Fig. 6.1
(a) Radiograph of a 7-year-old girl with Blount’s disease. Apex of the deformity is seen at the intersection of the two lines (red lines indicate the proximal and distal tibial mechanical axes). (b) Overcorrection by Rab’s osteotomy. (c) Radiograph at 3-year follow-up shows good alignment of the mechanical axis of the tibia
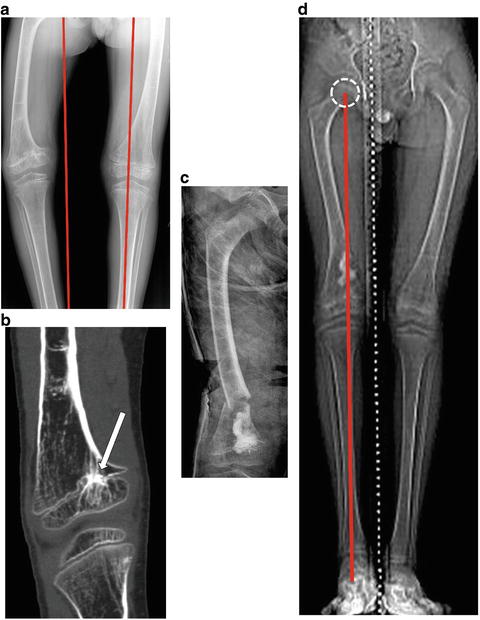
Fig. 6.2
(a) Right-sided genu varum in a 7-year-old boy with hemi-epiphyseal arrest of the right distal femur (red lines represent the mechanical axes of both lower limbs). (b) CT scan shows a peripheral physeal bar (white arrow). (c) Bar resection and cement interposition were performed in addition to corrective osteotomy of distal femur. (d) CT scanogram (supine) shows restoration of the mechanical axis and proximal migration of cement indicating restoration of growth at 18-month follow-up. A supine CT scanogram was taken in this case; however, a standing full-length radiograph is a more accurate measure of alignment and should be preferred
Principles Pertaining to Correction of Lower Limb Alignment
Minor changes in lower limb alignment following corrective osteotomy often remodel in children. Bone remodelling following correction occurs in both sagittal and coronal planes, although such remodelling is greater in the plane of joint movement and when the osteotomy is close to the growing end of the bone. This remodelling occurs at the site of osteotomy in accordance with Wolff’s law [5]. This law infers that remodelling will occur on the compression side by laying new bone. Pauwels postulated that malalignment of bone produces a differential growth at the physis which tends to realign the shaft perpendicular to the major joint reaction forces [6]. This observation is similar to the epiphyseal pressure rule of Heuter-Volkmann (growth is retarded by increased mechanical compression] [7]. Any residual deformity would tend to decrease by remodelling in 4–5 years following surgery [8]. Seventy-five percent of this remodelling occurs at the physis and 25 % by bone drift or translation [9, 10]. Thus a perfect anatomical alignment may not be necessary; however long-term follow-up is required in children with growth remaining.
Influence of Level of Osteotomy
In children, often the osteotomies are at a site distant from the apex or center of rotation of angulation (CORA). When planning an osteotomy, one should consider various factors such as the proximity of the CORA to the adjacent physis and/or joint, presence of pathological bone and neurovascular structures in the vicinity. Overall, metaphyseal osteotomies have a better healing potential than diaphyseal ones. The ease of rotational correction is the same at both levels in case of femur, but the proximal shaft is preferable as large corrections at the distal third would be theoretically at the expense of an undesirable alteration in the patella-femoral dynamics [11]. Any corrective osteotomy or lengthening should not be performed at the site of pathological bone to avoid healing problems [12, 13]. The exceptions are where the entire bone is pathologic like in osteogenesis imperfecta or fibrous dysplasia.
Adjuvant Fibular Osteotomy: When and Where?
The fibula acts as a strut to prevent large angular or rotational corrections of the tibia. Thus, with opening wedge correction of the tibia, an adjuvant fibular osteotomy is often performed along with tibial osteotomy.
Fibular osteotomy should be avoided in its proximal third to safeguard the common peroneal nerve [14]. In the middle third there is a risk of damage to peroneal vessels [15–17].
Classic recommendation of doing a distal tibial de-rotation without a fibula osteotomy is for rotational corrections of up to 35° [18]. However, de-rotational osteotomies of up to 55° internal and 45° external have been reported without fibular osteotomy and without neurovascular compromise [19]. We however prefer a fibular osteotomy while doing a rotational correction of greater than 30°.
We tend to perform osteotomy at the proximal and middle third junction in case of proximal tibial angular osteotomy and close to distal and middle third junction in distal tibial/rotational osteotomies.
A segment of the fibula should be resected when the desired angular correction in tibia is considerable [20]. Fibula osteotomy, if performed at a site far away from CORA, leads to wide displacement of the fibula and in such situation may require resection of the projecting portion of fibula. A distal tibio-fibular fusion should be performed to avoid ankle instability when a fibular pseudarthrosis is anticipated following such resections [21].
At least 10 % of the total fibular length should be preserved distal to the osteotomy to avoid ankle instability [22]. Our experience shows that proximal fibular migration occurs if the fibula does not unite, irrespective of the level of osteotomy.
Principles Pertaining to Specific Osteotomies
Opening Wedge Osteotomy
The axis of deformity correction lies on the convex cortex. The overall length of the limb increases following deformity correction. The final length achieved will be equal to the sum of the lengths of the convex border of the deformity (Fig. 6.3a). If the combined total correction exceeds 2.5–3 cm of lengthening, shortening may be required as a cautionary measure since significant lengthening could compromise the neurovascular status. The nerve stretch in certain circumstances may be further influenced by the direction of rotation such as the risk of iatrogenic injury being somewhat less in external than internal rotation when performing a proximal tibial osteotomy because of tethering of the peroneal nerve at the proximal fibula [23]. When the axis of correction lies away from the osteotomy site further lengthening is achieved; for instance in calcaneal lengthening osteotomy the axis of correction lies away from the calcaneum, i.e. at the talar head [24] (Fig. 6.4).
Fig. 6.3
(a) Open wedge osteotomy in a deformed bone of length “l” showing increase in length of the bone. The final length “L” is the sum of convex borders of the deformed bone. (b) Closed wedge osteotomy in an angular deformed bone showing increase in length of the bone. The final length “L” is the sum of concave borders of the deformed bone (ACA axis of correction of angulation). (c) In a straight bone an open wedge angular osteotomy causes less shortening than a closed wedge as shown by the red lines. Hence, the former is preferred when minimal lengthening is desired along with corrective osteotomy
Fig. 6.4
(a) Axis of correction of angulation (ACA) is located away from the calcaneum, i.e. at the talar head. The effective lengthening along with open wedge osteotomy can be seen. (b) Preoperative and (c) intraoperative radiographic views of left calcaneal lengthening osteotomy and the increase in talar head coverage brought about by it
Closing Wedge Osteotomy
The axis of deformity correction lies on the concave side of the deformity. The overall length of the limb increases following deformity correction and is equal to the sum of the concave borders of the deformity as shown in Fig. 6.3b. Generally, a closed wedge osteotomy in a straight bone reduces the limb length whereas the bone length increases or remains the same with an open wedge osteotomy, for instance with compensatory osteotomies for the proximal femur in Perthes disease and non-union of the neck of femur (Fig. 6.3c).
Dome Osteotomy
Dome osteotomy is ideal for deformities with CORA close to the joint line such as in physeal or metaphyseal injuries near the knee or ankle. The displacement of the osteotomy is directly proportional to the radius of correction. Dome osteotomy causes minimal length alteration as the CORA is usually at or near the site of deformity in the metaphysis. The advantage of such an osteotomy is good bony contact and intrinsic stability. However this technique is limited by its inability to correct rotational malalignment.
Angular Correction and Translation
An angular osteotomy involves shifting of mechanical axis in the direction of correction of the deformity; that is, the mechanical axis shifts medially in varus and laterally in valgus osteotomy. Hence translation of the distal fragment has been advised in order to restore the mechanical axis [23]. A valgus proximal femoral osteotomy requires lateralisation of the distal fragment. However when doing an angular correction below the knee the direction of translation is opposite, i.e. lateral translation for varus and medial translation for a valgus osteotomy. Glard et al. showed that proximal femoral varus osteotomy with medial translation in Perthes disease did not affect the mechanical axis deviation at the knee [25]. There are a number of studies which show remodelling of the femoral neck-shaft angle following varus osteotomy with or without translation [25–30]. In a child, do we need to translate the distal fragment when performing angular correction to optimise the mechanical axis? Sanghavi et al. found that after varus de-rotation osteotomy, the neck-shaft angle tends to revert to normal depending on the age at which the operation was undertaken [26]. Tercier et al. showed that following proximal femoral osteotomy in Perthes, the resulting mechanical axis deviation is usually subtle and clinically insignificant in children [27]. Following varus osteotomy of the proximal femur in cerebral palsy 60 % of the correction is lost after 8 years by remodelling [28]. In pelvic support osteotomy it has been shown that up to 30° of valgus angulation at the osteotomy site does not cause any significant change in mechanical axis [31]. Therefore it is our assumption that translation of the distal fragment during angular correction of proximal femoral deformities is not mandatory in younger children unless the magnitude of correction is outsized, such as greater than 30°. This observation is also supported by the acceptability of overriding/bayoneting fracture reduction in younger children where after a few years complete restoration of the anatomy occurs [32]. The advantages of not translating are that the periosteal hinge medial or lateral stays intact and the final lengthening achieved is greater than with translation (Fig. 6.5).
Fig. 6.5
(a) Effect of angular correction on length of a straight bone. Red solid lines indicate length of the straight bone. Increase in length is seen following opening wedge osteotomy without translation. Translation has relatively less effect on the final limb length. “S” is the amount of shortening effected following translation. ACA axis of correction of angulation. (b) Top: Radiograph of a child with Perthes disease of the right hip. Bottom: A varus de-rotation osteotomy was performed. The medial intact periosteal hinge is shown (white arrow)
Oblique Osteotomy
An oblique osteotomy corrects multi-planar deformities at the same time. A meticulous preoperative planning is essential as it involves correction of the deformity in various planes through a single osteotomy. Lesser the obliquity of the plane, lesser is the bony contact after angular correction but easier and greater is the rotational correction such as in Rab’s osteotomy (Fig. 6.6).
Fig. 6.6
In this example the amount of desired external rotational (20°) and valgus angular correction (40°) (indicated by dotted lines) is plotted on the graph. θ, the angle of inclination of proximal tibial osteotomy with the horizontal lies between 60 and 65°. Adapted from [74]
Lengthening/Shortening Osteotomy
Lengthening osteotomy in a single stage is best achieved either by a step cut/long oblique osteotomy to maintain adequate contact while lengthening at the same time such as in distal fibula, metatarsals or proximal ulna. Acute lengthening of 1.7 cm and 3.2 cm for the tibia and femur, respectively, has been performed with minimal complications in adults [33]. Opening wedge angular correction can some time offset the shortening caused by varus angulation and gain in length to some extent, for instance in Perthes disease (see Fig. 6.4a). It is important to keep in mind the change in length ratio as compared to the companion bones in case of osteotomies of leg and foot [34]. Acute shortening of up to 3 cm can be performed safely in young adults with open tibial fractures with bone loss [35]. Further shortening should be gauged based on the clinical assessment of limb vascularity. Fibular shortening osteotomy can be combined with proximal tibia corrective osteotomy in achondroplasia to correct the lateral collateral laxity and fibular overriding [36]. The major disadvantage of lengthening/shortening osteotomy with acute correction is that the amount of correction safely gained is limited. If the magnitude of angular deformity correction is considerable, either a shortening osteotomy or distraction osteogenesis is preferred to avoid significant risk to the neurovascular structures and soft-tissue tightness (Fig. 6.7).
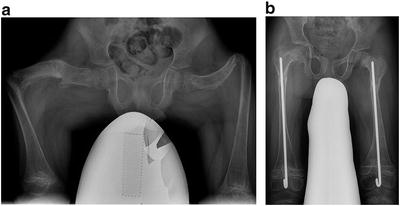
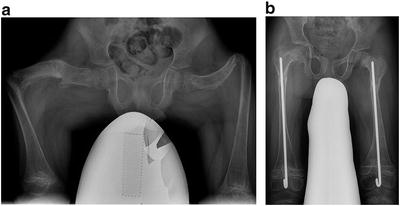
Fig. 6.7
(a) Radiograph of a 10-year-old girl with osteogenesis imperfecta and bowing deformity of both femora. Restoring the length of the femur is limited by the stretch on neurovascular structures and soft tissues. (b) Hence, corrective osteotomies are combined with shortening
Special Considerations
Deformity Secondary to Physeal Injury
Angular deformity secondary to physeal insult is usually progressive until skeletal maturity. The following strategies can be adopted for such corrections:
Overcorrection of the deformity to compensate for future progression of deformity.
Combination of acute corrective osteotomy and excision of physeal bar and interposition.
Acute corrective osteotomy combined with a growth modulation technique: This would however invoke a shortening effect due to arrest of either side of the physis.
An opening wedge osteotomy would simultaneously address the existing limb length discrepancy.
Mango Slice Effect
In the Indian subcontinent, raw mango slice, a savoury seasonal snack for children, is split into multiple radial cuts for better seasoning. This makes a good illustration for osteotomy with multiple open wedges for diaphyseal deformity as seen following rickets and other metabolic disorders. The concept and execution are explained in the following illustration. Small corrections at two or more CORAs allow lengthening and deformity correction spread over the length of bone (Fig. 6.8).
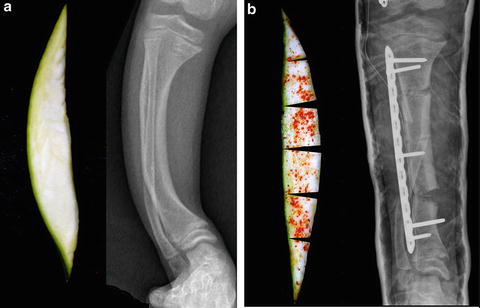
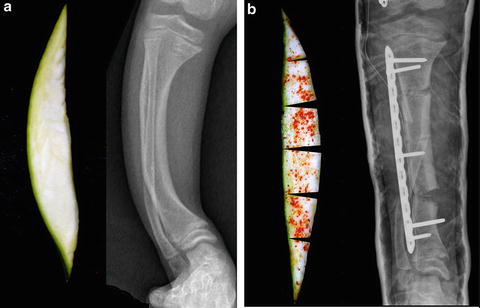
Fig. 6.8
(a) An intact mango slice and (b) a slit, seasoned one can be compared with multiple opening wedge osteotomies in a bowed tibia
The Deformity Memory Effect
Paediatric congenital and developmental conditions such as developmental coxa vara, fibular hemimelia and posteromedial bowing of tibia have a memory because of associated soft-tissue contractures. Following an osteotomy, either the deformity can recur by bending the callus or slow relapse occurs due to abnormal forces on the growing physis [Heuter-Volkmann]. In these situations the osteotomies should be combined with soft-tissue lengthening or shortening of the bone (Fig. 6.9).
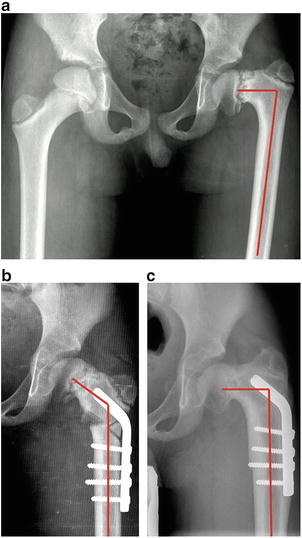
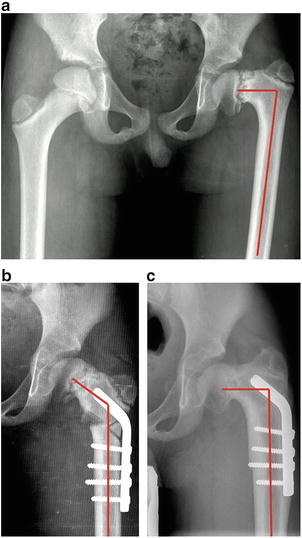
Fig. 6.9
The deformity memory effect. (a) Developmental coxa vara in a 15-year-old boy. (b) Corrective osteotomy and blade plate fixation. (c) Radiograph at 16-month post-op follow-up shows reduction of neck-shaft angle (red angles) in spite of the implant position remaining unchanged
Cozen’s Phenomenon
Certain fractures of the proximal tibia in a growing child are associated with a proximal tibial valgus deformity. These deformities may correct spontaneously over a few years, and thus an acute corrective surgery for the tibial valgus should be deferred for at least 3–4 years following the fracture [37, 38] (Fig. 6.10).


Fig. 6.10
Cozen’s phenomenon. (a) Three-year-old boy with proximal tibia fracture. (b) Radiograph after 4 years shows tibial valgus deformity
Box 6.1
Acute deformity is preferred in children and when the magnitude of deformity or length discrepancy is relatively small.
Soft-tissue constraints should be addressed simultaneously where needed, to avoid recurrence.
Knowledge of the natural history of the underlying pathology is crucial before executing an acute osteotomy.
Anatomical alignment of mechanical axis is not mandatory in younger children because of remodelling potential.
A dome osteotomy can be performed when the CORA is juxta-articular.
Fibular osteotomy may be necessary for tibial osteotomies for large correction.
Indications
The indications for acute correction with an osteotomy in children are varied and include correction of certain uniplanar or multi-planar skeletal deformities. The indications include angular and rotational correction as well as treatment of mild length discrepancies.
Site-Specific Osteotomies
Metaphysis
Frontal plane angular deformities around the knee [genu varum or genu valgum] related to conditions such as Blount’s disease, metabolic bone disease, physeal arrests and coxa vara are often treated with acute correction via a metaphyseal osteotomy (Fig. 6.11).
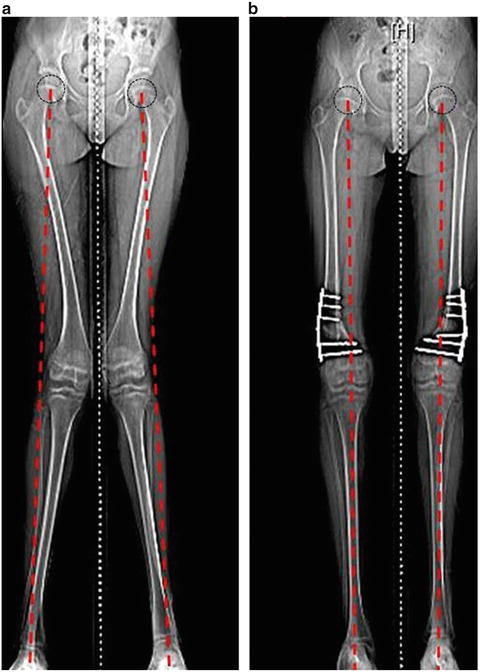
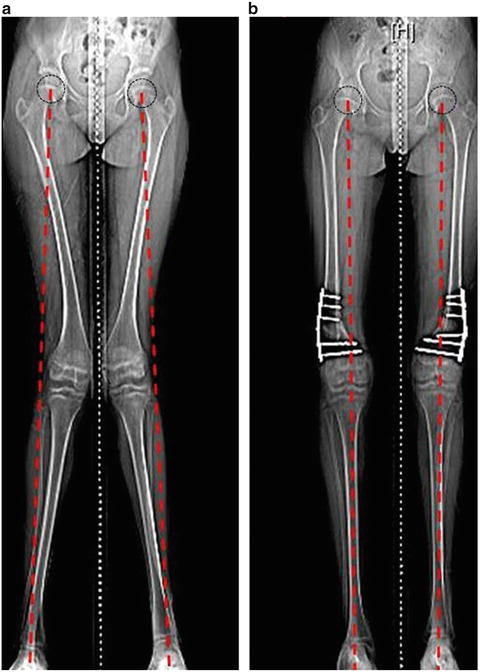
Fig. 6.11
CT scanograms (supine) comparing (a) pre-op and (b) post-op mechanical axis alignment (dotted red lines) in a 14-year-old girl with bilateral genu valgus. She underwent bilateral varus osteotomies of distal femora and fixation with locked compression plates. Supine CT scanogram was taken in this case. However, a standing full-length radiograph is a more accurate measure of alignment and should be preferred
Epiphyseal
Juxta-Apophyseal
Re-directional osteotomies of greater trochanter, calcaneal and tibial tuberosity improve muscle function by optimising the lever arm dysfunction [42–45] (Fig. 6.12).
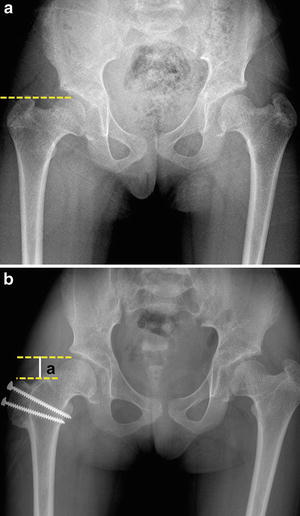
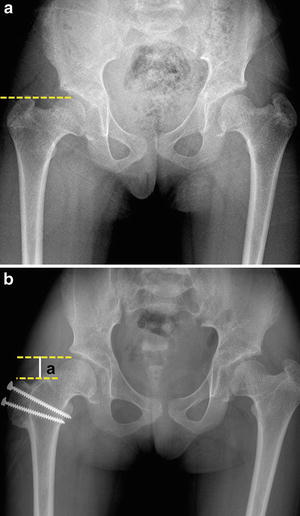
Fig. 6.12
(a) A 10-year-old girl with skeletal dysplasia with shortened abductor lever arm and abnormal articulo-trochanteric distance bilaterally. (b) Distal and lateral transfer of right greater trochanter was performed. The increased length of abductor lever arm following trochanteric transfer improves abductor power and gait and eliminates trochanteric impingement. a, restored articulo-trochanteric distance
Diaphysis
The common indications for diaphyseal osteotomies include metabolic bone disorders such as rickets, osteogenesis imperfecta, renal osteodystrophy and deformities secondary to traumatic or pathological fractures due to osteomyelitis and cystic lesions of bone. Posteromedial bowing of tibia and congenital limb deficiency form a special subset of diaphyseal osteotomies due to their propensity for complications due to associated soft-tissue inelasticity requiring special measures to avoid complications, for instance, postponing the deformity correction till the child with posteromedial tibial bowing is older and using a locked plate to prevent fractures or bowing of the regenerate that may cause recurrence of the deformity. Congenital pseudarthrosis of tibia is a rare disorder where the primary aim of treatment is to achieve union along with deformity correction and limb lengthening (Fig. 6.13).
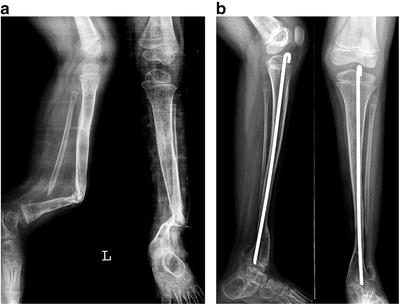
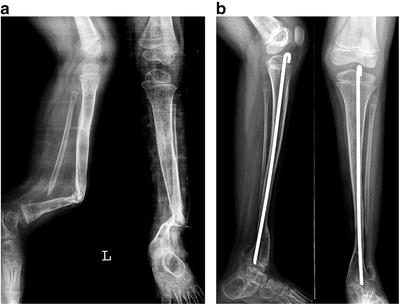
Fig. 6.13
(a) Anteroposterior and lateral views showing congenital pseudarthrosis of tibia in a 6-year-old boy. (b) Six years following corrective shortening osteotomy, resection of hamartomatous periosteum, bone grafting and revision intramedullary rodding
Metabolic bone disorders often exaggerate the natural curves of shafts of long bones, often leading to anterolateral bowing in the femur and tibia. The associated diaphyseal deformities are typically a generalised bow and multi-apical in nature, requiring multilevel osteotomies for correction. Severe forms of osteogenesis imperfecta often cause grotesque diaphyseal deformities. The poor quality of underlying bone warrants an intramedullary device to splint the bone after correction (see Fig. 6.7).
Certain Considerations Based on Location of the Deformity
Proximal Femur
In order to avoid damage to the capital physis, most of the proximal femoral osteotomies in children are carried out distant from the site (apex) of deformity. Such acute correction reorients the femoral head in valgus or varus, extension or flexion and rotation and is also used for shortening the femoral segment in certain cases of long-standing dislocated dysplastic hips.
Most of these osteotomies cannot be performed at the CORA due to the presence of pathological bone at the site of deformity as in proximal focal femoral deficiency or because of proximity to the proximal femoral physis and the tenuous blood supply to the femoral head [12, 13]. The common example is Perthes disease where proximal femoral varus or valgus osteotomies realign the articulation to either increase femoral head coverage or avoid impingement by the deformed head (Fig. 6.14). A combination of angulation, shortening and rotation is sometimes necessary to achieve optimal reorientation, for instance a proximal femoral osteotomy in a child with a congenital and neurogenic hip dislocation. In developmental coxa vara realignment of the physis to a more horizontal position prevents relapse.


Fig. 6.14
(a) Radiograph of a 6-year-old girl with bilateral dysplastic hips. (b) Open reduction was performed in conjunction with femoral shortening osteotomy to avoid avascular necrosis and de-rotation to correct anteversion and reduce the hip
Acute osteotomy of the intertrochanteric and sub-trochanteric regions of femur orients the proximal femoral physis more horizontally, thus converting shear forces to compressive forces.
Sub-capital realignment osteotomies are an example of correction at the level of deformity (CORA) in slipped capital femoral epiphysis but are rarely done because of the risk of vascular compromise to the femoral head blood supply (Fig. 6.15).
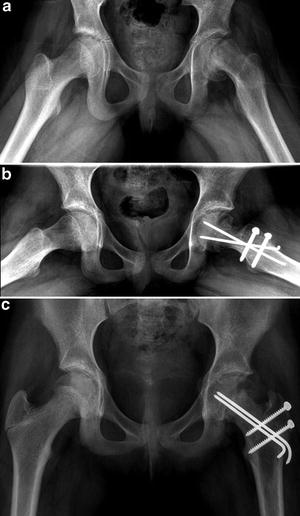
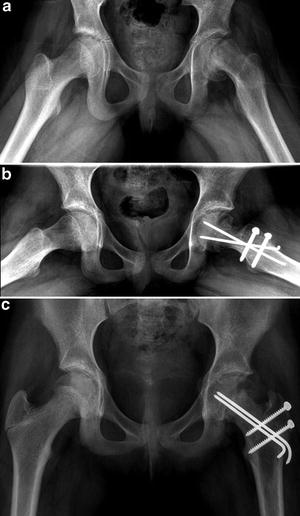
Fig. 6.15
(a) Acute on chronic SCFE left hip in a 12-year-old girl. (b, c) A modified Dunn’s osteotomy was done to realign the head and avoid femoro-acetabular impingement
Osteotomies Around the Knee
Flexion deformity of the knee associated with intractable joint contractures and muscle imbalance such as myelodysplasia, arthrogryposis, cerebral palsy and poliomyelitis can be corrected by supracondylar extension osteotomy of the femur. Such osteotomies reorient the arc of knee motion allowing full apparent extension and improve the child’s gait and function. A distal femur-shortening osteotomy can counter the long-standing flexion contracture without significantly affecting the hip extensor power. Correction of coronal plane angular deformities by closed or open wedge is the commonest indication around the knee. While this is now being rapidly replaced by the growth modulation technique, correction via an osteotomy has a role when the deformity is severe and growth potential is limited or where rapid correction is desirable. Lower limb deformities in children with certain skeletal dysplasias where growth modulation techniques play a limited role can also be treated by acute corrective osteotomy. The correction of deformity around the knee requires due consideration to neurological and vascular structures due to their proximity to the osteotomy site (Fig. 6.16).
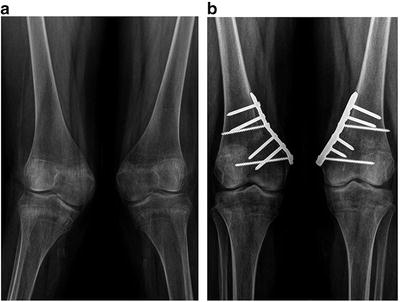
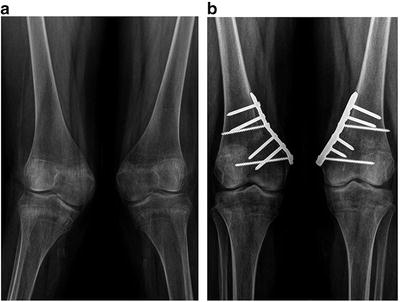
Fig. 6.16
(a) Bilateral genu valgus in a skeletally mature girl. (b) Bilateral closed wedge osteotomies and metaphyseal plate fixation were performed. Closing rather than open wedge osteotomies were performed to avoid common peroneal nerve injury. In femoral valgus deformity corrections greater than 30° we prefer to decompress the nerve
Acute Correction of Length Discrepancy
Correction of minor shortening can be obtained by acute lengthening. Brachymetatarsia correction by acute lengthening of up to 15 mm can be performed safely without any neurovascular compromise [34]. Trans-iliac osteotomy is a rarely done procedure which achieves lengthening when angular correction is not sought. In relative femoral neck lengthening, displacement osteotomy of the trochanter is combined with reshaping of the head, neck and trochanter to eliminate femoro-acetabular impingement and lengthen the lever arm (Fig. 6.17). Acute lengthening of the distal fibula by a step-cut or long oblique osteotomy is another example [43].
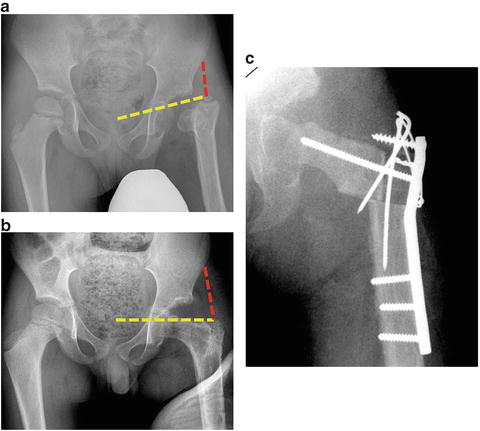
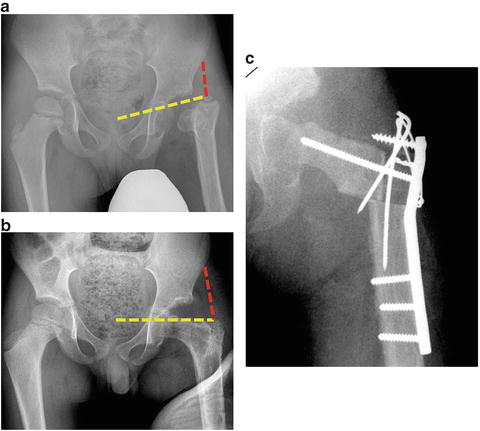
Fig. 6.17
(a) Radiograph of a 6-year-old boy with Choi’s type IVa [44] post-septic sequel left hip. (b) A neck-lengthening osteotomy with distal transfer of the greater trochanter shows optimisation of the hip abductor lever arm function. Red- and yellow-dotted lines indicate abductor lever arm and moment arm, respectively. (c) Immediate post-operative radiograph
Osteotomy with Adjuvant Procedures
Sometimes acute correction of the deformity can be combined with another procedure. This can be unifocal such as physeal bar excision with corrective osteotomy in hemi-physeal arrests around the knee (see Fig. 6.2). Alternatively it could be bifocal, where it is not optimal to do the angular correction at the same site as that of lengthening, for instance pelvic support osteotomy with distal femoral lengthening [47, 48]. Guided growth procedures can also be performed along with acute osteotomy, e.g. lateral proximal tibial guided growth along with ipsilateral Rab’s osteotomy for a child with Blount’s disease [49]. To counter the muscle imbalance brought about by cerebral palsy or meningomyelocele and other neuromuscular disorders, corrective osteotomy is combined with a muscle-balancing procedure, thereby avoiding relapse. For example, patellar tendon reefing is done following supracondylar extension osteotomy for fixed flexion deformity of the knee in cerebral palsy, and tibialis anterior transfer to the heel is combined with a calcaneal osteotomy in a child with excessive ankle dorsiflexion and weak plantarflexors.
Disease-Specific Indications
In certain conditions like osteogenesis imperfecta, when the child is non-ambulatory, the indication for a corrective osteotomy is to aid seating on a wheelchair, better hygiene and prevent further deformities rather than aligning mechanical axis. A long-standing dislocated or destroyed painful hip in a child can be managed by a pelvic support osteotomy combined with excision of the femoral head.
Box 6.2
Apophyseal reorientation osteotomies (calcaneal, greater trochanter and tibial tuberosity) lengthen the lever arm for optimal joint function.
Metabolic bone disorders usually cause multi-apical deformities which often require acute multilevel corrective osteotomies.
Acute shortening osteotomy may be performed primarily as in proximal femur to avoid avascular necrosis or in conjunction with deformity correction to avoid stretch on neurovascular structures.
Various realignment osteotomies of the proximal femur are described to increase joint coverage, reduce impingement, realign capital physis and increase the arc of motion.
Planning
Rules Governing Osteotomy Planning
Growth considerations have to be kept in mind when planning deformity correction. Hence osteotomy planning in children is somewhat different from that of adults where accurate line diagrams and metaphyseal angles are drawn with a view to achieve precise alignment of the knee mechanical axis. While restoring the mechanical axis is important in children, the deformity correction involves aligning the proximal and distal physes parallel to each other and perpendicular to the ground rather than merely achieving exact anatomical alignment. However in older children nearing skeletal maturity, the principles of restoring the mechanical axis used for adults are more applicable. While there are several methods for preoperative planning, we will illustrate our preferred planning methods for acute correction of the tibial and femoral deformities in children.
Planning for Tibial Deformity Correction
Step 1: Finding the CORA
The aim of surgical correction via an osteotomy is to achieve near-normal mechanical alignment and joint orientation of the lower extremity. After obtaining standing radiographs in the orthogonal planes, the joint lines at the knee and ankle are drawn (yellow-dotted lines) as shown in Fig. 6.18b. Red lines form the anticipated mechanical alignment angles of the tibia with the yellow-dotted lines tangential to the knee joint and talar dome. We consider the talar dome as the reference line for distal mechanical axis since the epiphysis and physis of the distal tibia are often misshapen in angular deformity in growing children. The mechanical axes intersect each other at the CORA and the angle [α] thus subtended is the magnitude of correction of the deformity (Fig. 6.18b). When the CORA is located in the bone near the obvious apex of deformity (area where the deformity visually appears to be maximum), correction can be obtained by a single osteotomy of magnitude “α” at this level.
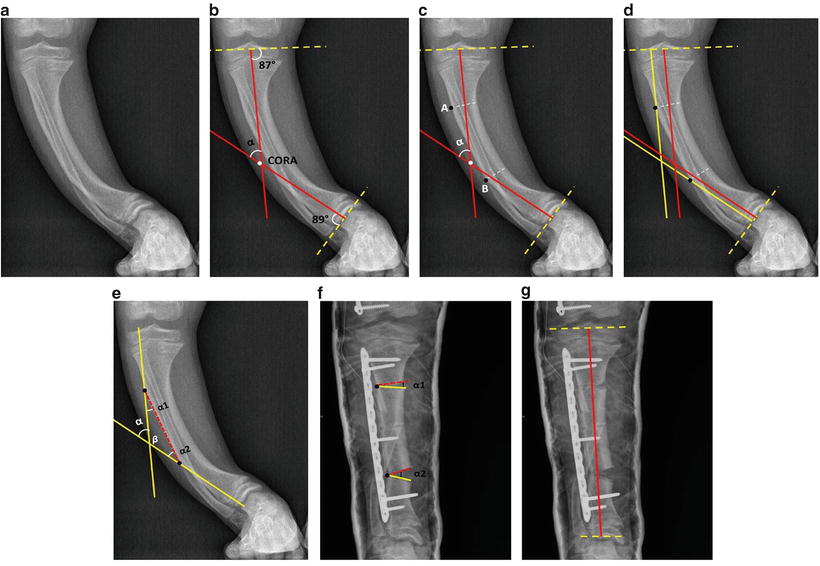
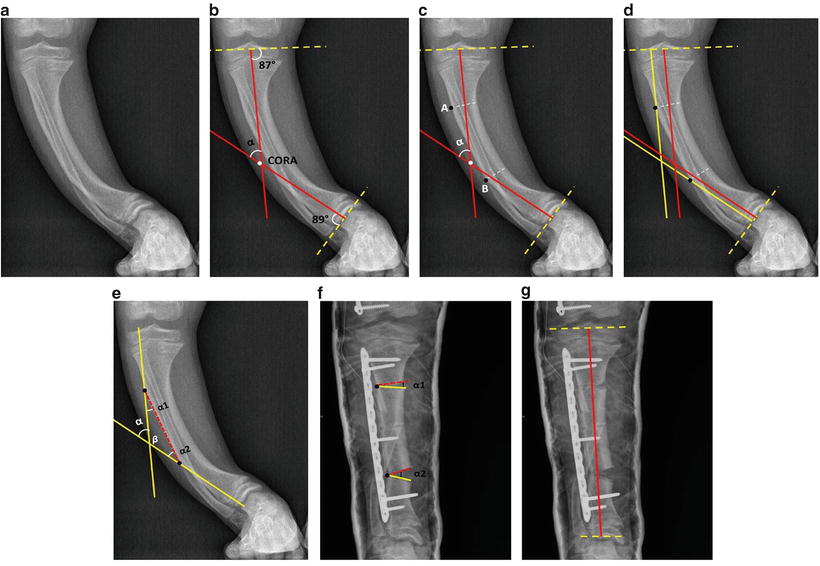
Fig. 6.18
Steps in planning correction of tibial deformity. (a) Bowing deformity of the tibia due to metabolic bone disease. (b) Yellow-dotted lines drawn tangential to the tibial plateau and talar dome. Mechanical axes [red dotted] of proximal and distal tibia are drawn from the centre of the former landmarks. The point of intersection of these lines is the CORA of the deformity and the angle “α” subtended is the magnitude of correction. (c) Two suitable sites for osteotomy “A” and “B” are plotted on the convex or concave tibial border based on execution of an open or closed wedge osteotomy, respectively. (d) Lines (yellow solid) are drawn parallel to the proximal and distal mechanical axes through these points. (e, f) The two points are connected by a line (red dotted), thus forming a triangle with α1, α2, and β angles. An opening wedge osteotomy of “α1” magnitude proximally and “α2” distally is planned. (g) Final radiographs after executing the osteotomies showing the corrected mechanical axis
Step 2: Finding the Axis of Correction for Two CORAs
In bowing deformities, the CORA could be located away from the obvious apex of deformity, suggesting the presence of two or more CORAs [23]. In such situations, two points (A and B) are plotted at the desired osteotomy sites on the cortex of the bone (Fig. 6.18c). These points form the centre of the arc of correction of the deformity. Lines (yellow) parallel to the mechanical axis of the individual fragments [red] are drawn through the proximal and distal points, respectively, as shown (Fig. 6.18d). These points are now connected by a single line (dotted red) (Fig. 6.18e, f). The sum of the two acute angles, α1 and α2, subtended in the triangle formed is equal to the total magnitude of correction “α”.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


