FIGURE 6-1 Mild, nonprogressive clinodactyly with radial deviation of small finger due to trapezoidal-shaped middle phalanx.
Clinodactyly of the index finger is a unique entity that presents at birth with marked deformity (Figure 6-2). It is often unilateral, with male predominance. It is commonly associated with brachydactyly and a hypoplastic trapezoidal or triangular middle phalanx. It is not associated with systemic anomalies or mental retardation. The index finger is usually radially deviated.2
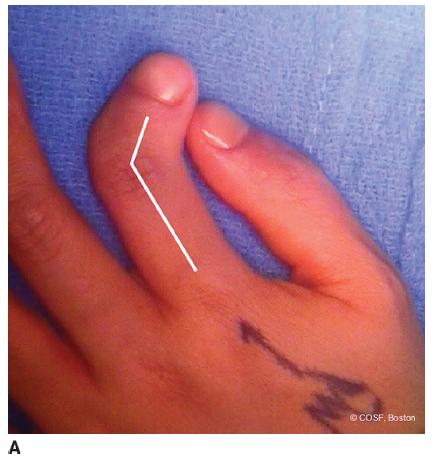
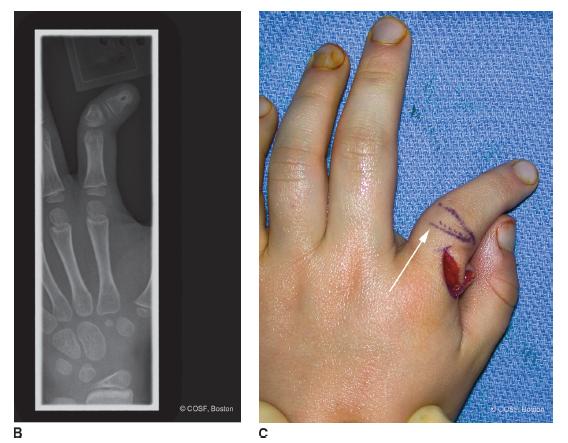
FIGURE 6-2 A: AP clinical view of index finger clinodactyly. Arrows outline deformity due to middle phalangeal delta phalanx B: Anteroposterior radiograph of same patient with middle phalanx bracketed epiphysis and distal phalanx partial duplication. C: Surgical correction. Z-plasty flaps are seen on the radial aspect of the index finger. Skin markings outline the planned corrective osteotomy (arrow).
Triphalangeal thumb is a unique form of clinodactyly in which the “extra bone” is triangular or trapezoidal shaped. This delta phalanx leads to malalignment of the thumb and, if severe, can impair pinch. Too much length with a rectangular extra phalanx can also impair thumb function. Inheritance is autosomal dominant. It is seen with other thumb malformations, such as thumb polydactyly. It is usually not seen with other systemic conditions or syndromes.
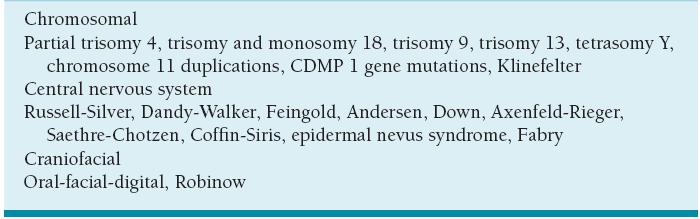
Associated syndromes and conditions are common. Delta phalanges and bracket epiphyses are often a part of other, more complex hand conditions (see Chapter 5). They are seen as a frequent part of chromosomal, central nervous system, and craniofacial abnormalities (Table 6.1). Many conditions that include symptoms of impaired intelligence have clinodactyly as part of their clinical spectrum. In utero ultrasound screening for Down syndrome includes clinodactyly as one of the diagnostic criteria. Clinodactyly of the thumb is seen most often with Rubinstein-Taybi syndrome, Apert syndrome, and dystro-phic dysplasia (hitchhiker thumb).
Table 6.1 Representative syndromes associated with clinodactyly (not exhaustive but representative)
Clinodactyly can be congenital (as above) or acquired. Acquired situations are due to physeal changes from trauma, infection, and benign tumors (intra-articular osteochondroma enchondroma) (Figure 6-3).3

FIGURE 6-3 Anteroposterior radiograph of middle finger clinodactyly secondary to intra-articular osteochondroma from middle phalanx ulnar condyle.
Camptodactyly
Camptodactyly by definition is a flexion posture or contracture of the PIP joint. Like clinodactyly, it usually involves the small finger and is often bilateral, though typically asymmetric (Figure 6-4). There is an autosomal dominant inheritance pattern of variable penetrance and expressivity with isolated small finger camptodactyly. Less than 1% of people have camptodactyly. Unlike clino dactyly, camptodactyly is usually secondary to soft tissue abnormalities. The most commonly implicated anatomic structures are the flexor digito-rum superficialis (FDS) and the lumbrical. The abnormal volar static and dynamic forces lead to skin, fascial, volar plate, check rein ligament, and collateral ligament tightness. Eventually bone and joint deformity develops (Figure 6-5). Camptodactyly often presents during periods of accelerated growth. Since infants usually double their size in the first 6 months and triple their size in the first year, this is a common time for presentation. Similarly, you can almost hear teenagers grow as they eat their way through their families’ refrigerators, so adolescents are the second-most common presenters of this condition to the office.

FIGURE 6-4 Lateral clinical view of mild small finger camptodactyly. Note normal PIP creases.

FIGURE 6-5 Lateral radiograph of clinodactyly demonstrating “parrot beaking” of proximal phalanx and flexion contracture of the PIP joint.
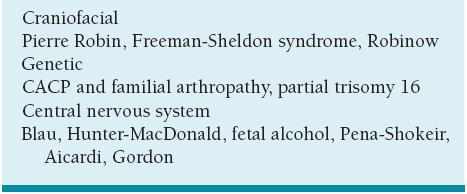
Camptodactyly is seen with other orthopaedic or generalized conditions. The most common orthopaedic condition with camptodactyly is arthrogryposis, usually involving multiple digits. Various types of skeletal dyspla-sias can have camptodactyly. Beal arachnodactyly is another syndrome that has associated PIP joint flexion contractures. Marfan syndrome has PIP joint flexion posturing. The extreme form of a flexion contracture at the PIP joint is symphalangism. Like clinodactyly, the associated syndromic conditions include genetic and craniofacial abnormalities (Table 6.2). There is a unique genetic condition described in Saudi Arabian families, the camptodactyly-arthropathy-coxa vara-pericarditis (CACP) syndrome. It is an autosomal recessive disorder caused by mutations in the proteoglycan 4 (PRG4) gene. Manifestations vary across families as well as between affected individuals from the same family, with digital camptodactyly and arthropathy of the knees the most ubiquitous, while pericarditis is evident in only one-fifth of all reported cases.4,5
Table 6.2 Representative conditions with associated camptodactyly (not exhaustive but representative)
Clinical Evaluation
About the only thing that comes to us without effort is old age.
—Gloria Pitzer
Clinodactyly
For both clinodactyly and camptodactyly, careful physical examination and thorough patient/parental counseling are critically important. In clinodactyly, measurement of the angular deformity from proximal to distal aspects of the digit through the point of maximum deformity is recorded. This is remeasured with each visit to assess progression, or lack thereof, with growth. The usual pathology is asymmetric longitudinal growth of the middle phalanx physis in the finger and proximal phalanx in the thumb. The quality of the volar digital flexion creases at the IP joints provides insight into the underlying bony architecture. In clinodactyly, the PIP and DIP converge on the radial side rather than remain parallel (Figure 6-6). You must distinguish between static and progressive deformity with growth over the first 5 to 10 years of life. If progressive and/or severe, the involved digit can overlap the adjacent digit during grasp and alter function. The most common situation is the small finger crossing over or under the ring finger. In the thumb, marked radial deviation impairs tip-to-tip pinch and allows for only lateral pinch against the ulnar aspect of the thumb IP joint. Similarly, index finger clinodactyly can impair pinch, though the deformity is almost always to the radial side. Radiographs define the bony architecture. Generally there is a delta phalanx or even a C-shaped longitudinal epiphyseal bracket.6,7 The triangular, trapezoidal, bracket-shaped epiphysis, or intra-articular osteochondroma of the involved phalanx, defines the deformity and guides surgical correction, if needed.
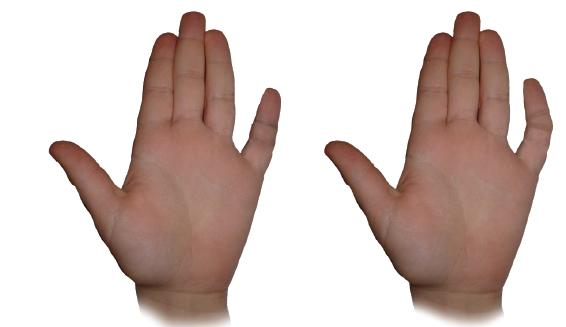
FIGURE 6-6 Illustration diagram of parallel and converging IP joint creases in normal and in clinodactyly.
Cooney classified clinodactyly as a combination of simple, complex, and complicated (Table 6.3). The deformity can be isolated with single bone involvement, complex involving multiple bones as a part of a congenital hand malformation, or complicated as a part of a systemic syndrome. The clinodactyly will either be static, remaining stable with growth, or progressive, eventually impairing hand function. With progression of the bone and joint deformity, a corresponding soft tissue contracture develops on the concave side of the digit. Unfortunately, there is no role for splinting or therapy in clinodactyly. A major issue for parents and patients is the cosmetic appearance. However, their concerns should not lead you to initiate “pointless” treatment8 or perform unnecessary and potentially problematic surgery.9 The preferred treatment for mild-to-moderate clinodactyly is to avoid surgery.
Table 6.3 Modified Cooney Classification
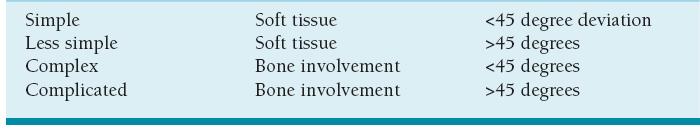
Adapted from Cooney, W P. Reconstruction of the Child’s Hand. Carter, P. ed. Philadelphia. Lea and Febiger. 1991, pp209-235.
Camptodactyly
The degree of PIP joint passive contracture, age of the patient, and general medical condition defines the camptodactyly. The passive limits of extension are recorded and monitored throughout growth and treatment. The degree of active PIP joint extension lag is compensated by MCP and DIP joint hyperextension in order to clear the digit from the palm and not interfere with adjacent digital function and release activities. This results in a highly functional situation because grasp remains strong, and release is not impaired, though differences in appearance remain.
The pathoanatomy is at the core of camptodactyly and usually relates to an abnormal FDS and/or lumbrical insertion and/or origin. The abnormal insertion of either of these structures pulls the PIP joint into flex-ion without balanced extension. The deformity can be flexible (usually early in course) or fixed. Fixed deformity implies shortened flexor tendon and sheath, contracted check rein and collateral ligaments, thickened volar plate, and possibly bony deformity. As with any intrinsic-extrinsic imbalance or MCP-IP joint cascade malalignment, the PIP flexion contracture must be assessed with varying degrees of wrist and MCP flexion and extension to define the pathoanatomy. In addition, you need to distinguish by exam the presence or absence of the small finger FDS and whether it is conjoined to the ring finger.
Presentation and progression usually occurs during periods of rapid growth acceleration, thus the classification system of infantile/congenital (type I), adolescent/acquired (type II), and syndromic (type III). In marked, fixed deformity, all the local anatomic structures become involved with contracture of the volar skin, fascia, collateral ligaments, volar plate, and flexor tendons. The extensor mechanism becomes attenuated and displaced. Eventually, deformity of the proximal phalangeal head and neck (flattening into a “parrot beak” deformity with loss of convexity) and middle phalanx base (flattening with asymmetric loss of concavity) develops with volar joint subluxation (Figure 6-5). At this stage, opportunity for successful intervention is more limited.
Differential diagnosis includes traumatic boutonniere deformity, inflammatory arthritis, juvenile palmar fibro-matosis, trigger fingers, arthrogryposis, Beal syndrome, pterygium syndrome, symphalangism, extensor tendon hypoplasia, congenital delta phalanx in flexion, and ulnar or C8-T1 neuropathy with clawing, among others.
Surgical Indications
The only thing I will remember from my hand fellowship when I am drooling on my chin in the nursing home is “Never operate on a PIP joint unless you have to.”
—Peter Waters countless times
Our advice is to leave mild-to-moderate clinodactyly and camptodactyly in your office, in the therapist’s office, and out of your operating room. Leave alone the deformities for which the other digits and a smart brain can compensate without thought or inefficiency of action. That said, marked deformity does need to be addressed. With clinodactyly, osteotomy of the involved phalanx coupled with skin rebalancing is the indicated intervention. With camptodactyly, soft tissue releases and rebalancing are most important, though often must be combined with bone and joint procedures. Knowing when you or someone else should do surgery is a major step on the congenital learning curve. Indicated surgeries are (1) camptodactyly >60 degrees that is unresponsive to stretching and splinting and (2) clinodactyly >30 degrees that interferes with grasp or pinch. Less clear indications are (1) physiolysis for progressive clinodactyly in children younger than 5 years and (2) camptodactyly between 30 and 60 degrees in a compliant family and patient.
SURGICAL PROCEDURES
 Splinting Techniques
Splinting Techniques
All the evidence obtained so far indicates there is no role for splinting in clinodactyly. Splinting and therapy will not correct bone or joint deformity in either clinodactyly or camptodactyly. However, passive extension stretching and splinting is the predominant treatment for most cases of camptodactyly. In infantile (type I) camptodactyly, the pathoanatomy is soft tissue contractures and muscle imbalance without bone and joint deformity. Progressive extension splinting with forearm-based orthoplast techniques have been effective in reducing and maintaining correction (Figure 6-7).9 Also, splinting with an active and passive range-of-motion program will often reduce the deformity to an acceptable level for function in an adolescent situation provided the patient is compliant. The splinting and therapy approach is also a good test of patient and family compliance with a tedious, methodical program of care. Without compliance, postoperative care will fail and greatly affect the outcome of any surgical intervention.
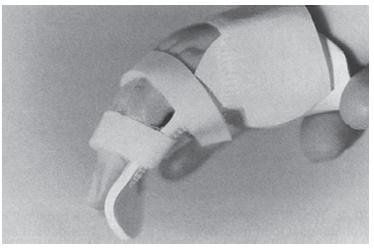
FIGURE 6-7 Illustration of a forearm-based, volar extension splint used for progressive static stretching of camptodactyly. (Reprinted from Benson 96 LS, Waters PM, Karnil NI, et al. Camptodactyly: classification and results of nonoperative treatment. J Ped Orthop. 1994;14(6):814– 819, with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


