In a follow-up study of 314 athletes (mean age 32.7 years), less than half (45%) of these athletes had returned to sport at greater than 3 years after ACLR. However, younger athletes were found to return to preinjury levels of play at a greater rate. Of the 43 athletes younger than 18 years of age, 72% had attempted playing their preinjury sport which was the highest percentage of any of the groups (18 to 25 years, 26 to 32 years, .32 years) but only 49% reported playing at their preinjury level at follow-up.21
The Multicenter Orthopaedic Outcomes Network (MOON) group reported 85% of 100 soccer athletes (mean age ♂ 27.7 ♀19.8 years) returned to preinjury level of play.22 Shelbourne et al.23 provided further evidence that age is inversely related to the likelihood of return to competition. In a study of 413 high school basketball and soccer athletes with mean age of 15.5 years, Shelbourne et al.23 reported that 87% of the basketball athletes (both boys and girls) returned to high school competition and 93% of the females and 80% of the male soccer athletes returned to competition.
“Other interests” and fear were cited as the primary reasons for failure to return to play rather than physical symptoms in high school and college football players following ACLR.24
Psychological factors may play a significant role in a greater likelihood of return to preinjury level of activity in adolescent athletes following ACLR. In a study comparing adolescent and adult psychological readiness for ACL surgery, Udry et al.25 found that adolescents reported not only higher preoperative mood disturbance levels than adults but also higher levels of “psychological readiness” for surgery. Adolescents reported more pros associated with surgery and used a greater number of cognitive and behavioral processes of change than adults. The greater mood disturbances prior to surgery and the greater “readiness” for surgery may be the result of the central role that physical activity may play in their life at this stage. Adolescents may be more disturbed by the disruption in their usual activities and separation from their peers and more invested in returning to their previous level of activity.
Both organized sports and social play and games play an important developmental role in the child and adolescent athlete. Acceptance by peer groups takes on critical importance at this stage as the child develops his or her sense of identity independent of his or her family. Sports provide a way to learn to interact socially, work toward a collective goal, follow rules, and understand the concept of fair play.26 When children and adolescents are sidelined by injury, they are not only deprived of the pleasure of playing a sport they enjoy but also deprived of the opportunities for personal growth and development that is provided by the social aspect of organized sports and free play.
In a study of the influence of patient outcomes following ACLR, younger patients had significantly higher self-efficacy scores which are related to greater perceived knee function, postoperative sports activity levels, and knee-related quality of life.27 The patient’s preinjury level of activity was also found to be predictive of the probability of returning to preinjury levels of activity.
The greater availability of sports for middle and high school athletes, the social role that sports may play in this age group in which teammates form a key social support system, and psychological factors may all play a role in the greater return to play rates in pediatric and adolescent athletes following ACLR.
An ACL injury at a young age is a life-changing event. In addition to surgery and many months of rehabilitation, the time lost from school and play can have significant effects on the athlete’s mental health and academic performance.28 Elective knee ligament reconstruction performed on a school day results in more difficulties than surgery performed during a school holiday or summer break; therefore, a child’s daily school life should be accounted for in the surgical decision-making process.29 The consequences are far more reaching than being sidelined from their sport; they are often sidelined from their life, or perceive it that way.
FACTORS ASSOCIATED WITH RISK OF SECOND INJURY
The psychological makeup of a pediatric patient combined with the physical challenges they must overcome following ACLR is a recipe for increased risk of a second injury.
Given that pediatric and adolescent ACL patients are more likely to return to sport and face a high risk of a second injury, what specific factors have been identified as risk factors?
Not surprisingly, risk is related to activity levels. For each increase of 4 points on the Marx Activity Scale, the risk of retear increases threefold.30 Age is also a key factor; risk of reinjury is estimated to drop by 50% for each decade of life, placing the pediatric and adolescent athlete squarely in the highest risk group.31 In discussing RTP, it must be remembered that top-level athletes may well have exceptional neuromuscular skills and therefore be reasonably well prepared to meet the demands of safe return to sport. It is, however, the clumsy or unskilled player who returns to a low level of sport who may be at greater risk of reinjury.32
Biomechanical factors that have been identified as risk factors for primary ACL tear are, not surprisingly, found to be associated with risk of secondary ACL tear.11,13,33–37 Paterno et al.11 performed 3-day analysis of drop vertical jump (DVJ), postural stability analysis by Biodex, and a KT-1000 on 56 athletes aged 13 to 20 years returning to level 1 sports; 13 athletes went on to suffer a second ACL tear in the first year following return to play. Athletes who demonstrated deficits in postural stability on the involved limb were two times more likely to retear. Findings from the 3-day analysis of DVJ were even more predictive of second injury. Side-to-side differences in sagittal knee moment at initial contact and greater frontal plane knee motion during landing were correlated with a three-fold or greater increase in likelihood to tear, whereas those demonstrating hip rotation at the initial 10% of landing were more than eight times more likely to suffer a second ACL injury.
In a follow-up study of the incidence of second ACL injury 2 years after primary ACL injury and return to sport, Paterno et al.38 reported 15 times greater risk of ACL tear during the first year compared to a 6 times greater risk than controls in the second year following return to sport.
The influence of biomechanical factors and neuromuscular control on risk of sustaining a second ACL injury, either ipsilateral or contralateral, indicates the need for evaluation of these factors in the return to play decision-making process in this high-risk population.
CURRENT MODELS OF RETURN TO PLAY DECISION MAKING
Quantitative measures have historically played the principal role in determining when an athlete is cleared for play following ACLR. A systematic review from 2001 to 2011 was conducted to identify factors used to determine unrestricted return to play after ACLR.39 Of 264 articles, 40% failed to provide any criteria, 32% used amount of time postoperatively as the only criterion, and only 13% noted objective criteria required for return to athletics. These included muscle strength (9%), single-leg hop test (4%), general knee examination (6%), knee stability (1%), and validated questionnaire (1%). Only 2 studies out of 264 surveyed reported using three to four criteria to determine readiness to return to unrestricted activity. The criteria included strength, single-leg hop tests, absence of effusion, full range of motion (ROM), and 90% limb symmetry index (LSI). There is a discrepancy between functional and physical measures and the rate of return. Ardern et al.15 reported that despite 90% of patients achieving normal or near-normal outcomes on impairment-based measures of knee function, only 44% returned to competitive sports. This suggests that factors other than knee function could be contributing to return to sport. It also may suggest that LSI, in this population, may not be a good indicator of readiness. The contralateral limb is not the standard to which the index limb should be held. The commonly used functional tests may not be sensitive enough or demanding enough to identify deficits. Perhaps, the element of fatigue is not addressed sufficiently. Again, the role of psychological readiness cannot be overstated.
In a 2013 survey of 274 experienced arthroscopic surgeons, the most common measures used to determine clearance for play included Lachman test, pivot shift, anterior drawer, and ROM.40 Over 85% reported using no clinical measures whatsoever.
Barber-Westin and Noyes39 recommended a multifaceted approach to determining readiness to return to play: less than 10% LSI with isokinetic testing, less than 15% LSI with single-leg hop testing, less than 3 mm increased anteroposterior tibial displacement on Lachman or arthrometer testing, greater than 60% knee separation distance with DVJ, no effusion, full knee ROM, normal patellar mobility, no or minimal patellar crepitus, and no pain or swelling with all activities. In addition, single-leg squat, multistage fitness test, and 60-second sit-up test are considered.
A multifaceted approach has been proposed by several clinicians; however, it seems their criteria are still heavily weighted toward quantitative data. Myer et al.41 at the Cincinnati Children’s Hospital propose an algorithm for a safe return to sport. In order to enter the return to sport phase, the athlete must have no postsurgical history of giving-way, an International Knee Documentation Committee score of 70, and minimum baseline strength of knee extension peak torque to body mass: 30% females, 40% males at 300 degrees per second; 50% females, 60% males at 180 degrees per second. They propose a four-stage criteria-based return to sport progression, which incorporates measures of side-to-side symmetry in strength and landing force as well as measures of dynamic stability and mechanics of jumping and landing.
Wilk et al.42 proposed a return to sport progression over 20 to 30 weeks of rehabilitation based on fulfillment of specific criteria including results of KT-1000, isokinetic testing, proprioception, hop test, and practical specific tests.
Criteria used at the University of Delaware include quadriceps strength index (QSI), LSI on four hop tests, Knee Injury and Osteoarthritis Outcome Score (KOOS), and Global Rating Scale before entering the return to sport phase.43
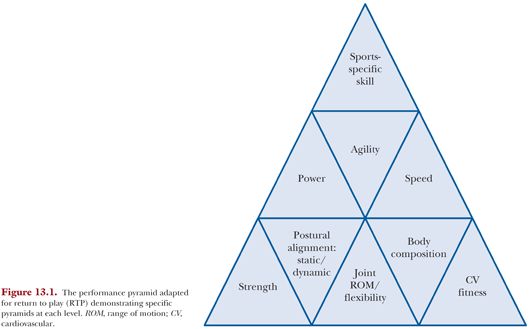
Given the high rate of reinjury, the ideal criteria to determine readiness to return to play has yet to be identified. Quantitative measures combined with the eagerness of the child and family to return to activity may result in clearing an athlete who demonstrates all of the qualitative risk factors for retear (postural instability, hip internal rotation, etc.) despite “passing” the quantitative thresholds. Often, these young individuals have not trained formally prior to their injury. The adolescent has only focused on skill development—playing soccer, etc. The optimum performance pyramid as described by Cook44 has a broad base of functional movement, with a slightly smaller level in the middle of functional performance and an even smaller level on top of sport-specific skill. Movement patterns, movement efficiency, and sport skill are balanced and adequate in the optimum performance pyramid (Fig. 13.1). In our experience, the adolescent and the injured athlete’s pyramids are often out of balance. As mentioned, the adolescent athlete focuses on the very top of the pyramid, where the focus for the rehabilitating athlete is too often the middle part of the pyramid. There may also be instances when the athlete does not feel ready to return to play despite meeting all clinical criteria. Patient reported outcome measures (PROM) specific to this population should be administered.