Introduction
The pregnant woman is susceptible to the specific consequences and complications of pregnancy as well as the full array of medical events that may occur unrelated to the pregnancy. In many cases, some form of diagnostic imaging will be required to assess or manage these conditions. The selection and application of the most appropriate imaging modalities will often require a multidisciplinary approach involving obstetricans, maternal-fetal medicine specialists, internists, surgeons and radiologists. This must take into account the clinical situation as well as the risks and benefits of the various forms of diagnostic imaging: ultrasound, X-ray, computed tomography (CT), radionucleotide scanning or magnetic resonance imaging (MRI). Although this chapter focuses on what is known about the safety of various modalities of diagnostic imaging in pregnancy, it is worth emphasizing that both the available data and broad clinical experience suggest that more harm is likely to be caused to pregnant women and their fetuses by withholding diagnostic imaging than by its judicious application.
X-rays and gamma rays ionize tissue through the deposition of energy. This is the first step in a series of events that may subsequently lead to genetic and/or biologic effects Environmental exposures [1] (Table 32.1), diagnostic [2] imaging techniques including X-ray, fluoroscopy, angiography, mammography, positron emission tomography (PET), single photon emission computed tomography (SPECT), computed tomography (CT) and most nuclear medicine procedures involve exposure to ionizing radiation. Any adverse effects of ionizing radiation on the outcome of pregnancy are dependent on the fetal radiation dose, the timing of exposure and the form of administration.
Table 32.1 Background/environmental radiation exposure
| Environmental source | Exposure |
| Cosmic, gamma and radon | Varies from 1.8 mSv/yr in the UK and Australia to 7.8 mSv/yr in Finland |
| Occupational exposures in workplaces that involve radiation | Most safety laws limit radiation exposure during gestation to <20 mSv and <100 mSv/5years |
| Cosmic radiation with air travel | 0.001–0.003 mSv/h on short-haul routes and up to 0.005 mSv/h on long haul |
| Nuclear accidents such as Chernobyl 1986 | 10–50 mSv over the subsequent 20 years (thyroid doses much higher) [3] |
Radiation is measured in three distinct ways:
- the amount being given off or emitted by a radioactive material (measured in curie or becquerel)
- the amount deposited per unit of weight of human tissue (the “absorbed dose” measured in rad, milligray or gray)
- the biologic risk of the exposure (measured in rem or sievert).
Absorbed dose and biologic risk are different depending on the type of radiation (alpha and beta particles, gamma rays and X-rays), and the particular tissue receiving the dose. This is because the different types of radiation have variable ability to transfer energy into the cells of the body.
Biologic risk of exposure, expressed as sieverts, is most often used when discussing radiation protection, particularly in environmental or occupational contexts. The radiation dose of interest in discussions about diagnostic imaging in pregnancy is the absorbed dose in grays or rads. (One Gy is equal to 1000 mGy is equal to 100 rad.) In assessing the potential effects of radiation in pregnancy, it is necessary to calculate both the maternal dose to a particular site as well as the estimated fetal absorbed dose. The remainder of this chapter will review what is known about the exposure risks to various common diagnostic imaging modalities.
Ultrasound and magnetic resonance imaging
Imaging techniques that do not involve electromagnetic radiation, i.e. ultrasound and MRI, are considered safe in pregnancy. The UK National Radiological Protection Board has recommended that “until further information becomes available, it is considered prudent to exclude pregnant women from NMR studies during the first 3 months of pregnancy. However, MR diagnostic procedures should be considered where the only reasonable alternative is an X-ray procedure” [4]. For MRI, gadolinium is used as a tracer to enhance imaging of vascular tissue or abnormal tissue. Gadolinium is teratogenic in high doses in animal studies, but a number of studies have evaluated the administration of gadolinium contrast material during human pregnancy and reported no obvious harmful effects. Administration of gadolinium contrast material in the first trimester should therefore be avoided where possible. In practice, contrast material is of limited usefulness in most obstetric applications (with the exception of assessing placenta accreta) and would more likely be required for an extra-abdominal indication such as a suspected maternal brain tumor. In such a situation, the maternal benefits would probably outweigh the potential fetal risks. Both the American College of Radiology and the European Society of Urogenital Radiology have stated there is no requirement to cease breastfeeding following the administration of gadolinium to a lactating woman as excretion of gadolinium into breast milk is extremely limited.
Fetal absorbed radiation with x-rays and computed tomography
In estimating the absorbed dose to the fetus, a number of techniques have been used. Dosimetry surveys even within a particular country have been found to vary by a factor of up to 30 or more for the same examination. With fluoroscopy, e.g. for uterine artery embolization, endoscopic retrograde cholangiopancreatography (ERCP) or other procedures, additional factors such as location of the beam, duration of screening, magnification and conventional versus pulsed fluoroscopy will influence dose. Digital radiography techniques may reduce fetal absorbed dose considerably. In a study of X-ray pelvimetry, the use of digital radiography reduced fetal absorbed dose by 85% [5]. Estimations of fetal absorbed dose from CT examinations vary considerably, depending on the method used [6]. In addition to the radiation technique, site and dose administered, factors such as maternal thickness will influence the fetal absorbed dose following X-rays and CT scanning. Table 32.2 presents approximate fetal absorbed doses for a number of common radiologic procedures. Conventional X-ray examinations beyond the abdomen/pelvis are associated with a negligible fetal absorbed dose, related to scatter or leakage radiation. More direct examinations, particularly those with fluoroscopy such as barium enemas, are associated with a more significant fetal absorbed dose.
Table 32.2 Approximate fetal doses from common diagnostic procedures [7–10]
| Mean in mGy | Maximum in mGy | |
| Conventional X-rays | ||
| Abdomen | 1.4 mGy (0.014 rad) | 4.2 mGy (0.042 rad) |
| Chest | <0.01 (<0.0001 rad) | <0.01 (0.0001 rad) |
| Intravenous pyelogram | 1.7 (0.017 rad) | 10 (0.1 rad) |
| Lumbar spine | 1.7 (0.17 rad) | 10 (1 rad) |
| Pelvis | 1.1 (0.11 rad) | 4 (0.4 rad) |
| Skull | <0.01 (0.001 rad) | <0.01(0.01 rad) |
| Thoracic spine | <0.01 (0.001 rad) | <0.01 (0.001 rad) |
| DEXA posterior anterior spine | 1.7 (0.17 rad) | 4.9 (0.49 rad) |
| DEXA proximal femur | 1.0 (0.1 rad) | 2.7 (0.27 rad) |
| Fluoroscopic examinations | ||
| Barium meal | 1.1 (0.11 rad) | 5.8 (0.58 rad) |
| Barium enema | 6.8 (0.68 rad) | 24 (2.4 rad) |
| ERCP | 400 (40 rad) | 1800 (180 rad) |
| Computed tomography | ||
| Abdomen | 8.0 (0.8 rad) | 49 (4.9 rad) |
| Chest | 0.06 (0.006 rad) | 0.5 (0.05 rad) |
| Helical chest | <0.01 (0.001 rad) | 0.13 (0.013 rad) |
| Head | <0.005 (0.0005 rad) | <0.005 (0.0005 rad) |
| Lumbar spine | 2.4 (0.24 rad) | 8.6 (0.86 rad) |
| Pelvis | 25 (2.5 rad) | 79 (7.9 rad) |
| Pelvimetry | 0.2 (0.02 rad) | 0.4 (0.04 rad) |
DEXA, dual energy X-ray absorptiometry.
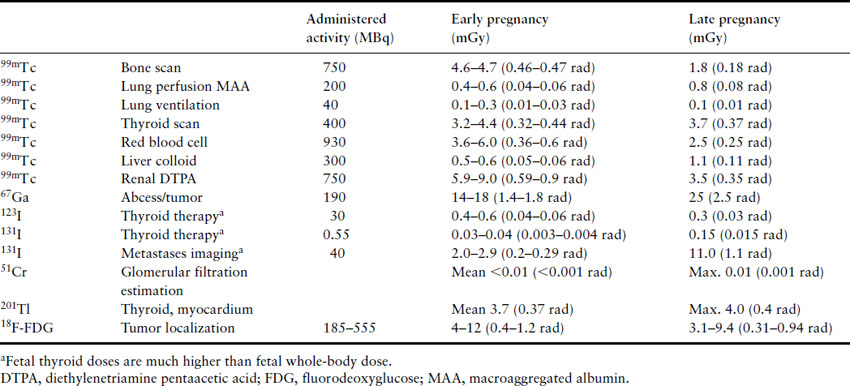
Fetal absorbed radiation with nuclear medicine imaging
In the case of nuclear medicine and PET studies, fetal absorbed dose will represent the cumulative effect of external irradiation from the maternal tissues as well as placental transfer and fetal uptake of radiopharmaceuticals (Table 32.3). The majority of radiopharmaceuticals are excreted in urine and irradiation from maternal bladder contents may be a more important source of fetal radiation. Hence, measures aimed at increasing the rate of urinary excretion may reduce the fetal absorbed dose significantly. Using smaller administered doses and longer imaging times can significantly reduce the fetal absorbed dose.
Table 32.3 Fetal whole-body dose from common radiopharmaceuticals in early pregnancy and at term. Dose includes maternal and fetal self-dose contributions [8,9,11,13]
Risks of radiation in pregnancy
Experimental assessments of radiation effects have identified a number of specific areas of potential concern:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


