Background
Determining the depth of villous invasiveness before delivery is pivotal in planning individual management of placenta accreta. We have evaluated the value of various ultrasound signs proposed in the international literature for the prenatal diagnosis of accreta placentation and assessment of the depth of villous invasiveness.
Objective
We undertook a PubMed and MEDLINE search of the relevant studies published from the first prenatal ultrasound description of placenta accreta in 1982 through March 30, 2016, using key words “placenta accreta,” “placenta increta,” “placenta percreta,” “abnormally invasive placenta,” “morbidly adherent placenta,” and “placenta adhesive disorder” as related to “sonography,” “ultrasound diagnosis,” “prenatal diagnosis,” “gray-scale imaging,” “3-dimensional ultrasound”, and “color Doppler imaging.”
Study Design
The primary eligibility criteria were articles that correlated prenatal ultrasound imaging with pregnancy outcome. A total of 84 studies, including 31 case reports describing 38 cases of placenta accreta and 53 series describing 1078 cases were analyzed. Placenta accreta was subdivided into placenta creta to describe superficially adherent placentation and placenta increta and placenta percreta to describe invasive placentation.
Results
Of the 53 study series, 23 did not provide data on the depth of villous myometrial invasion on ultrasound imaging or at delivery. Detailed correlations between ultrasound findings and placenta accreta grading were found in 72 cases. A loss of clear zone (62.1%) and the presence of bridging vessels (71.4%) were the most common ultrasound signs in cases of placenta creta. In placenta increta, a loss of clear zone (84.6%) and subplacental hypervascularity (60%) were the most common ultrasound signs, whereas placental lacunae (82.4%) and subplacental hypervascularity (54.5%) were the most common ultrasound signs in placenta percreta. No ultrasound sign or a combination of ultrasound signs were specific of the depth of accreta placentation.
Conclusion
The wide heterogeneity in terminology used to describe the grades of accreta placentation and differences in study design limits the evaluation of the accuracy of ultrasound imaging in the screening and diagnosis of placenta accreta. This review emphasizes the need for further prospective studies using a standardized evidence-based approach including a systematic correlation between ultrasound signs of placenta accreta and detailed clinical and pathologic examinations at delivery.
Introduction
Placenta accreta (PA) is an iatrogenic 20th century disorder of human placentation, characterized by the abnormal attachment or invasion of placental tissue to the underlying uterine musculature. PA may have been observed before the 20th century but all epidemiologic studies have shown a direct association between the increase in cesarean delivery (CD) and the increased incidence of PA in subsequent pregnancies. PA is not exclusively a consequence of CD and much smaller surgical damage to the integrity of the uterine lining, such as those following “uterine curettage, manual delivery of the placenta, postpartum endometritis and previous hysteroscopic surgery, endometrial resection, and uterine artery embolization (UAE)”, has been associated with PA in subsequent pregnancies. The development of PA was also reported in women with no surgical history but presenting with uterine pathology such as bicornuate uterus, adenomyosis, submucous fibroids, and myotonic dystrophy. These individual case reports suggest that intramyometrial implantation of villous tissue is not always secondary to uterine surgery and may explain the few rare cases of PA observed before the 20th century.
PA was first defined in 1937 by Irving and Hertig, as the “abnormal adherence of the afterbirth in whole or in parts to the underlying uterine wall.” The failure of the placenta to separate normally from the uterus after delivery is typically accompanied by severe postpartum hemorrhage, and attempts to remove a PA typically provoke further major hemorrhage, which is associated with increased maternal morbidity and mortality. Modern pathologists have graded PA into placenta creta (PC) or placenta vera, placenta increta (PI), and placenta percreta (PP) according to the depth of villous invasiveness. In PC, the villi adhere to the myometrium with no intermediate decidual layers between the tip of the anchoring villi and the muscular cells but do not invade the myometrium. In PI, the villi penetrate deeply into the myometrium up to the external layer whereas in PP, the invasive villous tissue reaches and/or penetrates through the uterine serosa. The PA spectrum can therefore be subdivided into PC for abnormally adherent placentation and PI and PP for abnormally invasive placentation. Cases of PA are also often subdivided into total, partial, or focal according the amount of placental issue involved. More recently, it has been suggested that cesarean scar pregnancy represents a precursor of one of the different grades of PA.
Several concepts have been proposed to explain the pathophysiology of PA. The oldest is based on a theoretical primary defect of the biological functions of the trophoblast, leading to excessive adherence or invasion of the myometrium. The other prevailing hypothesis is that of a secondary defect of the endometrial-myometrial interface leading to a failure of normal decidualization in the area of the uterine scar allowing trophoblastic infiltration beyond the superficial myometrium and villous development inside the myometrium. Although, the pathogenic mechanisms of the different types of accreta placentation, including scar pregnancies, are similar, the anatomical and clinical consequences vary widely. In placenta vera, the villi simply adhere to the superficial layer of the myometrium whereas in PI and PP the villous tissue invades into and may penetrate through the entire uterine wall thickness and reach the surrounding pelvic tissues and organs.
The worst clinical outcome arises when PA and, in particular the invasive forms of PA i.e. PI or PP are unsuspected at the time of delivery and the surgeon attempts to remove the invasive part of the placenta leading immediately to major hemorrhage and an increasing need for emergency hysterectomy. Prenatal diagnosis of PA has therefore become essential for the safe management of this increasingly common obstetric complication. However, recent population studies from the United Kingdom and the United States have shown that PA remains undiagnosed before delivery in between half and a third of cases. Determining the depth of placental invasion is essential for planning of individual management of women diagnosed with PA.
The objective of this review is to evaluate the value of the various ultrasound signs described in the international literature for the prenatal diagnosis of PA in general and for the assessment of the depth of villous invasiveness in the uterine wall in particular.
Materials and Methods
Information sources and search strategy
We conducted a systematic review of the literature and selected relevant studies published from the first prenatal ultrasound description of PA by Tabsh et al in 1982 through March 30, 2016. We undertook a PubMed and MEDLINE search using combinations of key words “placenta accreta,” “placenta creta,” “placenta increta,” “placenta percreta,” “abnormally invasive placenta,” “morbidly adherent placenta,” and “placenta adhesive disorder” as related to “sonography,” “ultrasound diagnosis,” “prenatal diagnosis,” “gray-scale imaging,” “3-dimensional (3-D) ultrasound”, and “color Doppler imaging” (CDI). We limited the search to studies published in English.
Eligibility criteria
The primary eligibility criteria were articles that correlated prenatal ultrasound imaging with pregnancy outcome. We used ultrasound signs from the standardized descriptions proposed recently by the European Working Group on Abnormally Invasive Placenta and the Abnormally Invasive Placenta International Expert Group. On gray-scale imaging the signs of PA are: loss of the clear zone in the myometrium under the placental bed; myometrial thinning to <1 mm or undetectable; intraplacental lacunae often large and irregular (“moth-eaten” areas); bladder wall interruption or loss (hyperechoic line between serosa and bladder lumen); placental bulge distorting the extrauterine organs; and focal exophytic mass of placental tissue extending beyond the serosa. On CDI the signs used are: uterovesical hypervascularity between the myometrium and the posterior wall of the bladder; subplacental hypervascularity (placental bed); bridging vessels across the myometrium and beyond the serosa; and lacunae feeder vessels with high velocity (turbulent) flow from the arterial vasculature of myometrium.
Study selection
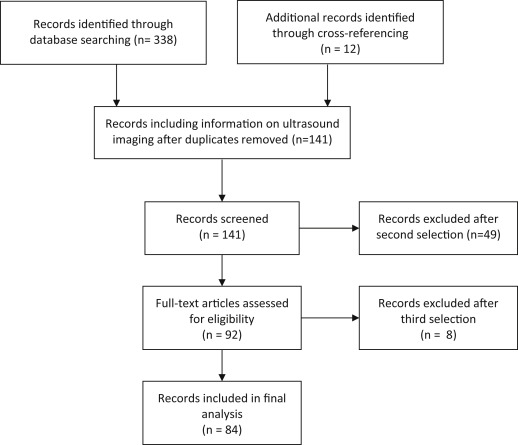
The initial database search provided 338 reports of which only 129 included information on ultrasound imaging using the key words described above ( Figure ). Cross-referencing provided an additional 12 reports, making a total of 141 records. After the second selection, letters with no description of the case, case reports with inconclusive diagnosis, commentaries, and reviews (n = 49) were excluded. A further 8 reports with no description of ultrasound features were further excluded leaving 84 reports for analysis.
The articles were separated into case reports (n = 31) and series (n = 53), and were reviewed independently. PA was subdivided in PC to describe superficially adherent placentation and PI and PP to describe invasive placentation.
Synthesis of results
Data containing study setting, study type, characteristics of study population, definition of PA, terminology, grading, and ultrasound description of placental structure were obtained for each of 83 studies selected. To evaluate the relationships among the depth of villous invasiveness, ultrasound signs, and clinical findings, management procedures including CD hysterectomy, focal myometrial resection, UAE, uterine artery balloon occlusion, uterine artery ligation (UAL), intrauterine balloon tamponade, methotrexate (MTX), B-Lynch suture, and lesions described during pathological examination were also extracted.
The case report data were analyzed using a data analysis and statistical software package (StatGraphic; Manugistics, Rockville, MD).
Materials and Methods
Information sources and search strategy
We conducted a systematic review of the literature and selected relevant studies published from the first prenatal ultrasound description of PA by Tabsh et al in 1982 through March 30, 2016. We undertook a PubMed and MEDLINE search using combinations of key words “placenta accreta,” “placenta creta,” “placenta increta,” “placenta percreta,” “abnormally invasive placenta,” “morbidly adherent placenta,” and “placenta adhesive disorder” as related to “sonography,” “ultrasound diagnosis,” “prenatal diagnosis,” “gray-scale imaging,” “3-dimensional (3-D) ultrasound”, and “color Doppler imaging” (CDI). We limited the search to studies published in English.
Eligibility criteria
The primary eligibility criteria were articles that correlated prenatal ultrasound imaging with pregnancy outcome. We used ultrasound signs from the standardized descriptions proposed recently by the European Working Group on Abnormally Invasive Placenta and the Abnormally Invasive Placenta International Expert Group. On gray-scale imaging the signs of PA are: loss of the clear zone in the myometrium under the placental bed; myometrial thinning to <1 mm or undetectable; intraplacental lacunae often large and irregular (“moth-eaten” areas); bladder wall interruption or loss (hyperechoic line between serosa and bladder lumen); placental bulge distorting the extrauterine organs; and focal exophytic mass of placental tissue extending beyond the serosa. On CDI the signs used are: uterovesical hypervascularity between the myometrium and the posterior wall of the bladder; subplacental hypervascularity (placental bed); bridging vessels across the myometrium and beyond the serosa; and lacunae feeder vessels with high velocity (turbulent) flow from the arterial vasculature of myometrium.
Study selection
The initial database search provided 338 reports of which only 129 included information on ultrasound imaging using the key words described above ( Figure ). Cross-referencing provided an additional 12 reports, making a total of 141 records. After the second selection, letters with no description of the case, case reports with inconclusive diagnosis, commentaries, and reviews (n = 49) were excluded. A further 8 reports with no description of ultrasound features were further excluded leaving 84 reports for analysis.
The articles were separated into case reports (n = 31) and series (n = 53), and were reviewed independently. PA was subdivided in PC to describe superficially adherent placentation and PI and PP to describe invasive placentation.
Synthesis of results
Data containing study setting, study type, characteristics of study population, definition of PA, terminology, grading, and ultrasound description of placental structure were obtained for each of 83 studies selected. To evaluate the relationships among the depth of villous invasiveness, ultrasound signs, and clinical findings, management procedures including CD hysterectomy, focal myometrial resection, UAE, uterine artery balloon occlusion, uterine artery ligation (UAL), intrauterine balloon tamponade, methotrexate (MTX), B-Lynch suture, and lesions described during pathological examination were also extracted.
The case report data were analyzed using a data analysis and statistical software package (StatGraphic; Manugistics, Rockville, MD).
Results
Case reports characteristics
The case reports included 38 individual cases with prenatal ultrasound findings. PA grading was confirmed clinically or histopathologically as PC in 13 cases, PI in 16 cases, and PP in 9 cases.
A planned CD hysterectomy with or without UAE or UAL was performed in 2 PC, 9 PI, and 7 PP. In the other 20 cases conservative management was attempted including focal myometrial resection with or without suture or MTX, uterine curettage, and the placenta left in situ with MTX or UAE. Conservative management was unsuccessful in 12 cases, including 5 PC, 6 PI, and 1 PP, and required a secondary hysterectomy. A dissection or partial resection of the bladder was required in 4 cases of PP. The mean gestational age at delivery was 30.6 weeks (SD 7.5; range 15-39 weeks). A detailed description of the pathologic findings was available in 28 cases. In the remaining 10 cases it was not available following successful conservative management but the PA grading was described at delivery.
Case reports synthesis of results
The terminology “placenta accreta” was used by 27 authors of case reports, “morbidly adherent placenta” by 2 authors, and “abnormal placentation” by 1 author. Two authors reporting on 3 cases did not describe the surgical history. In 5 (14.3%) cases there was a history of uterine curettage only and in 7 (20.0%) the women presented with a combined history of CD, myomectomy, and/or curettage. An obstetric history of CD was reported in 23 of 35 (65.7%) remaining cases.
Gray-scale imaging was used by all authors. In 8 cases, including 2 PC, 5 PI, and 1 PP, only gray-scale imaging signs were described, whereas in the remaining 30 cases, including 11 PC, 11 PI, and 8 PP, both gray-scale and CDI were reported. Table 1 displays the ultrasound signs identified in the diagnosis of the 38 case reports included in the review according to the depth of villous myometrial invasion. The mean gestational age at diagnosis was 24.3 weeks (SD 6.8; range 13-36 weeks). A loss of clear zone (92.3%) and bridging vessels (90.9%) were the most common ultrasound signs for PC. In cases of PI, the loss of clear zone (87.5%) and subplacental hypervascularity (81.8%) were the most common signs, whereas for PP, placental lacunae were found in all cases (100%) and subplacental hypervascularity was found in 6 cases (75%).
| Ultrasound signs | PC n (%) | PI n (%) | PP n (%) |
|---|---|---|---|
| Gray-scale parameters | (n = 13) | (n = 16) | (n = 9) |
| Loss of clear zone | 12 (92.3) | 14 (87.5) | 5 (55.6) |
| Myometrial thinning | 6 (46.2) | 11 (68.8) | 3 (33.3) |
| Placental lacunae | 5 (38.5) | 9 (56.3) | 9 (100) |
| Bladder wall interruption | 1 (7.7) | 2 (12.5) | 2 (22.2) |
| Placental bulge | – | 1 (12.5) | 1 (11.1) |
| Focal exophytic mass | – | – | 1 (11.1) |
| CDI parameters | (n = 11) | (n = 11) | (n = 8) |
| Uterovesical hypervascularity | 1 (9.1) | 2 (18.2) | 2 (25.0) |
| Subplacental hypervascularity | 5 (45.5) | 9 (81.8) | 6 (75.0) |
| Bridging vessels | 10 (90.9) | 7 (63.6) | 2 (25.0) |
| Lacunae feeder vessels | 2 (18.2) | 6 (55.5) | 4 (50.0) |
Series characteristics
The 53 series included 24 prospective and 29 retrospective studies with a total of 1078 cases of PA. All series except 8, which did not report data on surgical history, included women presenting with placenta previa and a history of CD and/or other uterine surgeries. In 21 series, including 568 cases of PA, the depth of villous invasiveness was not described. In the other 32 series, the distribution of the different categories of PA was reported, including 240 PC, 112 PI, and 158 PP.
A planned CD hysterectomy, with or without UAE or UAL, was the primary management option in 44 series. In 13 series, conservative management was attempted depending on the degree of myometrial invasion with secondary hysterectomy in cases of failure and in 1 series conservative management was successful in all cases. In 7 series, no information was available on the outcome and management. Overall, a CD hysterectomy was performed in 597 of 806 (74.1%) cases for which the data were available. The mean gestational age range at delivery was 34-37 weeks. A detailed description of the pathologic findings was available in 29 series. In 12 series, the pathologic examination was reported as performed but no data were provided and in 11 series there was no histopathologic information.
Series synthesis of results
The terminology used to describe PA was diverse. Seven studies used the term “morbidly adherent placenta,” 2 used “placental adhesive disorders,” 2 used “abnormally invasive placentation,” 2 used “abnormally adherent placenta” or “abnormal placental adherence,” 1 use “advanced invasive placentation,” and 1 used the term “abnormal myometrial invasion.”
Gray-scale ultrasound was used, and the corresponding data were presented by all authors except 1. In 10 series, gray-scale imaging only was used ; in 1 series sequential 2- and 3-D ultrasound were used. In the remaining 41 series, data from both 2-D gray-scale ultrasound and CDI were available. The gestational mean range at diagnosis in 31 series for which the information was available was 20-34 weeks. Table 2 displays the ultrasound signs used by authors to diagnose PA in the 53 series. The most commonly used signs were loss of clear zone (98%) and placental lacunae (96.1%) for gray-scale imaging and subplacental hypervascularity (85.7%) and bridging vessels (61.9%) for CDI. The authors of 8 series provided detailed data on 2-D ultrasound examination and placental grading. The corresponding data are presented in Table 3 . The presence of placental lacunae (78.9%) and subplacental hypervascularity (36.7%) were the most common ultrasound signs found. In 3 of these series the authors provided details of the placental grading for each individual standard ultrasound sign. These data were combined with those from the case reports ( Table 4 ) raising the number of cases available for analysis to 72. This analysis confirmed that a loss of clear zone (62.1%) and the presence of bridging vessels (71.4%) were the most common ultrasound signs found in cases of PC, that a loss of clear zone (84.6%) and subplacental hypervascularity (60%) were the most common sings in PI, whereas placental lacunae (82.4%) and subplacental hypervascularity (54.5%) were the most common signs for PP. No ultrasound sign or combination of ultrasound signs were specific of the depth of accreta placentation. No series reported on the lateral extension of accreta placentation and in particular on the involvement of the cervix.
| Ultrasound signs | n (%) |
|---|---|
| Gray-scale parameters (n = 52) | |
| Loss of clear zone | 50 (98.0) |
| Myometrial thinning | 34 (66.7) |
| Placental lacunae | 49 (96.1) |
| Bladder wall interruption | 30 (58.8) |
| Placental bulge | 11 (22.0) |
| Focal exophytic mass | 13 (25.5) |
| CDI parameters (n = 42) | |
| Uterovesical hypervascularity | 20 (47.6) |
| Subplacental hypervascularity | 36 (85.7) |
| Bridging vessels | 26 (61.9) |
| Lacunae feeder vessels | 22 (52.4) |
| Variables | References | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 65 n | 79 n | 84 n | 89 n | 95 n | 98 n | 102 n | 107 n | T n | |
| No. of cases | 15 | 10 | 9 | 41 | 26 | 32 | 10 | 9 | 152 |
| Placental grading | n | ||||||||
| PC | 8 | 8 | 5 | 15 | 16 | 16 | 3 | 1 | 72 |
| PI | 3 | 1 | 3 | 9 | 0 | 12 | 4 | 2 | 34 |
| PP | 4 | 1 | 1 | 17 | 10 | 4 | 3 | 6 | 46 |
| Gray-scale parameters (n = 152) | % | ||||||||
| Loss of clear zone | 7 | 10 | 4 | 37 | 23 | 20 | 5 | 0 | 69.7 |
| Myometrial thinning | 0 | 0 | 0 | 0 | 19 | 32 | 3 | 0 | 51.0 |
| Placental lacunae | 10 | 10 | 5 | 30 | 23 | 28 | 5 | 9 | 78.9 |
| Bladder wall interruption | 3 | 0 | 0 | 0 | 0 | 15 | 16 | 1 | 23.0 |
| Placental bulge | 0 | 0 | 1 | 0 | 9 | 0 | 0 | 0 | 6.6 |
| Focal exophytic mass | 0 | 0 | 1 | 0 | 11 | 0 | 0 | 0 | 7.9 |
| CDI parameters (n = 128) | % | ||||||||
| Uterovesical hypervascularity | 0 | 0 | 0 | 0 | 11 | 30 | 2 | 6 | 11.3 |
| Subplacental hypervascularity | 0 | 10 | 0 | 0 | 0 | 30 | 0 | 7 | 36.7 |
| Bridging vessels | 0 | 0 | 0 | 0 | 12 | 0 | 0 | 0 | 9.3 |
| Lacunae feeder vessels | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 6 | 8.6 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


