Children in Motor Vehicle Collisions
Daniel J. Murphy
Through 1986, approximately 2 million persons have died and 100 million have been injured worldwide in motor vehicle collisions. It was estimated that between 1984 and 2000, at least 6 million more people died and 350 million were injured subsequent to vehicle collisions throughout the globe (1).
Motor vehicle collisions cause between 4 and 5 million injuries each year in the United States (2). Motor vehicle collision survivors lost 11 million work days in 1985 as the result of their injuries (3). A 1994 review reported that 2.3 million children were involved in motor vehicle collisions during a 2-year period (4).
In 2002 the largest clinical assessment of a group of children with whiplash-associated disorders to date was published (5). The authors found that 47% of children riding in cars who were involved in crashes developed whiplash-associated disorders. This study did not count children who were resuscitated or admitted as an in-patient to a hospital for their injuries, nor did it include children younger than age 4. Consequently, the number of injured children would be greater than 47%.
In 2007, an Australian group quantified pediatric spinal injury by age, mechanism, and severity (6). The authors looked at spinal trauma among children up to age 16 at two pediatric trauma hospitals. The authors reported that traffic-related incidents are a leading cause of spinal injury across all age groups, accounting for approximately one-third of all spinal trauma and half of all serious injuries. At 47%, the 0 to 4-year-old age group had the highest proportion of serious injuries. The upper cervical spine was more commonly seriously injured in young children, and the lower cervical spine was involved more often in older children. Soft tissue injuries were greater in those older than age 8. The authors acknowledge that children who sustained minor injuries and were not brought to a hospital were not included in the sample. Therefore, this “data underrepresents minor injuries.”
Motor vehicle-related deaths were the fourth leading cause of mortality in the United States in 1987, killing more than 47,000 people. An additional 1.8 million individuals sustained disabling injuries (7). Motor vehicle collisions resulted in 40,300 deaths in 1992, making them the seventh leading cause of death overall in the United States, and the first leading cause of death among those aged 1 to 30 years (8).
The U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (9), make the following statements:
More than 41,000 people in the United States die in motor vehicle crashes each year.
Crash injuries result in about 500,000 hospitalizations and four million emergency department visits annually.
The economic burden of motor vehicle-related deaths and injuries is enormous, costing the United States more than $150 billion each year.
Motor vehicle crashes are the leading cause of death among children in the United States.
Motor vehicle-related injuries kill more children and young adults than any other single cause in the United States.
In the United States during 2006, 1,335 children ages 14 years and younger died as occupants during motor vehicle crashes and approximately 184,000 were injured. That is an average of 4 deaths and 504 injuries each day.
Two out of five deaths among teens in the United States result from motor vehicle crashes.
Motor vehicle crashes are the leading cause of death for US teens, accounting for 36% of all deaths in this age group.
In 2004, a total of 4,767 teens ages 16 to 19 died of injuries caused by motor vehicle crashes.
In 2002, the estimated economic cost of policereported crashes (fatal and nonfatal) involving drivers ages 15 to 20 was $40.8 billion.
PATHOMECHANICS OF INJURY
Early research on motor vehicle collisions and its biological effects have used a variety of experimental designs, including the use of anthropomorphic dummies (10,11); primates (12,13,14); rabbits (15); mathematical modeling (16); unembalmed human cadavers (17); and human volunteers (10,11,18).
In 1955, Severy et al. (10,11) performed a series of controlled rear-end collisions using both anthropomorphic dummies and human volunteers. The subject vehicle was struck from behind by a vehicle that was traveling between 7 and 20 miles per hour. These studies are considered to be one of the earliest attempts to quantify the forceful effects of rear-end motor vehicle collisions on a vehicle’s occupants. These early research studies and more contemporary writings reveal several concepts regarding motor vehicle collisions.
Force of Impact
The forces produced by motor vehicle collisions are high. A rear-end collision at 8 miles per hour results in a 2-G acceleration acting on the impacted vehicle and a 5-G force acting on the occupant’s head (19,20,21). Rear-end collision speeds between 7 and 20 miles per hour can create head accelerations as great as 11.4 G (10,11,22,23). According to Barnsley et al. (24), an impact speed of 20 miles per hour causes the human head to reach a peak acceleration of 12 G during extension. A 5-G force of acceleration acting on the heads of primates resulted in a 50% probability of brain stem injury, cerebral concussion, and cranial nerve stretch (13,20). During frontal impacts at speeds of approximately 40 miles per hour, the vehicle decelerates at a force of 90 G while the head of an occupant is subjected to a deceleration force of 46 G (25).
Collision Time Sequence
The mechanism of a motor vehicle collision and its associated injury occurs in a very short span of time. Various studies indicate a range from 0.25 seconds (26,27) to 0.5 seconds (28) from impact to completion of the flexion/extension motions of the cervical spine. Consequently, because of this short time sequence even low-speed rear-end collisions may result in significant injury (28).
Vehicle Damage and Personal Injury
Vehicle speed and damage are not reliable indicators of injury to the occupants. This is supported by the writings and research of Jackson (29), Macnab (22), Carroll et al. (30), Ameis (31), Hirsch et al. (19), Navin and Romilly (32), Morris (33), Emori (34), Sturzenegger et al. (35), Robbins (36), Duffy et al. (37), Gun et al. (38), Pobereskin (39), and Cailliet (40). Macnab (22) has created a scenario in which a vehicle is stuck in concrete and badly damaged by a collision impact, yet the occupants are not injured because their vehicle could not move forward, and a scenario in which a vehicle on ice is undamaged by a collision impact yet the occupants sustain significant injury because of the rapid accelerations permitted.
Mechanism of Injury
The principle of inertia was first described by Sir Isaac Newton more than 300 years ago. Inertia is the tendency of an object at rest to want to remain at rest and to resist change in its resting status. Unfortunately, different parts of a human body, whether adult or child, will have different inertias. For example, the human head will function inertially differently than will the human torso. Specifically, if the torso is suddenly moved, the inertially independent head will tend to remain at rest. This creates mechanical stress on the tissue that is responsible for attaching these two functionally different inertial masses to one another: the cervical spine.
Inertia is also the tendency of an object in motion to want to remain in motion and to resist change in its motion status. Again, unfortunately, different parts of a human body, whether adult or child, will have different inertias. Specifically, if the human body is in motion and the torso is suddenly stopped, the inertially independent head will continue in motion. This will, once again, create mechanical stress on the cervical spine because it is responsible for attaching these two functionally independent inertial masses to one another.
Velocity is the changing of position as a function of time. An example would be driving one’s automobile 55 miles per hour. This would mean that one’s position would change 55 miles if that velocity was maintained for 1 hour. Velocity alone will not injure or adversely affect the tissues of the human body. Velocity is frequently not noticed by human consciousness as long as all the parts of one’s body are traveling at the same velocity (speed and direction). Planet Earth, with an approximate circumference of 24,000 miles, makes one complete revolution every 24 hours. This means that all of us are traveling at an approximate velocity of approximately 1,000 miles per hour, yet we remain consciously unaware of this motion. In an airplane, one may be traveling at a speed of 500 miles per hour, yet the conscious perceptions are not that different from sitting in a chair on the ground.
Changes in velocity are perceptible. This occurs when one experiences an increase or a decrease in speed. Recall the sensations of increasing speed when merging onto a freeway, or the sensation of decreasing speed that is experienced when an airplane lands on a runway. This increasing or decreasing speed over a period of time is referred to as acceleration or deceleration.
The most common cause of bodily injury during motor vehicle collisions happens when change in the velocity of a vehicle (acceleration or deceleration) occurs rapidly, which results in different acceleration/decelerations among the different inertial masses of the occupant’s bodies. Therefore, the basic mechanism of injury during motor vehicle collisions involves inertial acceleration differences between the different inertial parts of the occupant’s body (22,23,25,26,41).
Soft Tissue Injury
The basic injury is considered to be a soft tissue injury. This is supported by the writings of Macnab (22), Dunn and Blazar (23), Hirsch et al. (19), Chester (20), Barnsley et al. (25), Jónsson et al. (42), and Barnsley et al. (43), to name but a few. Fractures of the spine do occur, but they are rare. However, Walter et al. (44) notes that approximately 80% of all cervical spine fractures are the result of motor vehicle accidents (see Chapter 23). Occult fractures that do not demonstrate on standard radiographs are also noted. These occult fractures may not even manifest on high-resolution computed tomography (CT) scanning (25).
Injury Repair
Soft tissue injuries reported as a result of motor vehicle collisions and their subsequent pathologies are slow to resolve. Ameis (31) notes that mild soft tissue injuries from motor vehicle collisions achieve symptom-free status about 6 months after the injury. He also notes that moderate-category soft tissue injury reaches maximum improvement between 12 and 36 months after injury. Ameis (31) claims that 50% of injured patients recover by the end of the first year after injury, 75% recover at 18 months after injury, and 85 to 90% recover between 2 and 3 years, although some patients report recovery up to 5 years later.
Parmar and Raymakers (45) reported that 50% of patients who have soft tissue neck injuries caused by rear impacts have significant pain 8 months after injury; 44% have significant pain at 12 months after injury; 22% have significant pain at 2 years; 18% have significant pain at 3 years; and 14% have significant pain at 8 years.
Schofferman and Wasserman (46) treated patients with low back and neck pain after motor vehicle accidents with an aggressive physical therapy stabilization program. Their patients reached maximum improvement between 8 and 108 weeks, with a mean duration of treatment of 29 weeks.
Residual Injury
Motor vehicle collisions are associated with a high percentage of residual chronicity of symptoms. Ameis (31) notes that 40 to 70% of injured patients endure permanent mild persistence of symptoms.
A study by Hodgson and Drundy (47) involving 40 patients indicated that 62% of those injured in automobile accidents still have significant symptoms caused by the accident 12.5 years after being injured.
Nunn and Greenwood (48) write that follow-up studies of whiplash have shown that, with standard treatment, up to 50% of the patients have significant pain 5 years after injury.
Gargan and Bannister (49) reviewed 43 patients who had sustained soft tissue injuries of the neck. They noted that 10.8 years after injury only 12% of patients had completely recovered. Residual symptoms were intrusive in 28% of patients and were severe in another 12
Watkinson et al. (50) reviewed 35 patients and reported that, more than 10 years after soft tissue cervical spine injury, residual symptoms were found in 86% of patients and were significant in 23%.
Tomlinson et al. (51) prospectively followed 42 adult patients injured from whiplash for a mean of 7.5 years and found:
29% of the patients had no symptoms
48% had mild symptoms that did not interfere with work or leisure
21% had intrusive symptoms that interfered with work and leisure and required continued treatment and drugs
2% had severe problems that required ongoing medical investigations and drugs.
In an extensive review of published studies of motor vehicle collision patients, Barnsley et al. (25) state that chronic neck pain develops in approximately 14 to 42% of patients with whiplash injuries, and approximately 10% have constant severe pain indefinitely.
Permanent Functional Impairment
Motor vehicle collisions are associated with a high percentage of residual permanent functional impairments. Ameis (31) indicates that 10 to 15% of patients never functionally recover after moderate-category soft tissue injury caused by whiplash.
Hodgson and Drundy (47) have reported that 62% of those injured in automobile accidents were still
having symptoms 12.5 years after being injured and, of the symptomatic 62%, 44% changed to lighter work activities permanently, and 62.5% modified their leisure activities to avoid exacerbation of symptoms.
having symptoms 12.5 years after being injured and, of the symptomatic 62%, 44% changed to lighter work activities permanently, and 62.5% modified their leisure activities to avoid exacerbation of symptoms.
Inertial Acceleration Injuries
The five classic inertial acceleration injured regions associated with motor vehicle collisions are as follows:
Inertial acceleration injuries between the head and the trunk, which primarily injures the cervical spine (22)
Inertial acceleration injuries between the skull and the mandible, which injures the temporomandibular articulation (22,52,53,54)
Inertial acceleration injuries between stapes bone in the inner ear and adjacent structures, which disturbs the vestibular apparatus and its concomitant balance/postural mechanisms (20)
Inertial acceleration injuries between the pelvis and the trunk, which injures the lower back
These inertial injuries often are magnified by lap seat belts and are detailed later in this chapter.
Chronicity of Symptoms and Functional Impairment
Leading explanations for the probability of long-term recovery, residual subjectivity, and residual functional impairments are based on recent advances in neuroanatomy, histology, histopathology, and empirical responses of patients during various invasive clinical studies. Culprit tissues in patients with problems are not the usual muscular strain or ligamentous sprain; rather it is damage to the facet joint capsules and/or to the intervertebral disc. Barnsley et al. (25) note that a significant proportion of patients with injury after whiplash have chronic and unremitting symptoms reflecting serious damage to the zygapophyseal joints or the intervertebral discs.
Several contemporary authors have identified the annulus of the intervertebral disc as the source of chronic spine pain, including Nachemson (55), Mooney (56), and Kuslich et al. (57). Barnsley et al. (24) summarizes that injuries to the intervertebral disc from motor vehicle accidents have repeatedly been reported from a number of sources. Taylor and Twomey (58) gave histological proof that the annulus of the disc is injured in neck sprains caused by motor vehicle collisions. Jónsson et al. (42) reported a high number of discoligamentous injuries when reviewing a series of 50 patients with whiplash distortion.
Other contemporary authors have identified the zygapophyseal joints as the source of chronic posttraumatic spine pain. Barnsley et al. (24) note that the cervical zygapophyseal joints are damaged in whiplash injuries; there is remarkable consistency among experimental data from cadavers, radiographic findings operative findings, and postmortem studies. Lord et al. (27) note that, in experimental studies using animals or cadavers subjected to whiplash motions, injuries to the cervical zygapophyseal joints are among the most common and most consistent lesions produced. Postmortem studies of victims of motor vehicle accidents reveal that zygapophyseal joint injuries are present in 86% of the necks examined. In a rare double-blind study, Barnsley et al. (43) further confirmed the high incidence of chronic posttraumatic whiplash pain arising from the cervical zygapophyseal joints, with up to 68% probability.
In 1993, Bogduk and Aprill (59) concluded that among those with posttraumatic neck pain, 41% of the patients had both a symptomatic zygapophyseal joint and a symptomatic disc at the same level; 20% of the patients had a symptomatic disc alone and 23% had a symptomatic zygapophyseal joint alone. Addition of these numbers indicates that of patients with posttraumatic chronic neck pain, 61% have intervertebral disc involvement and 64% have zygapophyseal joint involvement. Only 17% of the patients in this study did not have a symptomatic disc or a symptomatic zygapophyseal joint.
Head Restraints
A properly fitted head restraint minimizes the extension injuries and dampens rebound flexion injuries that occur as a result of being struck from the rear (22,26,33,60,61,62). A properly fitted headrest is one that is sufficiently high enough to avoid accentuated head restraint fulcrum injuries and close enough to effectively minimize posterior head rotation and compression injuries. The head restraint must be at least as high as the center of mass of the skull and within 1 in. (25 mm) of the back of the skull (33,61,62). The majority of head restraints in current automobile models do not meet either criterion (26,60,61,62).
Seat Belts
Seat belts minimize certain types of injuries, especially serious injuries and death (63,64). When worn correctly, lap/shoulder belts used by front-seat passengers reduce the risk of fatal injury by 45% (7,8) and the risk of moderate to critical injury by 50%. A study by Newman (65) concluded that the incidence of serious injury and death in frontal impacts is dramatically reduced by the use of seat belts. Orsay et al. (3) reported a 60.1% reduction in the severity of injury, a 64.6% reduction in hospital admissions, and a 66.3% reduction in hospital
charges among seat belt wearers. Lap belts without a shoulder harness in the rear seats reduced fatalities 18 to 40%. Therefore, the installation of lap/shoulder seat belts in rear seats should be implemented (66). Worldwide fatalities of vehicle occupants have been reduced by an average of 40% among front seat occupants and 70% among rear seat occupants, if restrained. With the universal use of vehicle restraints, fatal collision statistics would decrease by approximately 50% (67). However, seat belts increase other types of injuries (68,69), including the following:
charges among seat belt wearers. Lap belts without a shoulder harness in the rear seats reduced fatalities 18 to 40%. Therefore, the installation of lap/shoulder seat belts in rear seats should be implemented (66). Worldwide fatalities of vehicle occupants have been reduced by an average of 40% among front seat occupants and 70% among rear seat occupants, if restrained. With the universal use of vehicle restraints, fatal collision statistics would decrease by approximately 50% (67). However, seat belts increase other types of injuries (68,69), including the following:
There are more fractures to the sternum in belted passengers (70).
There are more abdominal viscera injuries (70).
This increased incidence of other injuries occurs because, at the time of impact, the belt serves as a fulcrum, increasing belt-fulcrum injuries (68,69,78,79,80). Prepubertal children are particularly vulnerable.
Sato (81) states that seat belt users are likely to sustain injury with frontal impact at 18 km per hour (11.2 mph); those not using seat belts are likely to be injured in the same accident at only 5 km per hour (3.1 mph).
Improper use of seat belts increases injury. The two most noted improper uses are:
Wearing a belt that is too loose. This would increase probability of submarining beneath the belt, injuring the abdomen and the head with the shoulder harness portion of the belt. Motorists should not put more than 2 in. of slack in the shoulder belt (82).
Placing the belt too high on the abdomen. During a crash, the belt may impose a load 20 to 50 times greater than the body weight. The only part of the body that can withstand this heavy load is the bony pelvis.
Lumbar Spine Injury
Lumbar spine injuries occur in approximately 50% of those who are involved in motor vehicle collisions (83). Many of the lumbar spine injuries are related to belt fulcrum trauma.
Air Bags
Air bags reduce overall motor vehicle collision injuries, especially when used in conjunction with lap and shoulder belts. They minimize serious injuries from sudden deceleration events. Alone they reduce fatalities by 40%; when used with belt restraints, they reduce fatalities by 66% (66). The U.S. Department of Transportation estimates that the installation of air bags in all motor vehicles would save approximately 8,800 lives per year (84). Airbags do not inflate inadvertently, are reliable for years, require no maintenance, and, when used with the lap-shoulder restraint, provide the best possible occupant protection (85).
Air bags are associated with certain types of injuries. They have occasionally been implicated in abrasions to the face, neck, and chest. They may injure the eye, cause facial bruising, or injure the temporomandibular joint (86). Skin burns have been observed, caused by escaping gas (73). Rare cervical spine fractures have been documented (87). Serious injuries to infants in rear-facing restraint buckets have been observed (88).
Optimum Safety
Occupant safety during motor vehicle collisions is probably greatest with adequate head restraint, adequate belt restraint, and air bags (87).
Prognosis Factors
Other factors are frequently related to increased injury, slower recovery, and worse prognosis for individuals involved in motor vehicle collisions. These factors include:
The occupant being unaware of impending collision before impact; that is, the occupant is caught by surprise (27,28,34,35). This is an important factor to consider when assessing children because most children are unprepared for any collision. Sturzenegger claims that the patient’s state of preparedness is the most significant factor with respect to injury.
The occupant’s head being turned at the moment of impact or there being an oblique line of impact causing head rotation during the collision (21,35,43,89,90). There is a natural compromise of the intervertebral foramen and its neurovascular contents as well as the intervertebral disc and the capsules of the zygapophyseal articulations when the head is turned. When in this rotated position, certain accident mechanisms cause increased rotation before flexion or extension mechanisms, resulting in magnified compromise to the disc, facet capsules, the contents of the intervertebral foramen, etc.
Degenerative joint disease present before the accident (19,23,31,32,33,34,35,41,42,43,44,45,46,47,48,49,50,62,83,89,90,91,92). These degenerated articulations and tissues are less capable of adequately handling and dispersing the forces of a traumatic event, resulting in greater injury, more required care, increased chronicity, and accelerated degenerative joint disease (61).
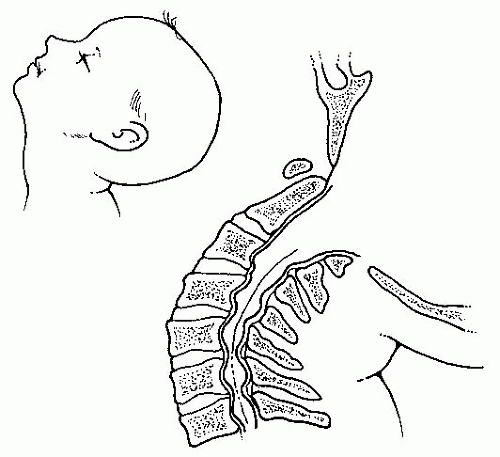
Central neural canal spinal stenosis present before the accident (83,93,94). The narrowing of the central neural canal before the collision reduces the space tolerance of the spinal cord and its coverings. This compromise and subsequent injury are greatest during extension/hyperextension movements because the central neural canal narrows during extension while the ligamentum flavum bulges anteriorly into the spinal cord, creating additional space impairment (Fig. 20-1). Some children have congenital central neural canal stenosis (61).
Litigation and Outcome
Litigation or its absence does not influence the long-term clinical outcome. Patients are not “cured by verdict.” Reviews of long-term clinical outcomes for patients after motor vehicle collision injuries show high incidence of residual chronicity and impairment years after settlement of the injury claims and when no possible additional monetary compensation was available (25,61,95). Using a different approach but arriving at the same conclusion, Schofferman and Wasserman (46) undertook a follow-up study of a group of litigants injured in motor vehicle collisions and noted that the majority improved or resolved with treatment despite their ongoing litigation. Many of the preceding principles also apply to children in crashes.
Summary
Individuals are injured in motor vehicle collisions. The nature of the injury falls under the rubric “soft tissue injury.” Fractures are rare, but they do occur, occult and otherwise. The type and severity of the injuries sustained cannot be determined by evaluating the damage to the patient’s vehicle or by understanding the speeds of the involved vehicles.
Seat belts minimize serious injury and fatalities but increase other injuries, such as neck sprain, abdominal viscera injury, lumbar spine belt fulcrum injury, and chest wall injuries. Seat belts do not reduce extension cervical spine injuries.
Proper head restraints minimize extension cervical spine injuries and dampen rebound flexion cervical spine injuries. A proper head restraint is close to the back of the occupant’s head (˜1 in.) and at least as high as the center of mass of the skull. If the head restraint is too low it may increase the patient’s extension injuries by functioning as a fulcrum.
Air bags prevent serious flexion or rebound flexion injuries. Air bags minimize the flexion of the head and cervical spine—something that shoulder harness seat belts will not do. Air bags will also minimize belt-induced chest wall, abdominal viscera, and lumbar fulcrum trauma. Air bags are not a panacea. They have been implicated in injuries to the temporomandibular joints and face, certain cervical spine fractures, and burns. However, injuries created by air bags are minor compared with those that occur without an air bag.
The extent of injury and the patient’s prognosis for recovery are influenced adversely when the patient is caught by surprise, when the head is rotated at the moment of impact, if the patient has congenital or acquired central canal spinal stenosis, and if there is degenerative joint disease present before the accident.
When the injured patient’s symptoms resolve in 2 to 3 months, the soft tissue injuries were probably to the muscles and noncapsular ligaments. When the injured patient requires many months to years to reach maximum improvement, the soft tissue injuries were probably to the zygapophyseal joint tissues, the intervertebral disc, or to a combination of the two. When maximum improvement is achieved, residual symptomatology is the rule. This residual symptomatology varies from a minor annoyance to severe enough to require a permanent alteration of work and leisure activities. Ten to 15% of motor vehicle collision patients with soft tissue injuries have indefinite, constant, severe pain and never achieve a full functional recovery. Litigation or its absence does not seem to influence the long-term clinical outcome or the patient’s eventual functional status.
PEDIATRIC INJURIES
Many of the concepts that pertain to adults in motor vehicle collisions also apply to children, including the basic principles of inertial acceleration/deceleration injuries, patient preparedness before impact, and rotation of the head or trunk before impact. Other concepts will be modified because of the uniqueness of child safety seats, the increased size of the pediatric head as a proportion of the overall body mass, the child’s ability to be restrained while facing the rear, the use of seat belts that are designed for adults, the use of lap belts without shoulder harnesses, the reduced height of the developing pediatric pelvis, the underdevelopment of the pediatric anterior superior iliac spine, the higher center of gravity in the pediatric body, the diminished development and strength of various spinal musculoskeletal components, and the ability to sit on the lap of adults when traveling in a vehicle. Overall, the pattern of injury among children in motor vehicle collisions is similar to those of the general population (96), excepting the differences noted below.
Injuries are the leading cause of death among children older than 1 year (4,97,98). Fifty percent of children between 1 and 14 years of age who died in the United States in 1980 died of injuries. Once a child is older than 12 months, injury becomes the leading cause of children’s doctor visits and the most common reason for admittance to the emergency department of hospitals (97,99). Motor vehicle accidents are the most frequent cause for these injuries to children and young adults (98).
The 1993 edition of “Accident Facts” by the National Safety Council indicates that, in 1992, 40,300 deaths and 2,200,000 disabling injuries occurred from motor vehicle accidents, with the total associated costs estimated to be $156.6 billion. Eight thousand three hundred students were injured from school bus accidents from 1991 to 1992. In 1990, 40.8% of all reported automobile occupant injuries were contusions; 17% were lacerations; 12.7% were abrasions; 11.8% were strains; 7.4% were fractures; and 4.2% were concussions. Of the strains, 66.9% were to the neck and 25.1% were to the back. Of the 40,300 deaths related to motor vehicle collisions in 1992, 5.1% were among children younger than 5 years and 4.9% were among children between the ages of 5 to 14 years.
Accidental injury overshadows all other causes of death among children. North American statistics consistently show that over the past 35 years motor vehicle collisions have been the leading cause of mortality and morbidity among children aged 1 to 14 years (4,100). In the 1970s, before child restraint laws, 16,820 children aged 0 to 4 years were killed in motor vehicle accidents (101). Motor vehicle collisions account for 37 to 50% of the deaths among children and lead to significant morbidity among those who survive the collision (102,103). Each year, twice as many children are injured or killed while inside automobiles as are injured or killed outside automobiles (104). More children in the United States die from automobile trauma than from any disease (85). One in every 48 children born in the United States will die in a motor vehicle collision before the age of 25 and one in every 20 children born in the United States will be seriously injured in a motor vehicle collision (85).
Among children, motor vehicle collisions contribute to an even greater proportion of injuries and deaths than in adults. Injury related to motor vehicles is the major cause of mortality among the pediatric population in the United States (4,7,105,106) and resulted in approximately 2,000 fatalities per year before the enactment of most state child restraint laws (107). Alcoff (105) notes that it has been estimated that a young child is 40 to 50 times more likely to die from injuries sustained in a car crash than from all the common childhood diseases against which children are immunized. He notes that in 1973, 116 Americans of all ages died of measles, mumps, rubella, polio, diphtheria, pertussis, and tetanus combined, whereas that same year, 1,988 children younger than 5 years were killed in vehicular collisions. Even after the enactment of child restraint laws, more than 600 infants younger than 5 years were killed in motor vehicle collisions in 1989 in the United States (85). The rate of child involvement in vehicle collisions is 21.4 per 1,000 per year. The rate of child injury from vehicle collisions is 4.76 per 1,000 per year, with the highest rate of injury in 3-year-old children (4).
Approximately 700 infants and toddlers were killed in automobile accidents in 1994, and another 75,000 were injured. Only about 60% of children consistently ride in car seats and as many as 25% of them are not buckled in properly (108).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree