or HRT use.
Prior Exposure to Radiation Therapy
Exposure to ionizing radiation, such as that which occurs in treatment with mantle radiation for Hodgkin’s disease, poses a risk for breast cancer. This is noted 7 to 10 years after completion of radiation therapy. The cumulative probability of breast cancer at age 40 approaches 35% in these women. The risk of breast cancer associated with radiation exposure decreases with increasing age at exposure.
Other Factors
Breast cancer is more frequent in Jewish women than in non-Jewish women and in black women more often than in white women. Asian women have a low incidence of breast cancer. Japanese women show lower rates of breast cancer than white women. Although postmenopausal breast cancer is less common in Japanese women who have migrated to Western countries than among the general populations of these countries, after two or three generations, the incidences of breast cancer in these women approaches that of white women. The Western diet, with its increased intake of animal fat, has been implicated in these studies.
Alcohol consumption has been reported to increase breast cancer risk in a dose-related manner. Women who drink approximately one drink per day have slightly elevated risk of breast cancer over nondrinkers. This risk is significantly higher with moderate to high alcohol consumption (two to five drinks per day).
Relative Risk
RR is a ratio that depicts the likelihood over time of an event’s occurrence in a study population relative to that in a reference population. It is often used to quantify risk factors for breast cancer. Absolute risk is a percentage that depicts the likelihood over time of the occurrence of an event. For rare events, these two are the same, but for common events they are not. It is best to discuss risk with patients in terms of absolute risk rather than RR.
Several models exist to estimate a woman’s risk of breast cancer. The Gail model, developed for use in the National Surgical Adjuvant Breast and Bowel Project (NSABP P-1) Breast Cancer Prevention Trial, is available from the National Cancer Institute (NCI) and provides a measurement of absolute risk over time for breast cancer. However, in familial-type hereditary cases, it underestimates the risk of breast cancer by overlooking age at onset, bilaterality of disease among affected family members, and breast cancer in non-first-degree relatives (Table 56.1).
BRCA1 and BRCA2
BRCA1 and BRCA2 are breast cancer–susceptibility genes that have expanded our knowledge of familial breast cancer. Linkage studies done in 1990 in early-onset breast cancer families led to cloning of the BRCA1 gene at the University of Utah in Salt Lake City in 1994. The BRCA1 gene consists of 22 coding exons distributed over approximately 100 kb of genomic DNA on chromosome 17q21. It is thought to be responsible for approximately 45% of early-onset hereditary breast cancers and nearly 90% of hereditary ovarian cancers in families with a high incidence of breast and ovarian cancers. Two specific mutations, 185delAG and 5382insC, are present in approximately 1.00% and 0.25% of the Ashkenazi Jewish population, respectively. They are thought to be founder mutations (i.e., an altered gene or genes seen with a high frequency in a population originating from a small ancestral group, one or more of the founders of which were carriers of the mutant gene).
BRCA2 was isolated on chromosome 13q12–13 in 1995. The BRCA2 gene is composed of 26 coding exons distributed over approximately 70 kb of genomic DNA. This gene appears to account for 35% of families with early-onset breast cancer. It confers a lower risk of ovarian cancer compared with that found in breast cancer. A single mutation, 6174delT, is found in approximately 1.4% of the Ashkenazi Jewish population. Together, both BRCA1 and BRCA2 mutations are found in approximately 1 in 40 Ashkenazi Jewish individuals. For both genes, the estimated penetrance is 70% to 90% for breast cancer by age 70, but the risk of breast cancer by age 50 may be lower for BRCA2 mutations.
TABLE 56.1 Breast Cancer Risk Factors | ||
|---|---|---|
|
The likelihood of a patient having a BRCA1 or BRCA2 mutation is dependent on certain factors such as age at the time of diagnosis of breast or ovarian cancer and the number and age of first- and second-degree relatives in the same parental lineage and ethnicity with breast or ovarian cancer. The parental lineage can be either maternal or paternal. The American Society of Clinical Oncology has issued guidelines for recommending genetic testing for families with high probability (>10%) of having a mutation for BRCA1 (Table 56.2).
Identification of patients with a high-risk family history should be referred for genetic counseling and testing. The decision to undergo genetic testing is a complex one, as it can affect an individual’s personal, psychologic, social, financial, and ethical well-being.
Women who have a negative genetic test should still be considered at risk on the basis of age and environment and because of the possibility of other genetic factors or unknown mutations.
TABLE 56.2 American Society of Clinical Oncology Guidelines for Recommending Genetic Testing for Families with High Probability (>10%) of Having BRCA1 Mutation | |
|---|---|
|
History and Physical Examination
Obtaining a thorough history, including a family history and information on menstrual status, pregnancies and lactation, hormone use, prior breast surgeries, and trauma, is essential. In addition, ascertaining whether the patient performs breast self-examinations, as well as the presence and characterization of nipple discharge or a breast mass, is important.
Bilateral breast examination is best performed following menstruation and prior to ovulation. At this time, breast engorgement and tenderness is less likely to be present. A multipositional breast examination should be performed, including examination in the upright and supine positions (Figs. 56.1, 56.2). Breast retraction and subtle changes in the skin and nipple may be missed if the patient is examined in only one position. Examination should be performed with hands at sides; with hands elevated above the head; and finally, with the arms tensed at the waist (contracting the pectoralis muscles). Attention is directed toward the supraclavicular area and axilla. Digital palpation is performed beneath the lateral pectoralis muscles into the axilla itself.
The second phase of the breast examination is conducted with the patient in the supine position. Digital palpation is carried out by using the index and middle fingers and applying varying amounts of pressure with the flats or pads of the fingers. A thorough examination systemically covers the entire breast and chest wall. The examination can be done in a clockwise direction or by rows (stripwise). It is important to carefully examine beneath the nipple–areolar complex and within the axilla.
An inflammatory appearance of the breast should raise suspicion of an inflammatory carcinoma. The classic appearance of inflammatory breast cancer includes a red, swollen breast with skin edema (“peau d’orange”). The breast is generally not tender. If the inflammation persists
following a short course of antibiotics to rule out cellulitis, biopsy of the breast and skin is warranted. Inflammatory breast cancer is often a clinical diagnosis, and a benign skin biopsy should not dissuade the clinician from undertaking further evaluation and treatment. Any asymmetric skin changes or changes of the nipple–areolar complex should arouse suspicion. Paget disease of the nipple is the presence of intraductal or invasive cancer involving the nipple and should be excluded by a nipple biopsy of the abnormal area following a mammogram.
following a short course of antibiotics to rule out cellulitis, biopsy of the breast and skin is warranted. Inflammatory breast cancer is often a clinical diagnosis, and a benign skin biopsy should not dissuade the clinician from undertaking further evaluation and treatment. Any asymmetric skin changes or changes of the nipple–areolar complex should arouse suspicion. Paget disease of the nipple is the presence of intraductal or invasive cancer involving the nipple and should be excluded by a nipple biopsy of the abnormal area following a mammogram.
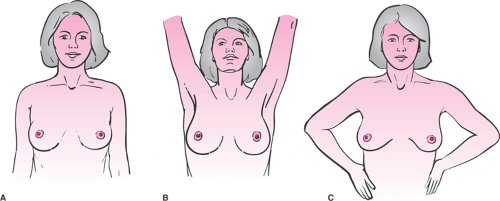 Figure 56.1 A: Inspection of patient with arms at sides. B: Inspection of patient with both arms raised. C: Inspection of patient with hands at waist, pectoral muscles contracted. |
It is important to instruct patients in the technique of breast self-examination. Physician-directed discussion on breast self-examination is the most effective approach. Physicians have the opportunity to reinforce what is normal versus abnormal to patients during the examination.
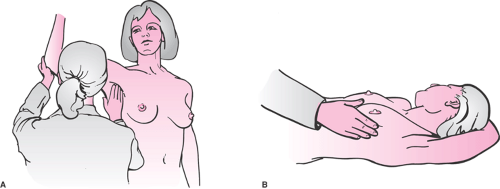 Figure 56.2 A: Palpation with patient upright, with support of ipsilateral elbow; axillary nodes and also supraclavicular nodes examined. B: Palpation of breast with patient in the supine position. |
If no abnormal findings are noted on examination, it is critical to document negative findings. The date of the last mammogram, discussion of cancer screening, and plans for follow-up should also be recorded.
Hormones (HRT or OCPs) should not be renewed without a documented annual breast examination or mammography, if indicated. A great deal of litigation results from failure to diagnose breast cancer. The Physician Insurers Association of America’s breast cancer claims study, conducted in 1988, determined that 75% of successful malpractice lawsuits involved primary care physicians with practices in family medicine, internal medicine, or obstetrics and gynecology. It is important that the medical chart includes careful documentation, since approximately one-third of the cases reported in the Physician Insurers Association of America’s study resulted from inadequate documentation.
Mammography
The primary goal of mammography is to screen asymptomatic women to help in detection of breast cancer at an early stage. In general, a routine screening mammogram consists of a mediolateral oblique (MLO) view and a craniocaudal (CC) view of each breast. With modern low-dose screening, the dose is <0.100 rad per study (for comparison, a chest x-ray delivers 0.025 rad per study). The effectiveness of screening also varies depending on the density of the breast.
Breast composition may be one of four patterns of increasing density:
almost entirely fat
scattered fibroglandular densities
heterogeneously dense
extremely dense.
The greater the breast density, the lower the sensitivity of the mammogram. Because some palpable cancers are invisible on mammography, a negative study cannot always exclude cancer. It is important to note that the false-negative rate for mammograms is 10% to 15% and that a normal mammogram does not eliminate the need for further evaluation of a dominant mass in the breast. If the clinical examination is suspicious, a negative mammogram should not delay further investigation.
Mammographic screening in women 40 years or older has reduced mortality by 20% to 30%. The efficacy of screening mammography in decreasing breast cancer mortality has been demonstrated in numerous studies. In the 1960s, the Health Insurance Plan of Greater New York performed a study of physical examination and mammography in a study group of 30,756 women and a control group of 30,239 women between the ages of 40 to 64 years. At 10-year follow-up, the study group had a 30% decrease in breast cancer mortality compared with the control group.
A total of eight large randomized trials on mammographic screening have been conducted. Six of the eight trials revealed a statistically significant reduction in mortality with mammographic screening. The reduction in mortality was not as evident among women between the ages of 40 and 49 compared with women over 50 years of age. The relative mortality reduction appears later in women between the ages of 40 and 49 at randomization compared with women 50 years of age or older. It is also likely that the small numbers of women between 40 and 49 years of age in the existing randomized trials may have contributed to this difference.
In a meta-analysis of eight randomized, controlled trials of mammographic screening, a statistically significant 18% reduction in mortality in women aged 40 to 49 was noted. Combined data from five Swedish trials yielded a statistically significant mortality decrease of 29% (Table 56.3).
TABLE 56.3 Randomized Population-based Mammography Trials | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
A published re-analysis excluded six of the eight studies because of issues related to randomization methods used and other factors in these trials. A re-analysis of the meta-analysis excluded six of the eight studies because of issues related to randomization methods used and other factors in these trials. This re-analysis questioned the risk reduction offered by mammography and resulted in much controversy.
Screening Interval
For several years, there has been a significant debate about the appropriate age at which to commence mammographic screening. In 1997, the American Cancer Society (ACS) and the NCI modified the guidelines for mammographic screening for women between the ages of 40 and 49, recommending regular mammograms for women in this age group. The recommended intervals differ: the ACS recommends a yearly mammogram starting at age 40, while the NCI recommends a mammogram every 1 or 2 years. The ACOG recommendations on mammography are similar to the NCI guidelines.
Annual screening mammography may commence earlier than age 40 in a few special circumstances (Table 56.4).
BI-RADS
In the past, a lack of uniformity in mammography terminology and reporting often led to confusion as to the malignant nature of a lesion. In 1994, the Mammography Quality Standards Act was passed by Congress and is administered by the Food and Drug Administration (FDA). It requires that mammography facilities monitor the results of their breast cancer–detection programs, including the number of recommended biopsies and the size, number, and stage of cancers detected. The American College of Radiology (ACR) Breast Imaging Reporting and Data System uses a terminology and lexicon system called BI-RADS for reporting abnormalities seen on mammography
(Table 56.5). This standardized reporting system was developed in 1995. Each category leads to a fixed assessment and specific management recommendations.
(Table 56.5). This standardized reporting system was developed in 1995. Each category leads to a fixed assessment and specific management recommendations.
TABLE 56.4 Screening Guidelines for Women Under Age 40 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
In addition, associated findings such as skin or nipple retraction, skin thickening, skin lesions, axillary adenopathy, and the presence of architectural distortion should also be reported.
TABLE 56.5 American College of Radiology BI-RADS Assessment Categories | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||
The predictors of malignancy for the BI-RADS categories are 0% to 2% for category 3 and approximately 98% or greater for category 5.
Category 4 is less predictable. Liberman and colleagues and Orel and colleagues have placed the risk of malignancy for this category around 30%.
The ACR Task Force has published a new edition of the BI-RADS classification system that will attempt to provide data on category 4 in terms of risk of malignancy. In the new edition of BI-RADS, category 4 is divided into three parts based on the prebiopsy risk for malignancy of the lesion: 4a (small); 4b (low, medium, and high); and 4c (substantial), in an effort to better guide clinicians and to collect meaningful data about this category. By subdividing the category, the ACR hopes to provide better communication to the referring physician about the prebiopsy risk of malignancy. Additionally, the fourth edition of the lexicon also addresses the assignment of categories to ultrasound and magnetic resonance imaging (MRI) findings. One recent retrospective study evaluated interobserver variability and positive predictive value of BI-RADS categories 4a, 4b, and 4c. The risk of malignancy was found to be 6%, 15%, and 53%, respectively.
Diagnostic Mammography
Abnormalities found on mammographic screening may need further evaluation with additional mammography views or other imaging modalities, such as ultrasound or MRI. In some screening programs, the mammograms are reviewed by the radiologist as they are performed, and if additional views are needed, they are performed on the same day. In other programs, if additional studies are required, the patient is called back for them at a later date. In several studies, the frequency of “call backs” has ranged from 5% to 11%.
Mammographic Lesions
A mass is defined as a space-occupying lesion seen in two different projections. If a possible mass is seen on only one view, it is called a density until its three-dimensionality is confirmed. A description of the shape and the margins of the lesion are also necessary. The highest frequency of carcinoma is noted in masses that have an irregular shape or spiculated borders. These lesions are associated with pleomorphic calcifications that appear discontinuous and linear in distribution. This discontinuous linear pattern suggests irregular filling of a duct with abnormal cells.
Microcalcifications
The BI-RADS lexicon describes calcification morphology (shape) and distribution. Calcifications may be scattered or clustered, coarse or fine, old or new. Comparison with prior mammograms is often necessary (Table 56.6).
TABLE 56.6 Morphology of Microcalcifications and Associated Lesions | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Breast Ultrasound and Magnetic Resonance Imaging
Breast ultrasonography can be used to distinguish between solid and cystic masses in the breast. It can be used to evaluate a focal mass identified on a mammogram or a palpable mass. It is also used as an adjuvant for biopsy. Because of its low specificity, it is not thought to be a good modality for screening. It cannot replace mammography, as it has no ability to detect microcalcifications. Ultrasound can complement mammography in young women with dense breasts because dense breasts limit the accuracy of the mammogram.
MRI has a high sensitivity in the diagnosis of breast cancer, ranging from 86% to 100%, but a low specificity of 37% to 97%. Because of this low specificity, it is of limited value in screening. It is an expensive test that requires intravenous contrast, and the technology for performing biopsy under MRI guidance is not widely available. Current uses include evaluation of breast implants for rupture, evaluation of pectoralis involvement with extensive breast cancer, and evaluation of postlumpectomy bed fibrosis. Other uses include evaluation of occult breast cancers and evaluation of multifocal disease in those patients who are considering breast conservation. Studies on the use of MRI for surveillance of women at high risk for hereditary breast cancer have been published recently. Warner and colleagues compared breast MRI with mammography, screening ultrasonography, and physical examination in 196 women at high risk for developing breast cancer. These women had proven mutations in the BRCA genes or strong family histories of breast and/or ovarian cancer. Six invasive cancers were found, including two cancers not identified through other modalities (i.e., mammography, ultrasound, and physical examination). A study of 236 women with BRCA mutations and MRI in conjunction with mammographic screening and clinical breast examination detected 22 cancers. Of these, 77% were detected by MRI and 32% were detected by MRI alone.
A multi-institutional Dutch national study trial for MRI screening in women with a familial or genetic predisposition, published in 2004, included 1,909 women. Of them, 358 were BRCA mutation carriers; 45 cancers were diagnosed, and 22 of these (49%) were detected by MRI alone. This demonstrates the greater sensitivity of MRI over the use of mammography alone in screening for breast cancer in these high-risk women.
Overall, MRI has proven to be an extremely valuable tool in screening women at the highest risk for developing breast cancer. Determining the optimal point in time to perform the MRI in relation to the mammogram is currently under investigation.
Digital Mammography
In 1991, the NCI convened a panel of experts on breast imaging. The panel placed high priority on the development of digital mammography. Four full-field systems were developed and underwent FDA testing. The benefits of digital mammography over traditional film mammography concern image acquisition and facilitation of storage. In addition, digital-image processing allows manipulation of image contrast and may enhance subtle contrast differences. In January 2000, the General Electric Senographe 2000D was approved by the FDA.
Pilot studies and U.S. Department of Defense full-field digital mammography screening trials of digital mammography versus conventional film mammography have found that the two modalities are similar in terms of the number of cancers diagnosed. However, the researchers noted a lower recall rate with digital mammography. Since its introduction, population-based screening trials comparing screen-film and full-field digital mammography have been conducted. In the Oslo I study conducted in Norway, full-field digital and screen-film mammography was performed in 3,683 women 50 to 69 years of age. The investigators found no statistically significant difference in cancer detection rates between the two modalities. The Oslo II study yielded similar results in cancer detection rates. Full-field digital mammography did yield higher cancer detection rates, but this difference between film and digital mammography was not statistically significant. In Canada and the United States, 49,528 women were enrolled in the Digital Mammographic Imaging Screening Trial (DMIST). All participants underwent both digital and film mammography in random order. The investigators noted that although the diagnostic accuracy of digital and film mammography was similar, the accuracy of digital mammography was better in women under age 50 years, in those with radiographically dense breasts, and in premenopausal or perimenopausal women. Thus, in women who met these
criteria, the investigators recommended digital mammography. How feasible this is remains a question, however. It is thought that fewer than 10% of facilities in the United States currently have digital mammographic systems. The cost of installing a digital mammographic system can significantly increase the cost of performing mammograms. However, when both technologies are available, the use of digital mammography can be tailored to the individual.
criteria, the investigators recommended digital mammography. How feasible this is remains a question, however. It is thought that fewer than 10% of facilities in the United States currently have digital mammographic systems. The cost of installing a digital mammographic system can significantly increase the cost of performing mammograms. However, when both technologies are available, the use of digital mammography can be tailored to the individual.
With ongoing research into this new technology, new adjunct technologies may be developed. For example, telemammography will make telemedicine consultations possible. Computer-aided diagnosis may facilitate second opinions for digital mammographic studies.
Diagnostic Evaluation
Palpable Mass
The workup of a patient with a dominant mass should include a bilateral mammogram. In addition to gaining valuable information about the characteristics of the mass, a secondary purpose in this setting is to screen the normal surrounding breast as well as the contralateral breast for nonpalpable mammographic abnormalities (densities or calcifications). Evaluation of a palpable mass is important to determine whether the mass is cancerous even if the mammogram is negative.
Fine-needle Aspiration or Biopsy
Fine-needle aspiration (FNA) can be extremely useful in providing a cytologic analysis of a palpable breast mass. Many palpable thickenings and all dominant masses should be considered for FNA, as it can differentiate between solid and cystic masses. In addition, FNA can diagnose and treat simple cysts and provide cellular material for cytologic analysis. The FNA should be performed after radiologic examination because the resultant hematoma could mask an underlying abnormality.
The breast is prepped with alcohol; with the physician facing the patient, the lesion is stabilized with the physician’s opposite hand. Usually, a 21-gauge or 25-gauge needle on a 10-cc syringe is used. Approximately 3 cc of air is aspirated into the syringe to facilitate expulsion of the contents onto the slide following the procedure. The needle is introduced into the lesion, and suction is applied on the syringe (Fig. 56.3). If the mass is cystic, the fluid is completely evacuated and the lesion should completely disappear. The syringe is withdrawn, and the fluid is discarded if it is serous and nonbloody. The patient should return in 4 to 6 weeks for reexamination.
If the lesion encountered is not cystic or suspected to be solid, an FNA biopsy can be performed in the same manner. After insertion into the lesion, multiple passes (10 to 15) through the lesion with changes in direction allow extensive sampling and create a “feel” for the mass (carcinomas are usually hard and gritty). The goal of sampling is to obtain material in the hub of the needle, not to fill the syringe. Care should be taken to release the suction before withdrawing the needle to prevent aspiration into the syringe. The sample is then ejected onto a glass slide, gently smeared with another slide, and placed in sterile jars containing 95% ethanol for transport to the cytology lab. Alternatively, it can be placed in a specimen jar containing cytofixative. The needle should be removed from the syringe, the medium aspirated into the syringe,
the needle replaced, and the medium then ejected into the jar.
the needle replaced, and the medium then ejected into the jar.
An FNA requires a cytopathologist who is experienced in breast pathology. The false-negative rate can range from 3% to 35% depending on the expertise of the aspirator and the cytopathologist, the size of the lesion, the location within the breast, and the cellular composition of the lesion. Negative findings of an FNA in the presence of a suspicious mass should not preclude further diagnostic evaluation. A diagnosis of atypical cells following an FNA warrants a surgical biopsy. Any mass remaining after aspiration of a cyst should be excised. Similarly, a cyst that recurs in the same location after one or two aspirations should be excised.
The false-positive rate of an FNA is <1%, but in the United States, most surgeons will not perform definitive surgery (i.e., a mastectomy or axillary dissection) without a prior surgical biopsy, core-needle biopsy, or frozen-section diagnosis at the time of surgery. An FNA that is positive for adenocarcinoma could, however, provide a preliminary diagnosis and guide subsequent management.
Patients with palpable solid masses can have a biopsy of the mass in the office with use of a Tru-cut 14-gauge biopsy device. The breast is prepped sterilely and a local anesthetic is used to infiltrate the skin. A small nick is made in the skin with a scalpel to accommodate the biopsy instrument. A core biopsy of the solid mass is obtained. The instrument has a “firing” range and therefore should be kept parallel to the chest wall to avoid penetrating trauma. The specimen is placed in formalin and sent to pathology. It is believed that if the specimen “floats” in the solution, it is likely nondiagnostic fat. Tumor specimens will have a grayish appearance and will typically “sink” in the solution.
Needle Localization and Excision
Needle localization is a technique that allows surgical excision of a lesion that is nonpalpable. The technique uses a hook-wire system to target the lesion, and image guidance can be provided by mammogram, ultrasound, and, in some cases, MRI. In mammography-guided needle localization, coordinates of the lesion are obtained by placing the breast in an alphanumeric grid. The needle is inserted, and when adequate placement is noted, the hook wire is deployed and the needle removed. Two mammographic views are then obtained.
The mammography films are available intraoperatively and show the relationship between the lesion and localizing hook. Excision with needle localization allows the surgeon to minimize the amount of breast tissue removed by following the needle to the targeted lesion. After removal, a specimen radiograph is obtained to ensure that successful removal of the lesion has been performed. Radiologists and surgeons who are experienced in needle localization and excisions report only 0.2% to 0.3% of lesions missed with this approach. The specimen radiograph helps to ascertain that the lesion was not missed.
Image-Guided Percutaneous Breast Biopsy
With the current advancements available in breast imaging, percutaneous image-guided breast biopsy is increasingly being used as an alternative to surgical biopsy. Percutaneous biopsy methods differ with respect to the method of imaging guidance and the tissue-acquisition device used. The use of image-guided percutaneous biopsy has advantages over surgical excision for the diagnosis of breast lesions. It is less invasive, and because less tissue is removed, it will result in less scarring on subsequent mammograms. Regardless of whether the diagnosis is benign or malignant, the patients who have percutaneous biopsies will undergo fewer operations. In addition, in cases of malignancy, the discussion and surgical treatment plan can be streamlined. The choice of which image-guided modality to use depends on the lesion. Stereotactic biopsy is best for calcifications. If a lesion is seen on ultrasound, it is best to use that modality, as it is easier to use and has been reported to be less costly.
Stereotactic Biopsy
Stereotactic biopsy uses specialized mammography equipment to calculate the location of a lesion in three dimensions. Stereotactic biopsy can be performed with the patient prone on a dedicated table or with the patient sitting in an upright unit. An automated core needle or directional vacuum-assisted biopsy probe is used to obtain the tissue specimens. Multiple tissue specimens are obtained for pathologic analysis. Many reports in the medical literature state that the procedure has a sensitivity of 70% to 100% and a specificity of 85% to 100%. The greatest success is noted in reports using 14-gauge core needles, as well as in those with increased numbers of specimens obtained. In mass lesions, it is likely that five core samples may be adequate for accurate diagnosis; however, ten or more core specimens may be required in cases of calcifications.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



