Care of the Fetus
Alan H. Jobe
PRENATAL CARE
The goals of prenatal care are to assess pregnancy and fetal risks and to monitor the pregnancy to optimize the chances for a good outcome. Ideally, a pregnancy is planned, and counseling and health assessments can begin before the fetus is conceived. There are risk assessment tools for evaluating the mother’s family and medical history, previous pregnancy history, and the progress of this pregnancy.1 Currently, most women receive a level 1 fetal ultrasound before 20 weeks’ gestation to assess gestational age, screen the fetus for anomalies, determine placental position, and identify multiple births. A level 1 ultrasound obtained prior to 20 weeks is more accurate than the date of the last menstrual period to determine gestational age. The early screening ultrasound is not intended to identify more subtle structural abnormalities. If anomalies are noted, the woman will be referred for a complete ultrasound evaluation of the fetus using more sensitive equipment and expert evaluations. In the United States it is now unusual for infants to deliver with major skeletal, cardiac, or other internal organ structural anomalies that have not been identified prior to delivery. Common chromosome anomalies such as trisomy 21 also have structural signatures that can be identified by early gestational ultrasound. The genetic abnormality then can be verified by amniocentesis. An accurate early assessment of gestational age is the cornerstone for subsequent monitoring of the pregnancy and decisions about the timing of delivery.
ANTENATAL SCREENING AND TESTING
All women should have plasma tests to evaluate blood type and Coombs status. Women who are Rh negative are carefully followed and given anti-Rh antibodies for fetal loss and for pregnancy abnormalities that may be associated with bleeding. The maternal plasma also is tested for antibodies to syphilis, rubella, hepatitis B, and often human immunodeficiency virus (HIV), as these infectious diseases adversely affect the fetus. Women are routinely offered second-trimester antenatal screening for Down syndrome using 3 analytes in maternal plasma, called the triple screen.2 Women at high risk of having a fetus with Down syndrome will have low α-fetoprotein, high human chorionic gonadotrophin, and low unconjugated estriol levels, adjusted for gestational age. If the maternal plasma tests indicate increased risk, a level 2 ultrasound can identify structural findings frequently associated with Down syndrome: increased nuchal fold translucency, a hypoplastic fetal nasal bone, and a short length relative to head size, together with other findings. The diagnosis can be confirmed by karyotype of fetal cells from amniotic fluid. The risk of Down syndrome increases with maternal age, and a fetal chromosome assessment is recommended for pregnant women 35 years or older.
Maternal serum α-fetoprotein values also are used to screen pregnancies for neural tube defects. In contrast to Down syndrome, this protein is elevated with open neural tube defects as well as with abdominal wall defects such as omphalocele or gastroschisis. Specific genetic screening is offered to women on the basis of family history and racial background. These tests can be performed on the mother and father for rare autosomal recessive diseases (eg, Tay-Sachs disease) to establish fetal risk, with fetal diagnosis using cells recovered by amniocentesis. Cystic fibrosis screening also is offered to select populations. Information about the genetic status of a high-risk fetus is critical for families to make reproductive decisions. Fetal cells and DNA can be detected at very low levels in maternal blood. In the future, accurate fetal assessments may be possible without invasive procedures such as amniocentesis or chronic villous sampling.3
The more mundane but important aspects of prenatal care include monitoring maternal health throughout pregnancy. Prenatal nutritional supplements assure adequate vitamins, minerals, and iron to support fetal growth. Urine is routinely screened for protein and glucose, and blood pressure is monitored, as hypertension is associated with poor pregnancy outcomes. Maternal counseling about nutrition, drugs, alcohol, and tobacco avoidance are important components of prenatal care. Illegal drugs can adversely affect a pregnancy and should be avoided. Tobacco use is associated with decreased fetal weight, prematurity, and postnatal lung abnormalities. Alcohol use during pregnancy causes developmental brain abnormalities and fetal alcohol syndrome, reflected in the very high incidence of poor neurodevelopmental outcomes in populations with high alcohol use.4 Fetuses are frequently exposed to multiple nonprescription drugs, and while most of these exposures are of no known consequence, they are best avoided.
As gestation progresses, the monitoring of the pregnancy intensifies. The hormonal adaptations of pregnancy normally challenge maternal glucose metabolism. Women with diabetes prior to pregnancy are at increased risk of fetal anomalies and should attempt good glucose control prior to conception, which can decrease the risk of fetal anomalies.5 Pregnancy with diabetes requires close management to avoid fetal macrosomia and late gestational stillbirths. Women without diabetes can develop gestational diabetes during pregnancy. Women at high risk are older, obese, may have a family history of diabetes, and may have previously delivered a large-for-gestational-age infant. Women are tested during pregnancy for gestational diabetes using oral glucose tolerance tests. Gestational diabetes is not a benign condition because risks to the fetus are increased.
THE DELIVERY
As term gestation approaches, the expectant mother and her obstetrician must make decisions about the delivery. Planned vaginal births frequently now are prepared for by labor classes to educate the woman and her partner about the birth process and how she can optimize both the experience and the outcome. However, the frequency of normal term births following the spontaneous onset of labor is decreasing in Western societies for multiple reasons.6 In the United States, the frequency of deliveries at greater than 40 weeks’ gestation has decreased strikingly because of elective inductions of labor. Cesarean deliveries have increased as obstetricians have elected to avoid the risks of delivering infants in the breech position or the risks of using forceps and other operative vaginal deliveries. Many labors now result in cesarean deliveries for any abnormalities or delays in otherwise spontaneous deliveries. Although most women can successfully labor and deliver an infant after a prior cesarean section, there is an increased risk of uterine rupture. Most women who have had a cesarean section now have repeat cesarean sections for subsequent deliveries. Some women choose cesarean delivery when there is no medical indication for it. The net result is that more than 30% of deliveries in the United States are now by cesarean section, and the median gestational age of delivery has decreased by 1 week for the entire population.
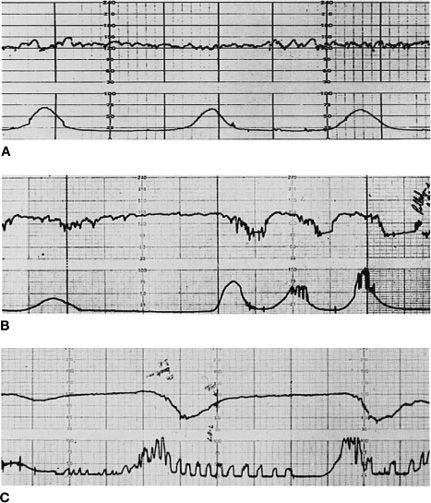
If there are concerns about a pregnancy, a variety of tests are used to evaluate fetal status. Fetal monitoring utilizes ultrasound technology to detect the fetal heart, fetal movements, fetal breathing, amniotic fluid volume, and uterine contractions.7 Fetal blood flow also can be monitored to assess placental resistance to flow. Some tests involve “stress” caused by an induced uterine contraction or stimulation of the fetus with an external sound source. The fetal heart rate pattern is used to assess fetal oxygenation status. The fetal heart rate normally is between 110 and 160 beats per minute with considerable beat-to-beat rate variability resulting from modulations of the fetal heart rate by the brain via the autonomic nervous system. A loss of variability may result from suppressed fetal central nervous system activity from hypoxemia and is a clinical indicator that the fetus may be at risk (Fig. 39-1). Decreased fetal movements also can identify fetuses at risk, as can decreased amniotic fluid volume. If uterine contractions are occurring, a fall in fetal heart rate after the onset of a contraction with a gradual return to baseline after the contraction has ceased (a late deceleration) suggests decreased fetal oxygenation. This oxygenation deficit results from the reduced placental perfusion that occurs with uterine contraction. Fetal heart rate decreases and increases not linked to contractions may indicate intermittent cord occlusions. Fetal assessments of heart rate prior to or concurrent with the onset of labor are evaluated within the context of the fetal gestational age, the estimate of fetal size, and other factors such as rupture of membranes. While fetal monitoring is not highly predictive of outcomes, some fetuses at high risk for a failed labor or birth depression can be identified. Fetal heart rate and uterine contraction monitoring are used routinely throughout labor to assess fetal status and the labor pattern. Labor monitoring is an imprecise tool for the identification of fetuses at risk for complications such as cerebral palsy and does result in increased cesarean section rates.
A spontaneous vaginal delivery is a natural human event. However, delivery is a relatively high-risk experience for both the mother and the fetus. Without medical management, both maternal and fetal death rates associated with spontaneous deliveries are high in the developing world. Adverse events such as postpartum hemorrhage or birth asphyxia can be anticipated in some cases on the basis of pregnancy history and labor progression, but adverse events are not always predictable or preventable. Labor and delivery remains an uncontrolled process.
COMPLICATIONS OF PREGNANCY
 PRETERM LABOR
PRETERM LABOR
Preterm labor is the onset of uterine contractions prior to 37 weeks’ gestation. Preterm deliveries are the major contributors to infant mortality. The rate of preterm delivery has increased despite intensive efforts to identify causes and develop treatments. The problem of prematurity includes multiple pathologies. Very early preterm deliveries prior to 28 weeks’ gestation are less than 1% of the deliveries but are the major association with infant mortality. Many of the deliveries are associated with both preterm premature rupture of membranes and chorioamnionitis, an inflammation of the fetal membranes and chord.8 These early deliveries seem to be associated with low-grade pathogens such as Ureaplasma or Mycoplasma. Later gestation preterms are frequently medically indicated because the women have preeclampsia, fetal growth restriction, or multiple births.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


