Fig. 41.1
Young girl from the Tojolabal community from the State of Chiapas, Mexico, with early lesions of actinic prurigo (AP)
It was first described in 1952 by López González from Argentina, under the name of Solar Prurigo [2]. Few years later, in 1954, Escalona and coworkers reported the first cases in Mexico [3], and from then on, AP has been identified in other latitudes such as Canada and in Central and South America [1]. Dr. Fabio Londoño, from Colombia, was the one who coined the term “actinic prurigo” [4].
Epidemiology
Begins in childhood between 6 and 8 years of age and is more common in women.
Commonly seen in dark-skinned people, Fitzpatrick’s phototypes IV and V.
Patients usually live in high-altitude, dry, sunny geographical areas.
AP occurs mainly in children between 6 and 8 years of age [5, 6] but can be seen at any age group [6]. It is more common in women, with a ratio of 2:1 compared to men [5–7] and commonly affects people with darker skin phototypes (IV and V of Fitzpatrick’s classification) [5, 6, 8] who live in dry and sunny geographical areas located in high altitudes, usually above 1,000 m above sea level. However, there have been cases reported to occur in people living at lower altitudes, even at sea level [5, 6].
Pathophysiology
Genetic Amerindian ancestry plays an important role in the pathogenesis of the disease [9], and may explain why AP predominates in countries, like Guatemala, Colombia, Honduras, Ecuador, Peru, Bolivia Mexico, that have indigenous populations with low cross-cultural influence, where there is a reported prevalence of the disease of 3.9 % [10] (Fig. 41.2).


Fig. 41.2
Well-developed lesions of AP in two patients from the Mazahua community from the State of Mexico, Mexico
Isolated cases have been reported in Costa Rica, Venezuela, Argentina, Uruguay, Chile, northern United States, in Canada’s Inuit population [1, 5, 7] (prevalence of 0.1 %) [10], Australia, Great Britain, and Thailand [1].
Little is known about the exact etiology of this disease. Some identified factors involved are low socioeconomic status, family history [8], living in rural areas, continuous contact with farm animals and exposure to wood smoke [11].
Regarding genetic predisposition, it has been shown that, in Mexico, 90–92.8 % of patients with AP express HLA-DR4 [12–15] and the allele HLA-DRB1*0407 [1, 7, 10] the most common subtype (60–80 %) [12, 15].
HLA-DR4 has also been identified in European patients with AP [1, 10]. Other related alleles associated with the disease are HLA-A28 and B39 in Mexico [1, 7], HLA-A24, HLA-Cw4, and DRB1*14 in Canada [7, 10], HLA-Cw4 in Chimila indians from Colombia [16], and HLA-B40 and Cw3 in Bogota [1, 7, 10].
Increased expression of HLA-B40 and Cw3 is seen in populations with strong Amerindian genetic lineage and may explain why this disease is more common in this ethnic group [1, 17]. HLA subtype DRB1*0407 has also been found to be more frequent in Colombian patients with AP [18].
In 1984, Moncada and coworkers [19] suggested that the skin of patients with AP had an abnormal immune response characterized by an increased number of T lymphocytes in peripheral blood, especially T helper cells (CD4+), and also an increased number of CDIa+ dendritic cells in the dermal inflammatory infiltrate [5, 20]. It was subsequently observed that this abnormal response was induced by solar radiation, particularly the spectrum of ultraviolet radiation A (UVA) and B (UVB). However, visible light also has an important role in the pathogenesis of the disease [1, 5, 21].
UVB radiation stimulates the production of tumor necrosis factor alpha (TNF-α) by epidermal keratinocytes, especially those from the suprabasal layer [1, 6]. This cytokine is able to activate immunoreactivity and expression of adhesion molecules on keratinocytes, which promote the migration of inflammatory cells that produce epidermal tissue injury and necrosis [6, 22]. TNF-α also initiates the activation of transcription factor NF-κβ and programmed cell death (apoptosis), so it is very likely that this immune response occurs in the pathophysiology of AP [23].
B cells in lymphoid follicles express CD80 (B7) and promote proliferation of Th2 cells that release IL-5 (eosinophil activator) and IL-4 (which stimulates production of IgE [24] and the activation of mast cells). This process promotes the formation of the characteristic ectopic germinal centers (lymphoid follicles) on the lips, also documented in other conditions of hypersensitivity, autoimmunity, or infection [25].
On the other hand, lymphocytes T-CD4+ induce the synthesis of IL-2, which activates natural killer cells and promotes the production of IgE antibodies [1] that have been demonstrated in situ and in serum of patients with AP [26].
Mast cells also play an important role in both inflammatory and allergic reactions. In 2007, a Mexican study has shown a higher density of mast cells in the lip lesions of patients with AP, compared to normal and inflamed mucosa due to other pathologic processes [26].
The presence of increased levels of IgE, eosinophils, and mast cells suggests a hypersensitivity reaction as one of the mechanisms in the pathophysiology of AP [25]. Generally, hypersensitivity reactions occur after exposure to an antigen that activates effector cells. AP may be classified as a delayed hypersensitivity reaction [19, 27, 28] type IVa, because after sun exposure, keratinocytes are able to produce TNF-α [1, 6]. It can also be regarded as IVb type reaction due to the presence of increased levels of IgE, eosinophils, and mast cells [29–31].
Clinical Presentation
Polymorphous dermatitis affecting photoexposed areas of face, neck, trunk, and extremities.
Lesions consist of extremely itchy erythematous macules, papules, infiltrated plaques. excoriations, lichenification, scars, and residual hypo or hyperpigmentation
Characteristically, it affects lips and conjunctiva with eventual pseudopterygium formation.
AP is a polymorphous photodermatosis. Patients usually have lesions on sun-exposed skin of face, neck, trunk, and extremities, and the lesions are distributed in a bilateral and symmetrical array (Fig. 41.3). This dermatosis predominates over areas where radiation hits with more intensity, such as nasal dorsum, zygomatic and superciliary arches, lower lip, and conjunctiva [5, 12]. Less frequently, lesions can be observed in non-photoexposed skin [9, 15] (Fig. 41.4).



Fig. 41.3
Patients with AP usually have lesions on sun-exposed skin of face, neck, trunk, and extremities and show a bilateral and symmetrical distribution. Associated xerosis can be seen

Fig. 41.4
Mild AP. Lesions predominate over nasal dorsum, zygomatic and superciliary arches, lower lip, and conjunctiva. Hypopigmented residual lesions can be seen
AP is an inflammatory dermatosis characterized by erythematous macules and papules that converge to form infiltrated plaques. Because it is extremely itchy, there are also excoriations, scale-crusts, lichenification, scars, and residual hypo or hyperpigmentation [5–7, 9, 12] (Fig. 41.5).


Fig. 41.5
Moderate to severe AP. Papular lesions become confluent forming infiltrated plaques. There are more exulcerations covered with scale crusts and lichenified areas, due to severe scratching
On the vermilion border of the lips, erythema, edema, fissures, and ulcers covered by serohemorrhagic scales can be observed. This is a very characteristic manifestation of the disease and is referred to as actinic prurigo cheilitis (APC). There is sometimes associated gingival hypertrophy, possibly secondary to mouth breathing due to the uncomfortable symptoms on the lip [12]. APC is a common clinical manifestation and more frequently affects the lower lip. Up to 65 % of children with AP can show labial lesions [1], and in 27.6 %, it could be the only manifestation of the disease [12] (Fig. 41.6).


Fig. 41.6
Actinic prurigo cheilitis. Lips can be swollen, with areas of erythema, fissures and ulcers covered by serohematic scales
Conjunctiva can be affected in approximately 45 % of patients. Conjunctivitis of AP initially presents with hyperemia, photophobia, increased tearing, and subsequent pseudopterygium formation, and in severe cases, there can be partial loss of the visual fields. It appears that conjunctival alterations are usually a late manifestation of the disease [5, 9, 12] (Fig. 41.7).


Fig. 41.7
Actinic prurigo conjunctivitis. Conjunctivitis of AP initially presents with hyperemia, photophobia, increased tearing and subsequent pseudopterygium formation
AP has a chronic clinical course with frequent exacerbations after sun exposure. In geographical areas where seasons are well defined, flares usually occur during spring and summer and decrease in the fall [9, 15]. In contrast, in regions with tropical climate without marked seasonal variations, exacerbations may occur year-round related with constant exposure to sunlight [5].
Histopathology
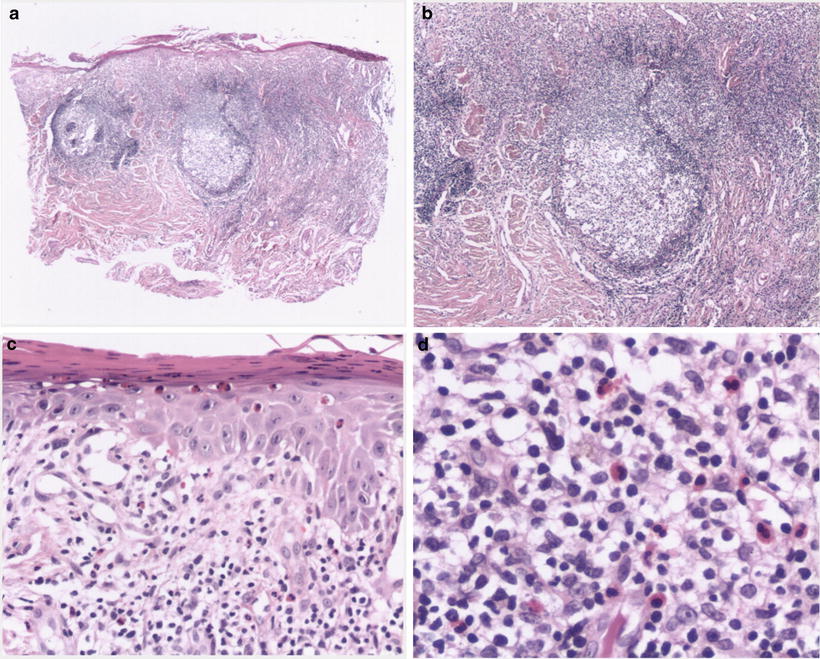
The microscopic picture of skin lesions shows hyperkeratosis, foci of parakeratosis, acanthosis, thickening of the basement membrane, and a superficial perivascular inflammatory infiltrate of lymphocytes. Sometimes, there are only mild inflammatory changes with epidermal hyperplasia, suggestive of a chronic dermatitis; however, the presence of an intense nodular inflammatory lymphocytic infiltrate with numerous eosinophils and mast cells suggests the diagnosis [32]. Unlike other photodermatoses, adnexal structures are not affected and solar elastosis is not a common finding.
Histology of APC shows hyperkeratosis, scale crusts covering ulcerated areas, mild acanthosis, spongiosis, and mild vacuolar alteration of the basal layer. At the superficial portion of the submucosa, eosinophils and melanophages can be found, and deeper in the lamina propria, there are dilated capillary vessels, interstitial edema, and a band-like or nodular lymphocytic infiltrate. Lymphocytes may aggregate and form well-defined ectopic lymphoid follicles. This particular histologic picture is named “follicular cheilitis” and is a very characteristic feature of APC [12] (Fig. 41.8).