Background
Despite a lack of evidence showing improved clinical outcomes with robotic-assisted hysterectomy over other minimally invasive routes for benign indications, this route has increased in popularity over the last decade.
Objective
We sought to compare clinical outcomes and estimated cost of robotic-assisted vs other routes of minimally invasive hysterectomy for benign indications.
Study Design
A statewide database was used to analyze utilization and outcomes of minimally invasive hysterectomy performed for benign indications from Jan. 1, 2013, through July 1, 2014. A 1-to-1 propensity score-match analysis was performed between women who had a hysterectomy with robotic assistance vs other minimally invasive routes (laparoscopic and vaginal, with or without laparoscopy). Perioperative outcomes, intraoperative bowel and bladder injury, 30-day postoperative complications, readmissions, and reoperations were compared. Cost estimates of hysterectomy routes, surgical site infection, and postoperative blood transfusion were derived from published data.
Results
In all, 8313 hysterectomy cases were identified: 4527 performed using robotic assistance and 3786 performed using other minimally invasive routes. A total of 1338 women from each group were successfully matched using propensity score matching. Robotic-assisted hysterectomies had lower estimated blood loss (94.2 ± 124.3 vs 175.3 ± 198.9 mL, P < .001), longer surgical time (2.3 ± 1.0 vs 2.0 ± 1.0 hours, P < .001), larger specimen weights (178.9 ± 186.3 vs 160.5 ± 190 g, P = .007), and shorter length of stay (14.1% [189] vs 21.9% [293] ≥2 days, P < .001). Overall, the rate of any postoperative complication was lower with the robotic-assisted route (3.5% [47] vs 5.6% [75], P = .01) and driven by lower rates of superficial surgical site infection (0.07% [1] vs 0.7% [9], P = .01) and blood transfusion (0.8% [11] vs 1.9% [25], P = .02). Major postoperative complications, intraoperative bowel and bladder injury, readmissions, and reoperations were similar between groups. Using hospital cost estimates of hysterectomy routes and considering the incremental costs associated with surgical site infections and blood transfusions, nonrobotic minimally invasive routes had an average net savings of $3269 per case, or 24% lower cost, compared to robotic-assisted hysterectomy ($10,160 vs $13,429).
Conclusion
Robotic-assisted laparoscopy does not decrease major morbidity following hysterectomy for benign indications when compared to other minimally invasive routes. While superficial surgical site infection and blood transfusion rates were statistically lower in the robotic-assisted group, in the absence of substantial reductions in clinically and financially burdensome complications, it will be challenging to find a scenario in which robotic-assisted hysterectomy is clinically superior and cost-effective.
Introduction
Over the last decade, the popularization of robotic-assisted laparoscopic hysterectomy has provided an alternative approach to performing minimally invasive hysterectomy. While the decrease in abdominal hysterectomy rates seen over this same time period is indeed a positive trend, the superiority of the robotic-assisted route over other minimally invasive surgical (MIS) routes for benign hysterectomy has yet to be proven. Although cited benefits of the robotic-assisted route over conventional laparoscopy include lower estimated blood loss and shorter length of stay, complication rates appear to be similar and costs significantly higher with robotic technology. Vaginal hysterectomy remains the preferred route when possible and is recommended as such by the American Congress of Obstetricians and Gynecologists. However, few comparative studies of robotic hysterectomy actually include vaginal approaches. A retrospective study by Orady et al reported shorter operative time and greater blood loss with vaginal vs robotic hysterectomy. While major complication rates were comparable, this study was likely underpowered to detect some differences due to its small sample size.
Because complication rates following hysterectomy are relatively low, analyzing large clinical or administrative data sets is the only realistic way to evaluate differences in outcomes between MIS approaches. Therefore, using data from a statewide quality improvement collaborative, our aim was to compare perioperative outcomes and complications of hysterectomies performed for benign indications with robotic assistance vs all other MIS routes, including conventional laparoscopy, vaginal, and laparoscopic-assisted vaginal routes. As a secondary aim, we sought to compare estimated costs of robotic-assisted laparoscopy to all other MIS routes using published cost data.
Materials and Methods
We performed a retrospective study using data from the Michigan Surgical Quality Collaborative (MSQC), a Blue Cross Blue Shield of Michigan/Blue Care Network–funded database voluntarily populated by both academic and community hospitals throughout the state. Data are abstracted from charts by specially trained, dedicated nurse abstractors. Patient characteristics, intraoperative processes of care, and 30-day postoperative outcomes from hysterectomy cases at member hospitals are routinely collected. To reduce sampling error, a standardized data collection methodology is employed that uses only the first 25 cases of an 8-day cycle (alternating on different days of the week for each cycle). Routine validation of the data is maintained by scheduled site visits, conference calls, and internal audits. The University of Michigan Institutional Review Board granted “not regulated” status to this study (HUM00073978).
Hysterectomies available from the MSQC database and performed for benign indications using a MIS route from Jan. 1, 2013, through July 1, 2014, were analyzed as part of the study. Minimally invasive hysterectomy cases were dichotomized into those performed using robotic-assisted laparoscopy and all others (vaginal, laparoscopic-assisted vaginal, and conventional laparoscopy). Bivariate analyses were used to compare the following clinical and demographic characteristics between robotic-assisted and other MIS routes: age (years), body mass index (kg/m 2 ), race, smoker, hypertension, American Society of Anesthesiologists (ASA) class, age-adjusted Charlson Comorbidity Index (CCI), prior pelvic surgery, insurance type, teaching hospital, and hospital bed size. The CCI is a validated scoring system used to stratify patients based on specific comorbidities and age at admission for surgery. A higher CCI score indicates increased severity of condition and is correlated with increased 10-year mortality. Insurance type was categorized as follows: private, Medicare, Medicaid, both Medicare and Medicaid, uninsured, missing, and other. The “other” category included self-pay, government-sponsored plans excluding Medicare or Medicaid (eg, Department of Veterans Affairs, TRICARE), workers’ compensation, and auto insurance.
Propensity score matching was performed to minimize selection bias and control for clinically relevant variables. Using the demographic, clinical, and hospital factors described above in a multivariable logistic regression model, a propensity score ranging from 0-1 was generated for each case. A 1-to-1 propensity score-match analysis using a caliper of 0.001 was performed between women who had a hysterectomy using robotic assistance vs other MIS routes. The matches between groups were assessed with a standardized difference score ≤0.1 for every covariate considered to indicate a good match. Perioperative variables including estimated blood loss (milliliters), surgical time (hours), specimen weight (grams), and length of stay (days), as well as surgical complications, were compared between the propensity score-matched cohorts. Intraoperative complications included those involving the bowel and bladder. Postoperative complications within 30 days of the hysterectomy included: superficial surgical site infection (SSI), deep/organ space SSI, deep venous thromboembolism, pulmonary embolism, myocardial infarction/stroke, pneumonia, sepsis, urinary tract infection, and blood transfusion. “Any complication” included occurrence of any of the previously listed intraoperative or postoperative complications. “Major postoperative complications” included the following: deep/organ space SSI, deep venous or pulmonary embolism, myocardial infarction/stroke, pneumonia, sepsis, and death. “Any SSI” included both superficial and deep/organ space SSI. Hospital readmission and reoperation were also compared between the 2 groups. The paired t test was used for continuous variables and χ 2 for categorical variables.
For variables significant in pairwise comparisons between the robotic and other MIS groups, we subdivided the other MIS group into vaginal, laparoscopic-assisted vaginal, and laparoscopic routes. Overall comparisons with the robotic group were calculated and then pairwise comparisons between each specific route and the robotic group were performed. Overall P values for continuous variables were calculated using analysis of variance. P values for continuous variables with robotic hysterectomies as referent surgical approach were calculated using generalized linear models with Dunnett-Hsu post-hoc P value adjustment for multiple pairwise comparisons. Significance was assessed for categorical variables using χ 2 test or, in the case of small cell sizes, Fisher exact test. For categorical variables, multiple pairwise comparisons were initially calculated using χ 2 tests or, in the case of small cell sizes, Fisher exact test with a post-hoc Sidak P value adjustment.
Cost estimates were derived from published data on hospital costs by hysterectomy route, SSI, and postoperative blood transfusion. The equation used to estimate cost differences between robotic-assisted and other MIS routes is presented in the Appendix . All statistical analyses were performed using software (SAS, Version 9.3; SAS Institute Inc, Cary, NC).
Materials and Methods
We performed a retrospective study using data from the Michigan Surgical Quality Collaborative (MSQC), a Blue Cross Blue Shield of Michigan/Blue Care Network–funded database voluntarily populated by both academic and community hospitals throughout the state. Data are abstracted from charts by specially trained, dedicated nurse abstractors. Patient characteristics, intraoperative processes of care, and 30-day postoperative outcomes from hysterectomy cases at member hospitals are routinely collected. To reduce sampling error, a standardized data collection methodology is employed that uses only the first 25 cases of an 8-day cycle (alternating on different days of the week for each cycle). Routine validation of the data is maintained by scheduled site visits, conference calls, and internal audits. The University of Michigan Institutional Review Board granted “not regulated” status to this study (HUM00073978).
Hysterectomies available from the MSQC database and performed for benign indications using a MIS route from Jan. 1, 2013, through July 1, 2014, were analyzed as part of the study. Minimally invasive hysterectomy cases were dichotomized into those performed using robotic-assisted laparoscopy and all others (vaginal, laparoscopic-assisted vaginal, and conventional laparoscopy). Bivariate analyses were used to compare the following clinical and demographic characteristics between robotic-assisted and other MIS routes: age (years), body mass index (kg/m 2 ), race, smoker, hypertension, American Society of Anesthesiologists (ASA) class, age-adjusted Charlson Comorbidity Index (CCI), prior pelvic surgery, insurance type, teaching hospital, and hospital bed size. The CCI is a validated scoring system used to stratify patients based on specific comorbidities and age at admission for surgery. A higher CCI score indicates increased severity of condition and is correlated with increased 10-year mortality. Insurance type was categorized as follows: private, Medicare, Medicaid, both Medicare and Medicaid, uninsured, missing, and other. The “other” category included self-pay, government-sponsored plans excluding Medicare or Medicaid (eg, Department of Veterans Affairs, TRICARE), workers’ compensation, and auto insurance.
Propensity score matching was performed to minimize selection bias and control for clinically relevant variables. Using the demographic, clinical, and hospital factors described above in a multivariable logistic regression model, a propensity score ranging from 0-1 was generated for each case. A 1-to-1 propensity score-match analysis using a caliper of 0.001 was performed between women who had a hysterectomy using robotic assistance vs other MIS routes. The matches between groups were assessed with a standardized difference score ≤0.1 for every covariate considered to indicate a good match. Perioperative variables including estimated blood loss (milliliters), surgical time (hours), specimen weight (grams), and length of stay (days), as well as surgical complications, were compared between the propensity score-matched cohorts. Intraoperative complications included those involving the bowel and bladder. Postoperative complications within 30 days of the hysterectomy included: superficial surgical site infection (SSI), deep/organ space SSI, deep venous thromboembolism, pulmonary embolism, myocardial infarction/stroke, pneumonia, sepsis, urinary tract infection, and blood transfusion. “Any complication” included occurrence of any of the previously listed intraoperative or postoperative complications. “Major postoperative complications” included the following: deep/organ space SSI, deep venous or pulmonary embolism, myocardial infarction/stroke, pneumonia, sepsis, and death. “Any SSI” included both superficial and deep/organ space SSI. Hospital readmission and reoperation were also compared between the 2 groups. The paired t test was used for continuous variables and χ 2 for categorical variables.
For variables significant in pairwise comparisons between the robotic and other MIS groups, we subdivided the other MIS group into vaginal, laparoscopic-assisted vaginal, and laparoscopic routes. Overall comparisons with the robotic group were calculated and then pairwise comparisons between each specific route and the robotic group were performed. Overall P values for continuous variables were calculated using analysis of variance. P values for continuous variables with robotic hysterectomies as referent surgical approach were calculated using generalized linear models with Dunnett-Hsu post-hoc P value adjustment for multiple pairwise comparisons. Significance was assessed for categorical variables using χ 2 test or, in the case of small cell sizes, Fisher exact test. For categorical variables, multiple pairwise comparisons were initially calculated using χ 2 tests or, in the case of small cell sizes, Fisher exact test with a post-hoc Sidak P value adjustment.
Cost estimates were derived from published data on hospital costs by hysterectomy route, SSI, and postoperative blood transfusion. The equation used to estimate cost differences between robotic-assisted and other MIS routes is presented in the Appendix . All statistical analyses were performed using software (SAS, Version 9.3; SAS Institute Inc, Cary, NC).
Results
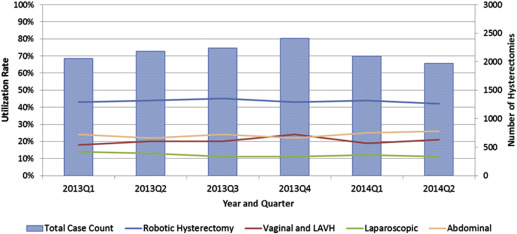
We identified 8313 cases of benign hysterectomy during the study period: 4527 performed using robotic assistance and 3786 performed using other MIS routes. The proportion of hysterectomies performed by route ranged from 43-45% for robotic assisted, 10-13% for laparoscopy, and 19-24% for vaginal, with or without laparoscopy ( Figure ). Prior to propensity score matching, groups differed significantly by nearly all demographic, clinical, and hospital factors ( Table 1 ). Compared to other MIS routes, women undergoing robotic-assisted hysterectomy were younger and more frequently non-Caucasian. They also had a higher mean body mass index and more frequently reported smoking. Comorbidities including hypertension and ASA class 3 were less frequent in women undergoing robotic-assisted hysterectomy, and these women also more frequently had prior pelvic surgery. Furthermore, a greater proportion of women having robotic-assisted hysterectomy had private insurance and significantly fewer had Medicare, no insurance, or other insurance. Finally, hospital characteristics differed between groups. Compared to other MIS routes, a greater proportion of robotic-assisted hysterectomies were performed at teaching hospitals and at those with <500 beds.