Complications of Labor
Donald J. Dudley
From 1970 to 2005, the cesarean delivery rate in the United States increased from 5% to 30%. The four primary indications for cesarean delivery include dystocia, elective repeat cesarean delivery, fetal distress, and abnormal fetal presentation. Dystocia, translated, means “difficult birth” and includes all abnormalities that may occur in women during labor. An expanded definition advanced by Bowes is that dystocia is “any complication or circumstance that interferes with the progress of labor and vaginal delivery that endangers mother or fetus.” Most authorities agree that the number of cesarean deliveries remains excessively high. One reason for the continued high rate of cesarean delivery is a poor understanding of the labor process and the lack of an organized approach to the management of labor. This fundamental lack of understanding often leads to unnecessary induction of labor, which has an a priori risk of cesarean delivery of at least 25%, or to inadequate augmentation of abnormal labor. With fewer inductions of labor and improved management of labor, a decline in the cesarean delivery rate can be expected.
Efforts at reducing the cesarean delivery rate have more recently focused on the categories of dystocia and repeat cesarean section. Obviously, the best method to decrease the incidence of repeat cesarean deliveries is to decrease the incidence of cesarean delivery initially. Hence, new efforts are being directed at the diagnosis and management of labor abnormalities in term pregnancies. The purpose of this chapter is to review these labor abnormalities and management options.
Keys to the Management of Normal Labor
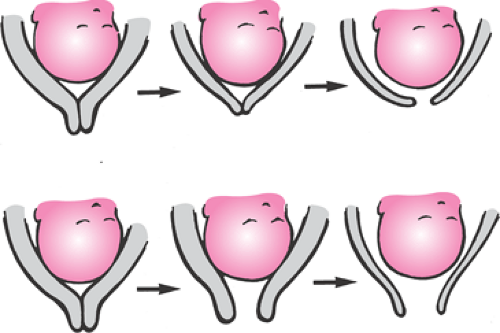
The normal labor process is reviewed in Chapter 2. The key points in the management of labor emphasized in this chapter are summarized in Table 24.1. Normal labor progresses in a predictable fashion after the diagnosis of labor is made. However, diagnosing labor is more difficult than might be expected. If the diagnosis of labor is made in error, all subsequent actions are not appropriate, as an induction of labor is being performed and different management is required. Labor in its simplest terms is defined as cervical change effected by regular, painful uterine contractions. In the nulliparous woman in her first labor, cervical change usually is manifest by cervical effacement, or thinning, followed by cervical dilation (Fig. 24.1). Conversely, in the multiparous woman, the initial stage of labor often is characterized by cervical dilation followed by effacement.
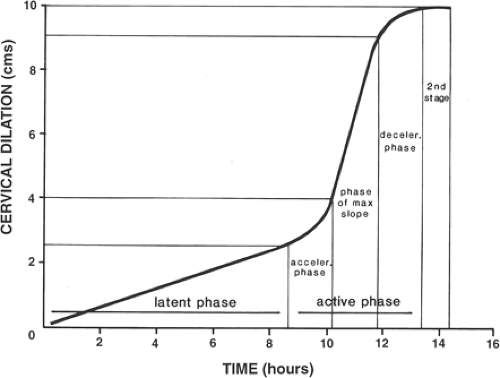
The normal labor curve is shown in Figure 24.2. This curve was developed by Emanuel Friedman based on the observation of several thousand laboring women. The first stage of labor is divided into the acceleration phase, active phase, and deceleration phase. The acceleration phase occurs when the active phase of labor starts. The cervix usually is effaced and <4 cm dilated. In the active phase, a minimum of 1 cm of dilation per hour can be anticipated (Table 24.2). The deceleration phase likely is an aberration of the mathematic analysis of Friedman’s original data and as such is likely not a physiologic event. In the second stage of labor, from complete dilation until delivery, again one can anticipate the laboring woman gaining a minimum of 1 cm of station of the fetal head in relation to the maternal pelvis per hour. Cervical examinations should be performed periodically to confirm that progress is being made. Early in their training, residents should be encouraged and allowed to perform examinations hourly so that full educational opportunities are gained. More experienced obstetricians often will perform examinations every 2 to 3 hours, depending on the presentation of the patient. After each examination, the progress in labor should be documented graphically on some form of a labor curve and a plan formulated with regard to future examinations and potential interventions. Other terms for a labor curve include partogram, labor graph, and parturograph.
TABLE 24.1 Keys to the Management of Labor | |
|---|---|
|
Nulliparous women and multiparous women behave fundamentally differently in labor. Figure 24.3 is an example of a labor curve showing the difference in labor patterns expected between nulliparas and multiparas. In the simplest terms, labor is the force of uterine contractions overcoming the resistance of the female reproductive tract, including the lower uterine segment, cervix, vagina, and perineum. In nulliparous women, more uterine force is required to overcome resistance in the reproductive tract, and the uterus tends to be less effective in maintaining effective uterine contractions. In multiparous women, less uterine force is required, and the tissues of the reproductive outlet, having been stretched by the previous delivery, have less resistance. As a result, the myometrium of the multipara usually maintains effective contractile activity. Thus, nulliparous women are more likely to develop labor abnormalities that require intervention. Multiparous women usually labor quickly and meet all expected milestones without the need for significant intervention.
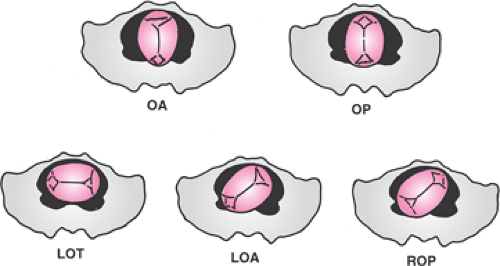
In addition to graphically depicting labor progress, the practitioner should pay close attention to the cardinal movements of labor (Table 24.3). This term refers to the changes that occur in the flexion and position of the fetal head throughout labor. The cardinal movements of labor usually occur in the following sequence: engagement of the fetal head, descent of the fetal head, flexion of the fetal head, internal rotation (assumption of an occiput anterior [OA] position), extension (as the fetal head progresses through the birth canal and crowns at the perineum), external rotation (or restitution to the transverse position), and then shoulder rotation after the head has delivered. Abnormalities in the cardinal movements of labor may be reflected by abnormal fetal head position and other specific abnormalities discussed below.
If labor is progressing appropriately, then a noninterventional approach is indicated, providing for maternal comfort and encouragement. However, if these landmarks are
not achieved by the patient, then timely intervention is recommended. Thus, the next important key in the management of labor is prompt intervention when labor progress is inadequate. The longer labor continues in a dysfunctional pattern, the less likely the underlying problem can be corrected with medical therapy. Prompt medical therapy for desultory labor is another important key to success in the management of labor.
not achieved by the patient, then timely intervention is recommended. Thus, the next important key in the management of labor is prompt intervention when labor progress is inadequate. The longer labor continues in a dysfunctional pattern, the less likely the underlying problem can be corrected with medical therapy. Prompt medical therapy for desultory labor is another important key to success in the management of labor.
TABLE 24.2 Expected Length of Different Phases of Labor | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Ineffective uterine contractions lead to increased tissue acid content in the myometrium, which further contributes to poor contractility. In one study, the pH of myometrial capillary blood obtained at the time of cesarean delivery from women with dysfunctional labor was lower than in women having cesarean for other indications. This also was associated with higher capillary lactate and lower oxygen saturation.
Normal labor is characterized by coordinated uterine contractions, cervical dilation, gain in station of the fetal head, and normal progress in the cardinal movements of labor. With careful attention to achieving these milestones of normal labor, a successful vaginal delivery is likely. However, if the parturient does not achieve these milestones, prompt intervention is more likely to increase the chances for vaginal delivery. Although an aggressive approach with regard to diagnosing labor abnormalities may enhance maternal and fetal outcome, the last important key to the successful management of labor is to use clinical judgment on when to abandon medical therapy in favor of surgical intervention. If the judgment is made that continuing medical therapy may dangerously compromise either mother or fetus, then prompt surgical delivery (cesarean or operative vaginal delivery) should be considered.
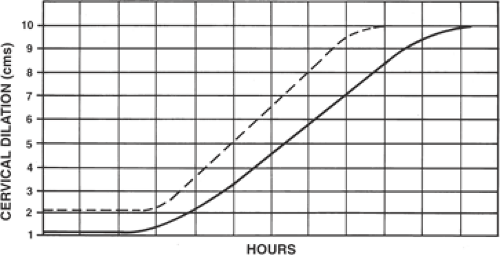 Figure 24.3 Labor curve of nulliparas versus multiparas. Note that different labor slopes are expected between nulliparous (solid line) and multiparous women (dotted line). |
TABLE 24.3 The Cardinal Movements of Labor | |
|---|---|
|
Epidemiology of Dystocia
The precise incidence of dystocia is difficult to determine and varies with different populations and different labor and delivery units based on local practice patterns. According to the National Center for Health Statistics, 28% of women who delivered in the United States in the year 2000 were diagnosed with labor abnormalities, with a primary cesarean delivery rate of 16.1%. The rate of primary cesarean delivery in 2004 increased to 20.6% of all deliveries in the United States. Dystocia is more common in nulliparous women than in multiparous women and is more common in the first stage of labor than in the second stage of labor. Labor abnormalities occur in approximately 25% to 30% of nulliparous women and in 10% to 15% of multiparous women. Dystocia occurs in the second stage of labor in about 5% to 10% of nulliparous women and is relatively rare in multiparas (<2%).
Abnormal labor is a common indication for cesarean delivery. According to the National Center of Health Statistics, in the United States in 2005, 30.2% of pregnancies were delivered by cesarean. In 1990, the overall rate was 23.6%, with 7.1% for the indication of “failure to progress” or dystocia and 8.5% for a repeat procedure. Other indications included abnormal presentation (2.6%), fetal distress (2.3%), and other problems (3.2%). Improved management of labor with a decrease in the number of cesarean deliveries for dystocia (and then having less need for repeat procedures) should be the goal of every labor and delivery unit in the United States. One contributing
factor to the cesarean delivery rate is the number of inductions. In 2004, the rate of inductions was 21.4% compared with a rate of 9.5% in 1990. Clearly, the induction rate has increased dramatically, with no proven benefit to perinatal outcome. While there have been many proposed targets for the overall rate of cesarean delivery and inductions, none of these figures is based on scientific evidence.
factor to the cesarean delivery rate is the number of inductions. In 2004, the rate of inductions was 21.4% compared with a rate of 9.5% in 1990. Clearly, the induction rate has increased dramatically, with no proven benefit to perinatal outcome. While there have been many proposed targets for the overall rate of cesarean delivery and inductions, none of these figures is based on scientific evidence.
In 2000, the American College of Obstetricians and Gynecologists (ACOG) published a monograph reporting on the efforts of a special task force charged with focusing on cesarean delivery in the United States. The primary conclusion of this task force was that efforts to reduce the cesarean delivery rate in the United States should focus on two benchmarks. First, there should be a focus on nulliparous women at term (37 weeks gestation or greater) with singleton fetuses in cephalic presentation. In 1996, the cesarean delivery rate for this group was 17.9%, and the Task Force concluded that efforts to achieve a reduction to the 25th percentile, or 15.5%, in this group of women were reasonable and could be accomplished. Second, the Task Force recommended that efforts be made to increase the percentage of women who are attempting vaginal birth after cesarean (VBAC). Of multiparas at 37 weeks gestation or greater with singleton fetuses and vertex presentations with prior low transverse cesarean incisions, 30.3% attempted VBAC in 1996. The Task Force recommended that a primary goal at the 75th percentile for this year, or 37%, would be reasonable. However, in 2004, the rate of attempted VBAC declined to 9.2%. Unless there is a dramatic change in the delivery of obstetric care in the United States, the rate of VBAC attempts likely will continue to decline. Clearly, efforts to address the cesarean delivery rate in the United States have been found to be a daunting challenge.
Etiology of Dystocia
Traditionally, the causes of abnormal labor have been attributed to the “powers” (uterine contractility), the “passage” (maternal pelvimetry), and/or the “passenger” (position and size of the fetus). In more scientific terms, these represent a primary dysfunctional labor, cephalopelvic or fetopelvic disproportion, abnormal fetal head position, and asynclitism. This section evaluates each of these potential causes of dystocia. The generic term failure to progress often is used as a diagnosis to justify cesarean delivery and is more appropriately used as a sign of an underlying problem and does not represent a diagnosis. Hence, “failure to progress” is not sufficient to describe the labor problem and should not be used.
Primary Dysfunctional Labor
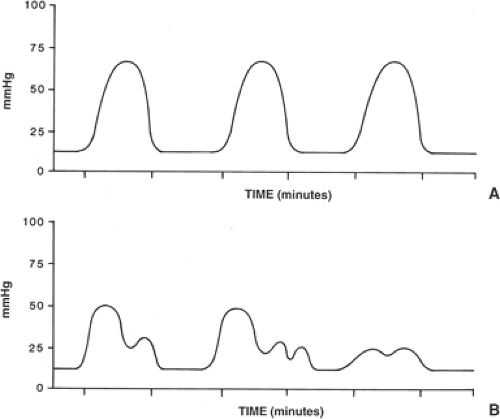
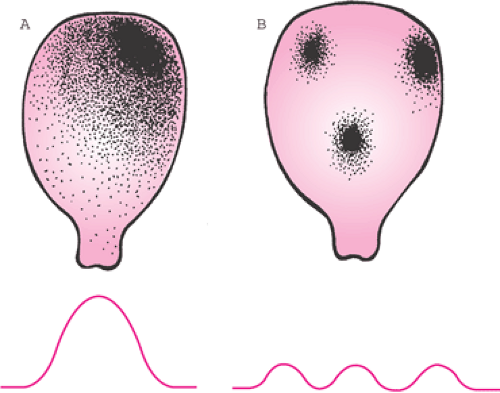
Primary dysfunctional labor refers to inadequate uterine contractility to maintain appropriate progress in labor. In general, an adequate uterine contraction pattern is one in which there are four to five concerted synchronous contractions every 10 minutes (Fig. 24.4). However, some women contract less frequently and continue to progress adequately in labor such that no intervention or treatment is required. Unlike the cardiac conduction system, the uterus has no defined nervous system for the conduction of electric signals to stimulate muscle contractions. The readiness of the uterus for labor is heralded by the occurrence and widespread distribution of gap junctions throughout the myometrium. Gap junctions allow for the rapid transmission of calcium fluxes through the uterine musculature and, hence, the occurrence of global uterine contractions. The uterus commonly has focal contractions throughout pregnancy (Braxton Hicks contractions), which are not of
sufficient strength or duration to effect cervical change and therefore do not constitute labor.
sufficient strength or duration to effect cervical change and therefore do not constitute labor.
Smooth muscle cells of the uterus are not randomly distributed but are arranged in a specific fashion such that maximal force can be generated to effect vaginal delivery. In women with uterine embryologic abnormalities such as uterus didelphys and bicornuate uterus, labor is not often successful in achieving vaginal delivery, as global, concerted uterine contractions cannot occur because of the abnormal arrangement of uterine smooth muscle cells. Similar problems may be noted in women exposed to diethylstilbestrol (DES) in utero with uterine anomalies characteristic of this teratogen (e.g., T-shaped uterus).
In the structurally normal uterus, contractions begin to occur less randomly days to weeks before the initiation of labor. Moreover, there is a distinct diurnal variation of uterine contractility such that in most women, uterine contractions occur more frequently and labor most often commences at night. These rhythmic variations may be the result of hormonal patterns in which specific and predictable changes in different hormones (e.g., corticotropin-releasing hormone, cortisol, progesterone, estradiol) allow for more frequent and stronger uterine contractions until the final signal for labor. While the precise nature of this signal in women is not known, cortisol appears to play a key role in the initiation of parturition.
As the normal uterus approaches term and the labor commences, different foci for the initiation of a uterine contraction may be present (Fig. 24.5). This phenomenon often leads to the clinical scenario in which some contractions are quite hard and lengthy whereas other contractions are mild and of short duration. Women will have mild contractions interspersed with firmer, more painful contractions because of the lack of a dominant “pacemaker” in the uterine musculature. While the uterus does not have a sophisticated electrical conduction system, cellular communication through gap junction formation allows for specific foci in the uterine smooth muscle from which contractions commence. Eventually, as labor progresses, one of these foci of uterine contractility predominates over other foci, resulting in more concerted and painful uterine contractions. As this occurs, true labor commences with effacement and dilation, and this change is reflected in the uterine tocodynometry patterns (Fig. 24.4). In a primary dysfunctional labor, uterine activity shifts from the concerted global contractions to more focal and less efficient contractions by allowing the reemergence of other pacemaker foci (Fig. 24.5). Medical therapy with oxytocin often is effective at correcting the underlying pathophysiology and restoring the pattern of global and concerted uterine contractions.
Although usually quite effective, oxytocin therapy may be of little benefit if the woman has intrauterine infection complicating labor. If the parturient has clinical signs of intrauterine infection, then labor progress often is desultory and not remedied with oxytocin augmentation, leading to a cesarean delivery rate of approximately 30% to 35% in these cases. Clinical signs of intrauterine infection include maternal fever (>38°C), fetal tachycardia (baseline fetal heart rate of >160 beats per minute), elevated maternal white cell count, uterine tenderness when the uterus is relaxed, and foul-smelling vaginal discharge. With the diagnosis of intrauterine infection, broad-spectrum antimicrobial agents should be administered and uterine activity stimulated with oxytocin if labor is not progressing adequately. Because oxytocin often does not work well in this scenario, the obstetrician should be prepared to move to cesarean delivery if oxytocin is ineffective in order to avoid neonatal infectious morbidity.
Cephalopelvic Disproportion
True cephalopelvic disproportion (CPD), or fetopelvic disproportion, commonly is diagnosed on the labor and delivery suite, although some authorities believe that CPD occurs in as few as 1 in 250 pregnancies. CPD occurs when the fetal birth weight or the fetal head is of sufficient size or orientation to preclude entry into the maternal pelvic inlet. This diagnosis often is made in retrospect after the birth weight is known and the positioning of the fetal head has been determined at the time of cesarean delivery. However, in the United States, the term cephalopelvic disproportion is used to describe almost any unsuccessful attempt at vaginal delivery. Further, the diagnosis of CPD often is used when labor progress is not sufficient and medical therapy is not successful or even not attempted. These cases often reflect inadequate use of oxytocin and are not problems with large fetal size or a small maternal pelvis. CPD is an important diagnosis because it has prognostic information for subsequent pregnancies when VBAC is considered. In women
with a prior diagnosis of CPD, success rates of VBAC are only 50%. Additionally, these women should be managed differently during the VBAC, with prompt repeat cesarean if labor does not progress appropriately.
with a prior diagnosis of CPD, success rates of VBAC are only 50%. Additionally, these women should be managed differently during the VBAC, with prompt repeat cesarean if labor does not progress appropriately.
Another important contribution to the fetopelvic relationship is the size of the fetus. Pregnancies with macrosomic fetuses (>4,000 g birth weight) have a greater risk of cesarean delivery for dystocia as a result of true CPD. In a study by Turner and colleagues, fetal macrosomia was associated with longer first and second stages of labor, a greater need for oxytocin therapy, and a greater risk for cesarean delivery for CPD refractory to oxytocin. In their patient population, the overall incidence of cesarean delivery of 5.2%, but if birth weight was between 4,000 and 4,500 g, the incidence of cesarean delivery was 13.8%. Also, forceps delivery was employed in 31.8% of infants with a birth weight between 4,000 and 4,500 g, whereas forceps were used in 13.6% of deliveries overall.
Unfortunately, there are no good predictors of fetal weight to guide management. Sonographic estimates of fetal weight at term are notoriously spurious and can miscalculate birth weight by up to 20%. The obstetrician employing Leopold maneuvers to estimate fetal weight by palpation of the maternal abdomen can only estimate small, average, or large fetal size. Hence, it is not advisable to induce labor or perform a cesarean delivery for presumed macrosomia unless the obstetrician judges that a dangerous situation exists for vaginal delivery (e.g., high risk of shoulder dystocia). Numerous studies of induction of labor for presumed macrosomia consistently show an increase in the cesarean delivery rate with no decrease in neonatal morbidity or shoulder dystocia.
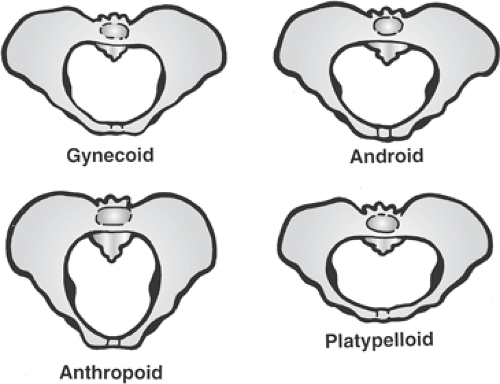
When the diagnosis of a labor abnormality is made, clinical pelvimetry should be performed to assess the dimensions of the maternal pelvis (Fig. 24.6). Only in the rare cases in which the maternal pelvis is markedly small or if there is clear CPD should cesarean delivery be performed without the prior use of oxytocin. For example, labor through a platypelloid pelvis with a normal term-sized fetus is rarely successful because of the markedly shortened anterior–posterior diameter that characterizes this pelvic architecture. After assessment of the pelvic type, approximations of the fetal size should be undertaken. Unless the fetus appears to be markedly macrosomic (>4,500 g), medical therapy with oxytocin should be instituted.
Abnormal Position of the Fetal Head
Abnormal positions of the fetal head include occiput posterior (OP), deep transverse arrest, and deflexion abnormalities such as face and brow presentations and reflect fundamental abnormalities in the cardinal movements of labor. Different positions of the fetal head are depicted in Figure 24.7. An OP position is unfavorable for successful vaginal delivery, particularly if the parturient has an android pelvic structure, as the long diameter of the fetal head negotiates the maternal pelvis at a relatively high station, leading to poor descent. The OP position may occur in up to 10% of women in labor and can be corrected with oxytocin therapy. According to Cheng and associates, associated factors for OP position include epidural use, amniotomy, African American race, nulliparity, and birth weight >4,000 g. Operative vaginal delivery, either via a Scanzoni maneuver or via a straight OP application with traction, is another option for delivery. A Scanzoni maneuver involves rotating the OP fetus to an OA position with forceps and then completing the delivery with forceps from the OA position. A Scanzoni maneuver is associated with a higher incidence of maternal trauma (third- and fourth-degree lacerations of the perineum and sulcus tears of the vagina) and fetal
trauma. Hence, such deliveries should be performed only by obstetricians skilled in these techniques and thus have largely fallen into disfavor. Moreover, delivery of the OP fetus via forceps should probably be attempted only if the fetal head has attained at least a +2 station. At higher stations, cesarean delivery may be the safest alternative. The prudent obstetrician will realize that assigning station in a labor characterized by an OP position is more difficult than in an OA position and often leads to the impression of a lower station than actually is present. Care should be taken to accurately assess the biparietal diameter in relationship to the maternal ischial spines.
trauma. Hence, such deliveries should be performed only by obstetricians skilled in these techniques and thus have largely fallen into disfavor. Moreover, delivery of the OP fetus via forceps should probably be attempted only if the fetal head has attained at least a +2 station. At higher stations, cesarean delivery may be the safest alternative. The prudent obstetrician will realize that assigning station in a labor characterized by an OP position is more difficult than in an OA position and often leads to the impression of a lower station than actually is present. Care should be taken to accurately assess the biparietal diameter in relationship to the maternal ischial spines.
A deep transverse arrest occurs in the second stage, where the fetus maintains an OT position at a low pelvic station. Deep transverse arrests often are associated with abnormal maternal pelvic architecture and may not be easily delivered via forceps. Kielland. forceps were designed to address the problem of the deep transverse arrest. Vacuum delivery probably should be avoided in this circumstance, as excessive traction of the fetus with a deep transverse arrest can result in significant birth trauma. Cesarean delivery is the most prudent option if the fetal station is not sufficiently low for operative vaginal delivery or if excessive traction is required to effect delivery. Operative vaginal delivery for a deep transverse arrest should be performed only by obstetricians skilled in the use of forceps for this problem.
Deflexion abnormalities also cause dystocia. The classic forms of deflexion abnormalities include brow and face presentations. Typically, a brow presentation is characterized by the long axis of the fetal head negotiating the short axis of the midpelvis, precluding vaginal delivery. A fetus in the brow presentation may spontaneously convert to a vertex or face presentation. Whereas fetuses with a brow presentation that do not convert rarely deliver vaginally (except in women with generously sized midpelvic dimensions with a small fetus), face presentations often will deliver vaginally if the mentum, or chin, is positioned anteriorly (mentum anterior). Although these extreme flexion abnormalities usually are easily diagnosed and are relatively rare, other mild flexion abnormalities may not be so readily evident. Flexion abnormalities may be suspected in a prolonged or protracted labor that is unresponsive to oxytocin. Unfortunately, there are no safe and accepted means to correct flexion abnormalities of the fetal head.
Often, abnormal fetal position may occur as the result of the maternal pelvic type (Fig. 24.6). For example, android pelvic types often lead to deep transverse arrest or OP position because of the progressive narrowing of the pelvis. Women with an anthropoid pelvis tend to have fetal positions persistently OA or OP, thus interfering with the normal cardinal movements of labor. Finally, women with a true platypelloid pelvis have transverse arrests, assuming that the fetal head negotiates the shortened pelvic inlet. Because many women have mixed pelvic types, careful clinical pelvimetry may provide valuable information in the management of dystocia.
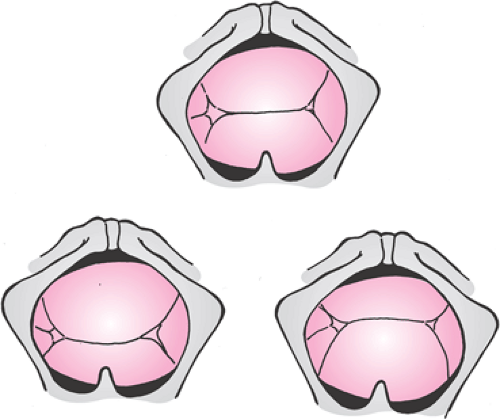 Figure 24.8 Synclitism. The term synclitism
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|