Cervical Spine Immobilization and Imaging
George A. Woodward
Nanette C. Dudley
Introduction
Cervical spine injuries, fortunately, are uncommon in the pediatric population. It has been estimated that cervical spine injuries occur in only 1% to 2% of pediatric patients with multiple trauma (1). However, the potentially devastating consequences of a cervical spine injury mandate proper immobilization and evaluation of all children who might have sustained such injuries. The purpose of cervical spine immobilization is to prevent the occurrence or exacerbation of spinal cord injury in the child with an unstable cervical spine. A variety of techniques may be used to attempt cervical spine immobilization, although some of these are more effective than others.
Mechanisms of injury most often associated with cervical spine damage in children include motor vehicle collisions, sports (contact, high-force activities), falls, diving accidents, and difficult newborn deliveries (breech, forceps) (2) (Table 24.1). All multiple trauma victims and those who have experienced a high-risk mechanism of injury should have cervical spine immobilization and evaluation.
To be effective and prevent secondary or ongoing injury, proper immobilization and care of the cervical spine should be started as soon as possible and continued until significant cervical spine injury has been excluded. Although cervical spine injuries can be devastating, necessary airway management and stabilization should not be delayed while awaiting formal cervical spine evaluation. Furthermore, there are at least two types of cervical spine immobilization, immobilization pending formal cervical spine evaluation and immobilization used for procedures like airway management. This chapter addresses these and other methods of cervical spine immobilization.
Anatomy and Physiology
The pediatric cervical spine is similar to the adult’s in that it can be anatomically divided into two sections (3). The anterior cervical spine is bordered by the anterior and posterior longitudinal ligaments and contains the bodies of the cervical vertebrae as well as the intervertebral disks. The posterior cervical spine includes the pedicles, lamina, spinous processes, and facet joints and the remainder of the cervical ligaments. Disruption of bony or ligamentous elements can potentially lead to an unstable cervical spine.
The child’s cervical spine differs in many ways from that of the adult (2,4,5) (Table 24.2). The infant’s large head and relatively weak neck muscles cause the fulcrum of the neck to be at C2-3, compared with C5-6 in the adult. Therefore, younger children tend to have upper cervical spine fractures whereas older children and adolescents have fractures in lower cervical
spine regions, similar to adults (6). The large amount of cartilage in the pediatric cervical spine cushions direct vertical forces and limits the occurrence of bursting or compression-type fractures. The radiolucent cartilaginous component of the pediatric cervical spine, however, can make radiographic evaluation challenging. Children have more horizontal facet joints and increased ligamentous laxity, allowing for increased anterior and posterior motion of the cervical spine. This flexibility allows for significant spine distortion during the traumatic event, and the spine can subsequently appear normal when evaluated radiographically.
spine regions, similar to adults (6). The large amount of cartilage in the pediatric cervical spine cushions direct vertical forces and limits the occurrence of bursting or compression-type fractures. The radiolucent cartilaginous component of the pediatric cervical spine, however, can make radiographic evaluation challenging. Children have more horizontal facet joints and increased ligamentous laxity, allowing for increased anterior and posterior motion of the cervical spine. This flexibility allows for significant spine distortion during the traumatic event, and the spine can subsequently appear normal when evaluated radiographically.
TABLE 24.1 High-Risk Mechanisms of Injury | |
|---|---|
|
Children have relatively large occiputs in comparison to their chest circumference, which leads to relative kyphosis of the neck in a supine position (7). Immobilization of an adult with a long spine board leaves his or her neck in a neutral (30-degree lordosis) position. A similarly immobilized young child, however, will have his or her neck forced into relative kyphosis (Fig. 24.1). By age 8, many of these differences have diminished, and the patient can be immobilized and evaluated as an adult.
Indications and Radiographic Evaluation
As described in the introduction, most pediatric cervical spine injuries are the result of high-force blunt trauma or specific mechanisms of injury like traction or axial loading. In children who are victims of these and many other types of trauma, prudence dictates cervical spine immobilization pending further evaluation. It should also be noted that, as compared with their adult counterparts, pediatric trauma victims can be difficult to evaluate. As is often the case with adult patients, the physician may be hampered by lack of patient cooperation and the absence of reliable witnesses, but young children present further problems because fear, pain, or lack of language skills may prevent them from relaying the symptoms (weakness, sensory changes) indicative of a cervical spine injury.
TABLE 24.2 Pediatric Cervical Spine Differences | |
|---|---|
|
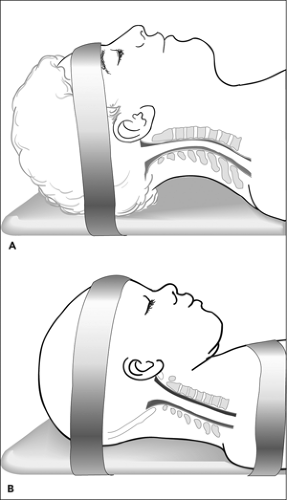 Figure 24.1 A. Adult’s neck in neutral position on spine board. B. Child’s neck in kyphotic position on spine board. |
Physical findings suggestive of cervical spine or cord injury include cervical pain (especially pain in the midline), traumatic torticollis, limitation of cervical motion, motor weakness, sensory changes, diaphragmatic breathing without retractions, hypotension without tachycardia, bowel or bladder dysfunction, and priapism (5). These patients may or may not have cervical spine immobilization in place on presentation to the emergency department (ED).
Full cervical spine immobilization (hard cervical collar, spine board, spacers, and straps) should be applied to any
patient with an unwitnessed or unclear mechanism of injury, a high-risk mechanism of injury, or a head injury involving loss of consciousness or altered mental status and whenever neurologic deficit or symptoms suggest a cervical cord injury. When the patient requires airway manipulation or intervention, in-line stabilization should be used. Although this can be accomplished from above or below the patient, immobilization from below may allow the airway to be managed in a less impeded manner.
patient with an unwitnessed or unclear mechanism of injury, a high-risk mechanism of injury, or a head injury involving loss of consciousness or altered mental status and whenever neurologic deficit or symptoms suggest a cervical cord injury. When the patient requires airway manipulation or intervention, in-line stabilization should be used. Although this can be accomplished from above or below the patient, immobilization from below may allow the airway to be managed in a less impeded manner.
Although cervical spine protection is important, immobilization should not delay airway assessment or intervention. Gentle airway maneuvers such as the jaw thrust, suctioning, and cricoid pressure can be performed without worsening an existing cervical injury. Vigorous airway maneuvers can, however, be detrimental to a patient with an unstable cervical spine (8).
Once a cervical spine injury has been diagnosed or is suspected, neurosurgical consultation may be necessary for further evaluation and definitive therapy. Transport of a patient with an unstable cervical spine over a long distance may require semipermanent immobilization (tongs, traction), and if the equipment and expertise does not exist at the referring hospital, a neurosurgeon may be included with the transport team.
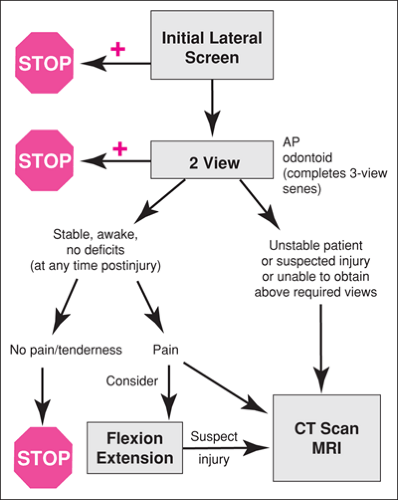
Radiographic options for cervical spine evaluation include routine radiographs, tomograms, computerized tomography (CT), and magnetic resonance imaging (MRI) (5,6) (Fig. 24.2). The most useful radiograph for cervical spine assessment is a lateral view, often performed at the bedside during trauma evaluation using portable equipment (9). This view should show any persistent dislocation or distraction but has an injury identification sensitivity of only 80% to 95%. The lateral cervical spine radiograph should be evaluated with regard to the alignment of the vertebral bodies, the integrity of the bones and cartilage, and the status of the soft tissues. The addition of at least two anterior views, C1-2 (odontoid view) and C3 through C7, increases the fracture identification sensitivity of the radiographic evaluation to 94% or greater (10). The odontoid view can be difficult to obtain on younger children (less than 5 years) and is not always done routinely in this age group (11). If a specific concern exists, a CT scan through C1 and C2 with reconstruction can replace the odontoid view (5). Oblique (pillar) views will provide further information about the posterior cervical column (pedicles, lamina, articulating and spinal processes) but rarely add significant information (12). Oblique views are potentially dangerous if performed with the standard 15-degree cranial angulation and neck rotation. CT scanning, when available, has replaced oblique views and tomograms if fractures are suspected on the initial radiographic film or series. Flexion and extension radiographs can be added for the awake patient who has a normal neurologic examination and three-view trauma series but for whom a persistent concern about possible column or ligamentous injury exists. Flexion and extension are performed by the patient, not by the radiology technician, and only to the point of mild discomfort. Clearly any initial radiographic evaluation should not involve neck motion if a cervical fracture is suspected. If an abnormality is identified, a search for other injuries that may not be contiguous is still necessary. Further radiographic views of an identified fracture, however, usually are not helpful in the acute evaluation. Importantly, cartilage fractures and ligamentous injuries will not be directly visible on the cervical radiograph. These might only be suspected if the patient presents with an abnormal neurologic examination or if radiographs demonstrate increased soft-tissue swelling.
A CT scan of the neck can be helpful to assess areas of the spine not adequately visualized with routine films, to delineate fractures suspected on radiographs, and to further elucidate an identified injury. A CT scan can be performed quickly and efficiently without neck motion. CT scans done properly can be reconstructed to avoid missing fractures in the horizontal plane.
MRI is useful acutely in the identification of spinal cord injury when neurologic deficits are present. MRI is excellent for the detection of blood accumulation (epidural hematoma), ligamentous injury, and cord damage. Although CT technology is still superior for fracture identification, newer technology has improved the MRI with regards to the identification of cortical bone injury (13). The difficulties associated with managing acutely ill patients during an MRI scan and the requirement that the patient not move during image acquisition limit its usefulness for acute injury evaluation. MRI has, however, been used in children with altered mental status to facilitate early removal of cervical immobilization (13,14).
The syndrome of spinal cord injury without radiographic abnormality (SCIWORA) is more common in children less than 8 years of age (2,15,16). When applied to a child’s spine, forces that would result in fracture or dislocation in an adult might not result in an abnormality on radiograph or CT scan because of the child’s ability to realign the flexible cervical spine. The patient may, however, have had significant neurologic compromise. SCIWORA was first identified before MRI, and many SCIWORA patients have identifiable injury with MRI (17). Any patient suspected of having SCIWORA should remain immobilized pending evaluation by a neurosurgeon and, if necessary, further imaging studies.
Medical personnel should consider exclusion of significant injury upon clinical grounds, so-called “clearing” of the cervical spine, without radiographs if the patient has not been involved in a high-risk mode of injury, is awake and alert, has normal mental status (i.e., has no head injury or shock and is not under the influence of drugs or alcohol), and has no other painful injuries that might mask perception or appreciation of neck pain. Additionally, the child must have no evidence of neck pain, no tenderness to palpation of the cervical spine, full range of motion of the neck, a normal neurologic examination (motor, sensory, mental status), and no history of transient neurologic symptoms (18,19) (Fig. 24.3). Older, verbal children (e.g., those at least 4 to 5 years old) are more easily evaluated because they should be able to have a meaningful conversation. The cervical spine should not be cleared, regardless of radiographic findings, in the patient with altered mental status. Only when the patient is alert and awake and demonstrates normal neurologic status in concert with normal radiographs should the cervical spine be cleared. If questions arise during the assessment of a child’s cervical spine, consultation with a radiologist or neurosurgeon may be helpful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree