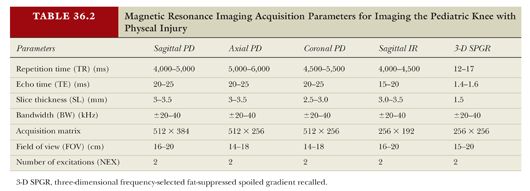
In 1963, Salter and Harris15 initially categorized fractures involving the physis (Fig. 36.2). This remains the most commonly used classification system guiding treatment of physeal injuries.15 Types I and II fractures are extra-articular, whereas types III to V fractures are intra-articular. Types III to V fractures may result in both joint incongruity and physeal damage.
Type I fractures are confined to the physis without extension into either the epiphysis or the metaphysis.
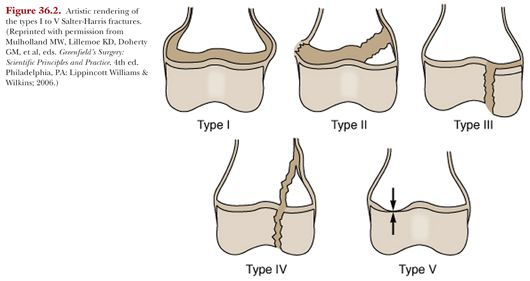
Type II fractures (Fig. 36.3) extend along the physis and exit through a portion of the metaphysis, often yielding a triangular-shaped metaphyseal fragment, sometimes referred to as a Thurston Holland fragment.
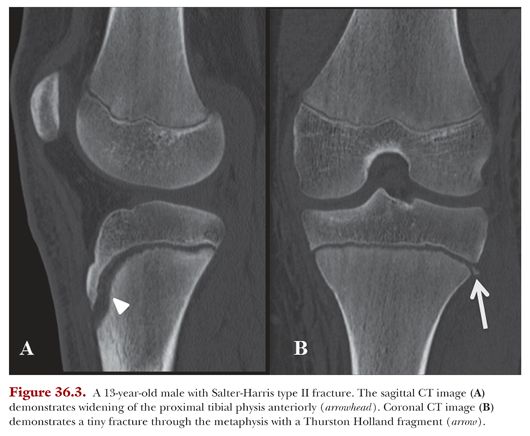
Type III fractures (Fig. 36.4) extend from the articular surface, through the epiphysis to the physis, through which the fracture exits.
Type IV fractures arise from the articular surface, extend through the epiphysis and physis, and exit through the metaphysis. Anatomic reduction of the physis is necessary to reduce the risk of bony bar formation.
Type V fractures are compression or crush injuries to the physis.
The Salter-Harris types III to V fractures are associated with the greatest risk of future growth disturbances.16
Of traumatic fractures involving the physis, the Salter-Harris type II fractures are the most common (60.9%) followed by type I (28.6%), type III (6.7%), and type IV (3.7%) fractures. No type V injuries were identified in the cohort studied by Kawamoto et al.2
Harris growth arrest lines, related to variations in the rate of bone growth, typically parallel the physis and can indicate physeal damage. These growth arrest lines may be seen on radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) examinations. A decreased distance between the growth arrest line and the physis on the side of injury indicates a deceleration of growth of the injured extremity. In contrast, complete absence of a growth arrest line in an injured extremity indicates complete cessation of growth. Growth arrest lines that are oblique rather than parallel to the physis suggest a tethering effect secondary to partial growth arrest. Other secondary signs of a partial growth arrest include progressive malalignment.5
Radiographs are the first-line imaging approach,7 particularly in the setting of trauma, due to their cost-effectiveness and ease of accessibility.17 However, radiographs do not allow for direct evaluation of the cartilage, as noncalcified cartilage is lucent on radiographs and thus secondary signs of physeal injury must be relied upon to make a diagnosis.18 Secondary findings of physeal injury on radiographs include epiphyseal displacement; physeal widening; and indistinctness of the normal, sharply defined sclerotic margins on the opposing sides of the epiphysis and metaphysis.12
On radiographs, signs of a type I fracture include widening, haziness, sclerosis, or irregularity of the physis. These findings can be subtle, and radiographs of the contralateral, symptom-free side may be helpful for comparison. For the types II through IV fractures, the fracture lucency may be seen in the metaphysis and/or epiphysis, but the precise degree of involvement of the physis can often not be determined. Of note, the type V injuries are often radiographically occult at initial assessment, leading to a delay in diagnosis if radiographs are the only means of imaging used to evaluate the injured patient.
Stress radiographs may be useful in evaluating posttraumatic joint stability, but they are often not possible in the acute trauma setting because of pain inhibition. In addition, there is a risk that the applied stress could cause inadvertent injury to the physis, such that a subtle Salter-Harris type I fracture might be converted into a displaced Salter-Harris type III fracture.19
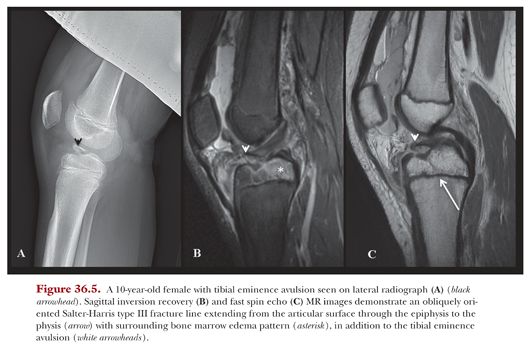
Radiographs are indicated for evaluation of fractures, but the use of radiography in isolation has significant limitations. Evaluation of the physis can be difficult when the x-ray beam is not parallel to the physis.20,21 The irregular three-dimensional (3-D) nature of the physis, which includes anatomic undulations and ridges, limits the use of the two-dimensional imaging used in radiographs. Subtle nondisplaced fractures may be occult on radiographs (Fig. 36.5).12
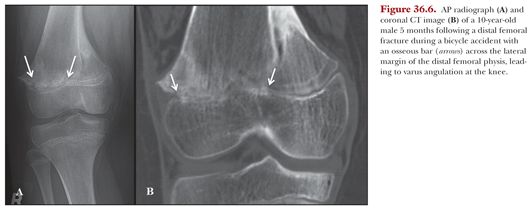
Only osseous bars are potentially visible on radiographs; fibrous tissue is radiolucent and a fibrous physeal bridge could not be appreciated. Even in the setting of an osseous bridge across the physis, radiographs cannot provide 3-D information regarding the size and location of the bridge (Fig. 36.6).
The widespread availability of radiography is useful in the regular follow-up of fractures to assess for fracture healing and to evaluate for potential growth disturbances and development of malalignment. Following physeal injury, the frequency at which follow-up radiographs should be obtained will vary based on the assessment of risk for subsequent growth disturbance. For example, with higher risk physeal injuries, it is reasonable to obtain radiographs every 3 months until normal growth rate can be documented, which may take up to 2 years5 or even until skeletal maturity.6 Without close radiologic follow-up, an angular deformity might not be identified until it is already apparent clinically6 at which time it may be more difficult to surgically correct.
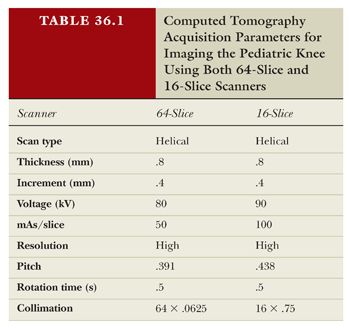
Cross-sectional imaging modalities such as CT can demonstrate the extent of physeal involvement in more detail than radiographs. CT can demonstrate subtle alterations in fracture alignment, which is particularly useful in Salter-Harris types III and IV fractures, which involve the epiphysis.12 Additionally, CT can provide further detail about a bony physeal bar. However, as with radiographs, cartilage remains radiolucent on CT, and direct visualization of a physeal injury remains limited. CT is more expensive than radiography22 and also employs ionizing radiation for image acquisition, but CT imparts higher doses of radiation to patients than radiographs do.23 Radiation dose is of vital importance, particularly in pediatric patients whose organs are more radiosensitive and whose longer life expectancy affords a lengthier period of time during which they can potentially develop a radiation-induced cancer.24 Radiation shielding should be always used, especially when imaging pediatric patients, with shields placed above and below the patient. Newer dual-energy CT scanners offer superior bone detail with marked reduction in dose. Table 36.1 shows suggested parameters used for scanning the knee with physeal injury on both 16- and 64-slice CT scanners.
With acquisition of thin slices yielding isotropic data sets, the CT data can be post-processed to generate both multiplanar reconstructed images and 3-D reformations (see Fig. 36.6).25 Thus, unlike radiography, CT can provide complex anatomic information about an osseous physeal bar.
CT is unable to provide as much direct information about physeal anatomy and pathology compared with MRI, but it remains an important imaging modality in the settings of Salter-Harris types III and IV fractures where detection and treatment of subtle joint incongruities is vital (see Figs. 36.4 and 36.5). CT is also indicated in the relatively small subset of patients in whom MRI is contraindicated.
In 1990, Jaramillo et al.18 first used MRI to evaluate physeal injuries in an animal model. Since then, MRI has proven to be clinically useful in demonstrating osseous and fibrous physeal bridges, epiphyseal and metaphyseal avascular necrosis, and growth arrest.12 An MRI of the knee obtained soon after injury can provide meaningful information about the relative location, morphology, and type of fracture26 or physeal injury as well as the precise size of the physeal damage.27
MRI is of particular value, as it offers high spatial resolution, superior soft tissue contrast, and multiplanar imaging capabilities without using ionizing radiation.19 Although MRI is more expensive and the acquisition and postprocessing is more time-intensive than that for radiography and CT, MRI can provide direct visualization of the physeal cartilage.20
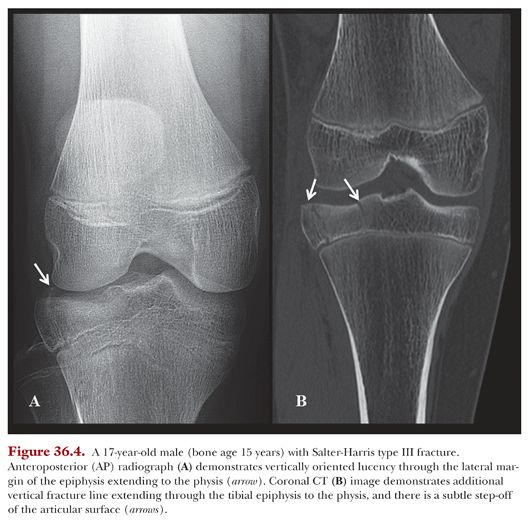
MRI of pediatric patients should be performed on a clinical 1.5 or 3.0 T magnet using a surface coil. Table 36.2 shows a suggested protocol for obtaining a knee MRI in pediatric patients.