2St John’s Hospital, Livingston, UK
3Canniesburn Hospital, Glasgow, UK
Overview
- Breast reconstruction should be offered to the majority of patients undergoing mastectomy
- There are a wide range of options for breast reconstruction, including using implants alone, myocutaneous flaps alone or the two together
- Surgeons performing breast reconstruction need specific training
- Patients who smoke or who have had radiotherapy are at high risk of complications from breast reconstruction
- Patients who have had breast-conserving surgery and have a poor cosmetic outcome can be offered partial breast reconstruction to improve results
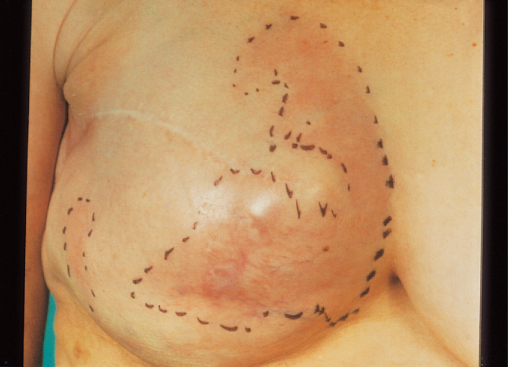
The purpose of the operation is to reconstruct a breast mound that matches the opposite breast in size, shape, position and contour to produce breast symmetry (Figure 17.1). Demand for reconstructive surgery has increased consistently, and up to half of patients offered immediate breast reconstruction choose to have it. No evidence shows that immediate reconstruction increases the rate of local or systemic relapse or that it makes relapse more difficult to detect. Breast reconstruction reduces the psychological trauma experienced by patients after mastectomy. Breast reconstruction (particularly immediate reconstruction, which gives substantially better cosmetic and psychological outcomes) should therefore be widely available.
Figure 17.1 Skin-sparing mastectomy in a patient who developed recurrence after breast-conserving surgery and radiotherapy (tattooing marks show the area treated). The breast was reconstructed with an extended latissimus dorsi flap with a small implant.

Treatment Options (Table 17.1)
Table 17.1 Options for breast reconstruction: Patient factors.
| Technique | Indications for | |
| Immediate reconstruction | Delayed reconstruction | |
| Prosthesis | Small breasts Adequate skin flaps | As for immediate reconstruction plus well healed scar plus no radiotherapy** |
| Tissue expansion and prosthesis | Adequate skin flaps Tension free skin closure Small to medium-sized breasts | As for immediate reconstruction plus well healed scar plus no radiotherapy** |
| Myocutaneous flaps | Large skin incision Doubtful skin closure Large breasts | As for immediate reconstruction Can be used if previous radiotherapy |
*Unless using acellular dermal matrix.
**Radiotherapy significantly increases complication rates.
The choice of operation for an individual patient depends on several factors. Immediate breast reconstruction is less time consuming for the patient (although not for the surgeon), but care must be taken that the oncological operation is not compromised for a better cosmetic result. Reconstruction can be carried out by immediate placement of a prosthesis (implant), but this gave poor results in the majority prior to the introduction of dermal matrix. Other options include insertion of a tissue expander or insertion of a flap of skin and subcutaneous fat with or without muscle (myocutaneous or fasciocutaneous flap) with or without prosthesis.
Implants and expanders are usually inserted under the muscles of the chest wall (the pectoralis major and parts of the serratus anterior, rectus abdominis and external oblique); the expander is inflated over several months to stretch the skin and muscle and is eventually replaced with a definitive breast prosthesis. This technique involves no additional scars. The long-term results of implant-based breast reconstruction depend on the tolerance of skin and chest wall muscle and the need for adjuvant radiotherapy. Although at first glance this might seem a simple and quick operation, this type of reconstruction is associated with a high rate of reoperation over time and in the majority the need for symmetry surgery to the contralateral breast.
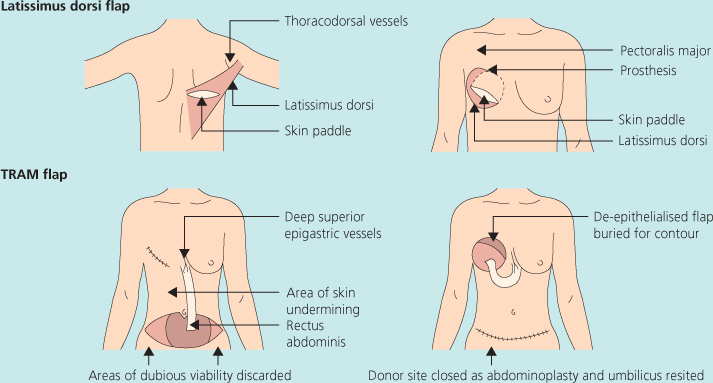
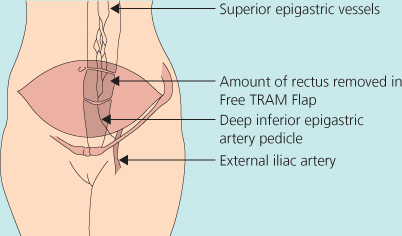
The two most common myocutaneous flaps used require movement of the latissimus dorsi muscle (with or without overlying skin) (Figure 17.1) or the lower abdominal fat and skin based on the rectus abdominus muscle (transverse rectus abdominus myocutaneous (TRAM) flap) (Figures 17.2 and 17.3). They allow for simultaneous replacement of skin and soft tissue and allow for the creation of larger and more pendulous breasts. All flap reconstructions leave scars at the donor site on the back or the lower abdomen respectively. Latissimus dorsi flaps often require a breast implant to be placed between them and the chest wall to create a breast mound, although by extending the flap to include overlying fat it is often possible to get sufficient bulk to reconstruct the whole breast without using a prosthesis. Transverse rectus abdominus myocutaneous (TRAM) flaps can be performed as a pedicled flap based on the superior epigastric artery or as a free flap based on the inferior epigastric vessels (Figure 17.3) with a microvascular anastomosis. Muscle sparing perforator flaps such as the Deep Inferior Epigastric Perforator (DIEP) or the Superficial Inferior Epigastric (SIEA) flaps harvest the same amount of lower abdominal tissue but protect the rectus abdominis musculature and preserve abdominal wall function. These flaps are bulkier and do not usually need an implant to be inserted.
All of the above reconstructions can give pleasing results in correctly selected patients when performed by experienced surgeons. All forms of breast reconstruction are substantial surgical operations, and preoperative counselling is essential.
Tissue Expansion and Prostheses
Silicone implants are currently licensed in the United Kingdom and United States for breast reconstructions. The newer silicone implants are ‘solid’ gel implants and come in a variety of shapes and sizes; these are not liquid at body temperature, should have a longer lifespan and should leak less silicone than liquid silicone implants. Saline prostheses are also available, but they do not have the same doughy consistency of silicone gel and breast tissue. Prostheses can occasionally provide satisfactory results if inserted immediately at the time of operation or as a delayed procedure in patients with small breasts who have adequate skin flaps.
The use of tissue expanders and implants has increased since the availability of human and porcine acellular dermal matrices. These are decellularised human (Alloderm®) or porcine
(Strattice®) dermis. They are sutured between the inframammary fold below and the cut edge of the divided pectoralis muscle above and act as a sling to accommodate an expander or implant (Figures 17.4 and 17.5). Acellular Dermal matrices provide additional soft tissue cover to the lower pole of the breast and this may avoid dissection of the serratus anterior muscles and the rectus sheath (Figure 17.4(a)). Most prostheses, however, are inserted after a period of tissue expansion (Figure 17.6), particularly in delayed breast reconstructions or if the patient desires a larger bust size and a concomitant augmentarion of the contralateral breast. Tissue expansion involves the placement of a silicone bag with an external filler port, or an integral filling valve. Saline is injected into the filler port at weekly visits (Figure 17.7). The increasing volume in the expander leads to gradual stretching of the overlying skin and recruitment of skin from the adjacent chest wall to cover the reconstructed breast. The expander is eventually removed and replaced with a permanent silicone implant (Figure 17.8). Double lumen expanders are prostheses that consist of an outer compartment filled with silicone for a natural feel and an inner compartment that can be inflated with saline. These devices do not need to be replaced with permanent implants (Figure 17.9). Once the desired volume is obtained, the filler port can be removed and the expander or prosthesis is left in situ. Tissue expansion is associated with discomfort of the chest wall and ribs, and the chest wall can be substantially depressed immediately under the expander. Textured tissue expanders seem to produce less chest wall distortion and less discomfort. This technique is likely to give better symmetry in bilateral cases or in patients who desire a concomitant augmentation of the contralateral breast.
Figure 17.4 Patient who had a previous mastectomy on the right and subsequently had a left subcutaneous mastectomy and bilateral implant based breast reconstruction with Strattice®.

Figure 17.5 (a) Strattice being inserted (b) Lateral view of the subcutaneous mastectomy shown in Figure 17.4.
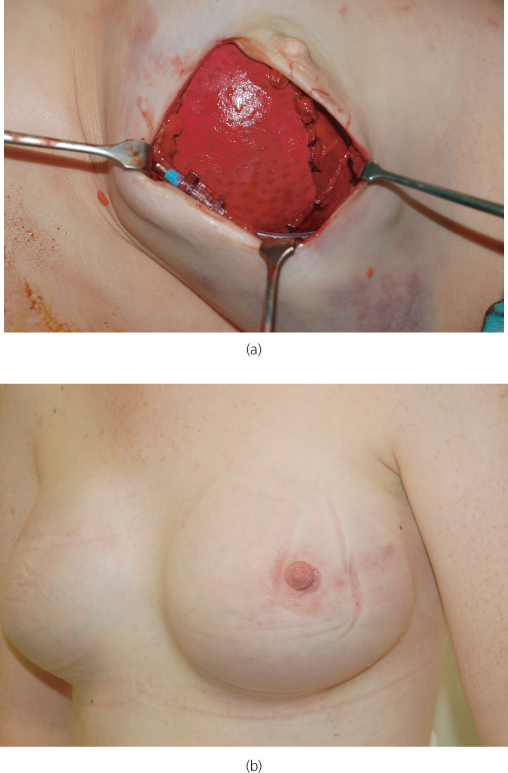
Figure 17.7 Textured tissue expander used for breast reconstruction which has an integral filler port that is located by a magnet as shown.
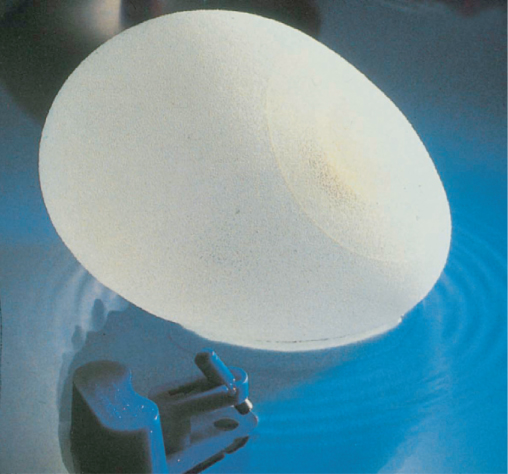
Figure 17.8 Patient who had bilateral reconstruction with tissue expanders replaced by implants and subsequent nipple reconstructions and tattooing.

Figure 17.9 Patient who had a left mastectomy with removal of nipple, but areola was left intact and right prophylactic mastectomy was reconstructed with bilateral Becker expander/prosthesis. Injection ports can be seen in situ below and lateral to prostheses.

It is difficult to create large breast mounds by tissue expansion. If this technique is to be used in a patient with large or very pendulous breasts, the possibility of reducing the contralateral breast should be considered and discussed with the patient (Figure 17.10). Further surgery to the contralateral breast may be required in future because implant based reconstructions do not mature and droop like autologous breast reconstructions over time.
Figure 17.10 Patient with left breast reconstruction by tissue expansion and prosthesis; she subsequently had her right breast reduced to achieve symmetry.

Complications with Breast Prostheses: Capsular Contracture
The most common complication after the use of prostheses is the formation and subsequent contraction of fibrous capsules around implants. The use of textured prostheses has reduced the incidence of capsular contracture from 50% with smooth implants at one year to 10% at 10 years with textured implants. Capsular contracture results in hardening, distortion, an inferior cosmetic appearance of the reconstructed breast mound, and often discomfort and embarrassment. Postoperative radiotherapy substantially increases the rate of capsular contracture. Possible treatments include capsulotomy or capsulectomy, with change of prosthesis to a textured implant if a smooth implant was used. Recent evidence suggests that fat grafting or lipomodelling around the capsule of the implant may improve capsular contracture. Closed capsulotomy (forced manual rupture of the fibrous capsule) is not an appropriate treatment. Recurrent capsular contracture may eventually require removal or replacement of the implant with autologous tissue.
Infection occurs in less than 5% of patients and results in the prosthesis having to be removed (Figure 17.11). Most units use prophylactic antibiotics to limit the rate of infection. Low-grade infection can occasionally manifest as early capsular contracture or erosion of the prosthesis through the overlying skin (Figure 17.12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree