Cardiac Pacing
Kathleen P. Kelly
Michael Altieri
Dr. Michael Altieri passed away in January 2004. It has been a great loss to me and to pediatric emergency medicine. He and I originally wrote this chapter together, with Mike writing the entire beginning part of the chapter and me writing the second half. As his portion is essentially unaltered from the first edition, he remains an author of the chapter.
Introduction
Emergency cardiac pacing is rarely performed in children but in selected cases can prove life-saving. With the increasing prevalence of cardiac surgery among pediatric patients with congenital heart disease, the likelihood of encountering children with arrhythmias in the emergency department (ED) has increased. Emergency cardiac pacing enables the physician to initiate and sustain a cardiac rhythm that will provide perfusion of the vital organs in a patient with symptomatic bradyarrhythmia. Clinicians who care for critically ill infants and children should be familiar with the unique aspects of performing cardiac pacing for these patients. Two methods used in the emergency setting are the transvenous approach and the transcutaneous approach. Transvenous cardiac pacing involves placement of a pacing wire in direct contact with the myocardium via the central venous circulation. Transcutaneous pacing, which can be performed far more rapidly, utilizes electrodes incorporated into adhesive pads that are applied directly to the external chest wall. Although easier, this method yields less reliable results and is most commonly used as a temporizing measure until transvenous pacing can be performed. Emergency transvenous pacers are inserted by physicians in the ED, intensive care unit (ICU), or operating room. Transcutaneous pacers are technically easier to use and may be applied and operated by physicians, nurses, or paramedics.
The ability to electrically depolarize muscle was first noted over a century ago; however, it was not until 1952 that the clinical utility of cardiac pacing for humans was demonstrated by Zoll. Pacemaker technology advanced from the original devices, which consisted of wires passing through the skin into the myocardium, to a more modern endocardial transvenous pacer introduced in 1959 by Furman and Schwedel. The first implantable permanent pacemaker also was developed in 1959. With the creation of the balloon-tipped central venous catheter by Swann in 1970 came the flow-directed transvenous pacers used today. The most recent development in pacing technology is the transcutaneous pacer. Although the initial experiments with transcutaneous pacing actually predated transvenous pacing, this technique was all but abandoned because of the pain caused by severe muscle contractions. This problem now has been overcome primarily with the use of decreased delivered current, an electrode with a larger surface area, and an electrical impulse with a longer duration. Consequently, it is now feasible in many instances to perform cardiac pacing effectively without using an invasive procedure.
Anatomy and Physiology
Sites used for transvenous pacer insertion are the femoral, right internal jugular, and left subclavian veins (Fig. 22.1). In adolescents, the right internal jugular vein site and, if necessary, the left subclavian vein site may be used. Whenever possible, the right internal jugular access site should be used so that the left subclavian vein is preserved for possible long-term pacemaker placement. When inserted through the right internal jugular vein, the pacer wire has a more or less straight-in approach to the right atrium via the superior vena cava. Disadvantages of this approach include possible carotid artery puncture, dislodgment of the catheter with movement of the head, and an increase risk of thrombophlebitis of the internal jugular vein. When inserted through the left subclavian vein, the angle of entry into the superior vena cava is less
acute than is encountered with the right subclavian approach. The main disadvantage of subclavian placement is possible pneumothorax.
acute than is encountered with the right subclavian approach. The main disadvantage of subclavian placement is possible pneumothorax.
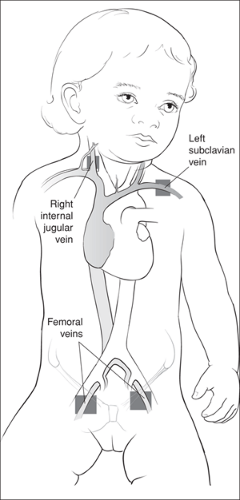 Figure 22.1 Preferred sites for transvenous pacemaker placement. (Note: the left subclavian vein site is recommended only for adolescents.) |
Because infants and younger children have a relatively short neck and a subclavian vein that is less accessible behind the clavicle, the femoral approach is preferred. Many clinicians use the femoral approach for all pediatric patients. The pacer wire passes along the length of the femoral vein into the inferior vena cava and ultimately enters the right atrium. The principle disadvantages of this route are an increased risk of thrombophlebitis, a higher incidence of infection, and restricted patient mobility because the catheter is easily dislodged with movement. In addition, the increased distance to the heart from a femoral access site often requires the use of fluoroscopic guidance in a child with poor cardiac output (i.e., when flow-directed catheters are less effective). An alternative approach is via the brachial vein, although this method is seldom used because of the smaller size of the vein and the relative difficulty of this technique. A cutdown is often necessary when using the brachial vein approach. The pacer wire passes along the brachial vein into the subclavian vein and finally through the inferior vena cava into the right atrium. Further discussion of these central venous access approaches is provided in Chapter 19.
Unlike transvenous pacing, transcutaneous pacing is easy to perform with pediatric patients and is often more effective for children than for adults. This is primarily because children have decreased density and thickness of the chest wall (ribs and muscle), which results in a lower transthoracic resistance, and a smaller chest diameter. Transcutaneous pacing can even be used with small children, as there are pediatric size electrodes as small as 6 × 7 cm.
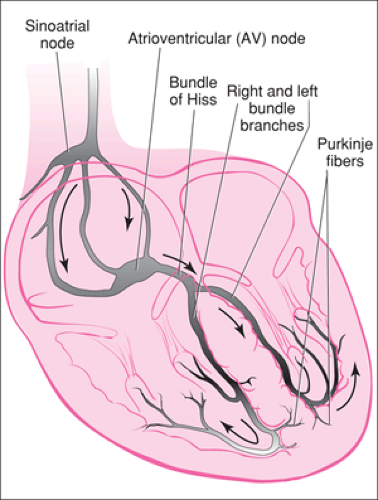
Before discussing the applications of cardiac pacing, it is useful to briefly review the conduction system of the heart (Fig. 22.2). Electrical activity is initiated by the sinoatrial
node, located at the junction of the superior vena cava and the right atrium. The stimulus is then spread throughout the atria and terminates at the atrioventricular (AV) node in the lower part of the right atrium. From there, the electrical impulse is conducted through the bundle of His, which divides to form the right and left bundle branches of the ventricles. The bundle branches further divide into the Purkinje fibers, which penetrate the myocardium, allowing rapid conduction of the impulse throughout the ventricles, with resulting contraction.
node, located at the junction of the superior vena cava and the right atrium. The stimulus is then spread throughout the atria and terminates at the atrioventricular (AV) node in the lower part of the right atrium. From there, the electrical impulse is conducted through the bundle of His, which divides to form the right and left bundle branches of the ventricles. The bundle branches further divide into the Purkinje fibers, which penetrate the myocardium, allowing rapid conduction of the impulse throughout the ventricles, with resulting contraction.
Most life-threatening arrhythmias in children are bradyarrhythmias. Asystole is also a common terminal rhythm in children, although not amenable to pacing. For infants and younger children, cardiac output directly depends on heart rate, and therefore bradyarrhythmias produce a fall in cardiac output and resulting circulatory compromise. Sinus bradycardia (a rate less than 60 bpm) resulting from a primary cardiac abnormality is relatively uncommon in the pediatric age group and generally indicates markedly increased vagal tone. Failure of impulse formation or transmission from the sinus node is referred to as “sinoatrial block” and may manifest as a nodal rhythm. Complete AV block is usually a congenital condition but can also be seen with digitalis intoxication and rheumatic carditis.
Indications
Conditions that lead to arrhythmias that require cardiac pacing are relatively uncommon in children. Consequently, this procedure will be indicated only in rare instances. However, in those circumstances where cardiac pacing is necessary, the procedure can be life-saving. In general, the indications for cardiac pacing can be divided into two categories: urgent and emergent. Situations requiring urgent cardiac pacing are those in which a child has a persistent arrhythmia that is refractory to drug therapy. Although minor associated symptoms may exist (e.g., mild dizziness, orthostasis), the cardiovascular status of the patient is otherwise stable. Potential arrhythmias include supraventricular tachycardia (SVT), which may require overdrive pacing in the ICU, or stable AV dissociation, which may require eventual surgical implantation of a permanent pacemaker. For these patients, transcutaneous pacing should be available in the ED, but transvenous pacing is generally unnecessary as part of the initial management. If transvenous pacing proves to be necessary, this procedure can normally be performed on a semi-elective basis in the radiology suite with the aid of fluoroscopic guidance, because any clinical deterioration in the patient is typically gradual. In such cases, echocardiography is an alternative means of visualizing placement of the pacer wire.
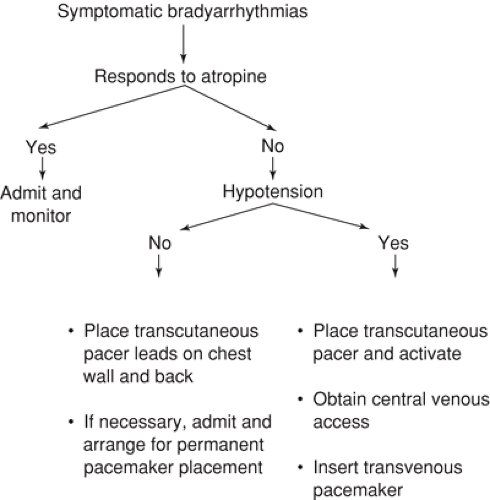
Emergent cardiac pacing is the procedure that will be indicated for children in the ED. These patients have significant hypotension associated with a refractory bradyarrhythmia, most commonly AV dissociation. Transcutaneous pacing can be attempted in such cases, but because the presenting rhythms are often difficult to abort, this should occur while the equipment required for transvenous pacing is being assembled and appropriate central venous access is obtained. An algorithm showing the indications for cardiac pacing is presented in Figure 22.3.
The young child with a significant bradyarrhythmia typically shows signs of poor perfusion. The patient may be pale and/or mottled. The extremities are often cool and cyanotic, and capillary refill time may be prolonged. Urine output is decreased or absent, and the child will often be lethargic or, in more extreme cases, unconscious.
Congenital heart defects are associated with a variety of clinically significant arrhythmias, including the bradyasystolic rhythms. Such defects include Ebstein anomaly, transposition of the great vessels, and congenital mitral stenosis. Among neonates, congenital complete heart block is associated with maternal systemic lupus erythematosus. Pediatric patients who have undergone cardiac surgery for repair of a congenital anomaly (e.g., tetralogy of Fallot, atrial and ventricular septal defects, endocardial cushion defects) are also at risk for arrhythmias. Additionally, acquired processes may be associated with an increased incidence of bradyarrhythmias, such as rheumatic heart disease, myocarditis, cardiac tumors, and certain metabolic and electrolyte disturbances.
In general, infants and younger children requiring emergent transvenous pacing should have the wire inserted via a catheter in the femoral vein, using fluoroscopic guidance as indicated. Older children and adolescents may be managed similarly to the adult patient, using the right internal jugular vein or subclavian vein. Although the left subclavian vein provides a more reliable approach for insertion of a transvenous pacer, it should only be used when absolutely necessary, because the left subclavian is also the preferred site for a permanent pacemaker. A balloon-tipped flexible catheter should be used to avoid cardiac perforation. A rigid wire is indicated only in an arrest
state with no significant blood flow. Because children rarely suffer a full bradycardic arrest purely on the basis of cardiac dysfunction, using a rigid wire will seldom be appropriate for this patient population.
state with no significant blood flow. Because children rarely suffer a full bradycardic arrest purely on the basis of cardiac dysfunction, using a rigid wire will seldom be appropriate for this patient population.
Transcutaneous Pacing
Equipment
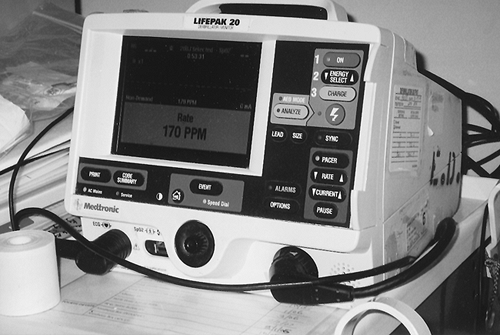
The equipment for transcutaneous pacing comprises the pacing unit, electrodes, cardiac monitor, and defibrillator. Several transcutaneous pacing models are available that perform only pacing (e.g., Zoll, NTP, ZMI Corp., Cambridge, MA). However, many practitioners prefer to use a unit that combines external pacing with cardiac monitoring and defibrillator capabilities (e.g., Lifepak 20, Medtronic Physio-Control, Redmond, WA) (Fig. 22.4). These units are equipped with digital display and buttons to control the delivered current and to select either demand or asynchronous modes. The Lifepak 20 has a variable rate control ranging from 40 to 170 bpm. This is an improvement for use in children over earlier models, which had maximum rates of 90 bpm.
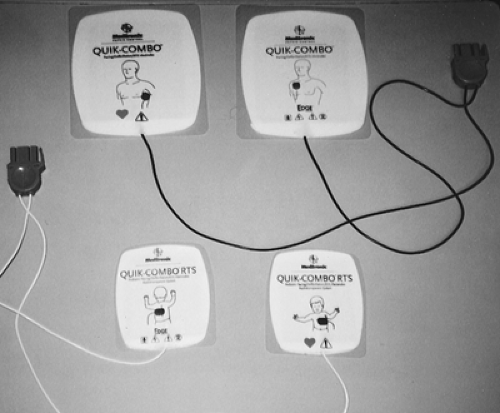
The electrodes for transcutaneous pacing are now available in adult and pediatric sizes (Fig. 22.5). They are silver/silver chloride pads measuring 13 × 15 cm for older children and adults and 6 × 7 cm for smaller children and infants. The electrodes have been shown to be safe for both the patient and medical personnel. Clinicians can perform CPR with their hands directly over them if necessary.
Procedure
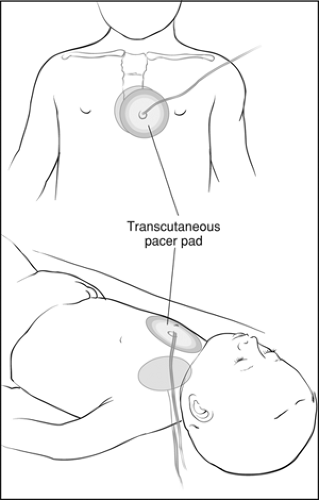
Transcutaneous pacing electrodes are easily applied to the anterior and posterior chest walls with the adhesive. The normal location of the V3 lead of the ECG is an ideal anterior position, while the posterior lead should be placed on the upper back between the scapulae (Fig. 22.6). If capture does not occur in these positions, the posterior lead can be moved to
a more lateral or even axillary location. If possible, the leads should not be placed over bony structures such as a scapula.
a more lateral or even axillary location. If possible, the leads should not be placed over bony structures such as a scapula.
Sedate patient as indicated.
Apply adhesive electrodes to anterior and posterior chest walls.
Connect patient to monitoring system of pacing module.
Set rate just above patient’s rate.
Set system on demand mode if patient has an intermittently acceptable intrinsic rate; otherwise set system on asynchronous mode.
Set output to lowest value.
Turn on pacer.
Gradually increase output until capture is noted.
Set output just above pacer threshold.
Set rate to minimum desired rate.
Make plans for transvenous pacing.
The patient should be monitored using the cardiac-monitoring capabilities of the transcutaneous pacer. In general, pediatric patients should be sedated before transcutaneous pacing (see Chapter 33). The rate should be set appropriately based on the age of the child. Assuming there is an intrinsic rate, the pacemaker is set on demand mode so that pacing will occur only when the patient’s own ventricular rate is inadequate. The monitor is turned on with the output at the lowest level, and the output is gradually increased until capture is obtained. The rate is then set to a minimum acceptable heart rate for the patient, and the output is set just above the pacing threshold. At this point, immediate plans should be made for transvenous pacing as needed on an urgent (stable patient) or emergent (unstable patient) basis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree