Accessing Indwelling Central Lines
Susan M. Fuchs
Introduction
In children, numerous illnesses exist that require long-term parenteral pharmacologic or nutritional therapy and repetitive blood drawing. Several long-term central venous access devices (indwelling lines) have been developed that allow the administration of antibiotics, chemotherapy, blood, hyperalimentation, and fluids, often on an outpatient basis. When a child with one of these indwelling lines is evaluated in the emergency department (ED), the ability to properly access the device can be an important skill for providing optimal management. Because these devices directly access the central circulation, it is always necessary to follow sterile procedures to reduce the risk of infection. Air embolism and central vein thrombosis are additional risks.
Types of Equipment
Several indwelling lines are currently available, and clinicians should become familiar with the ones used most commonly in their own medical center. Differences among the devices include access, flushing, and aftercare.
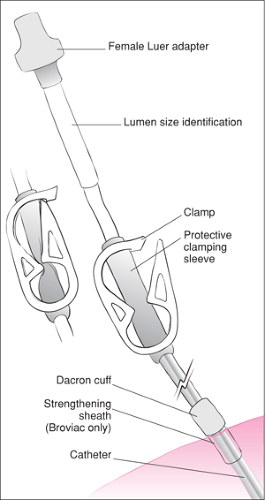
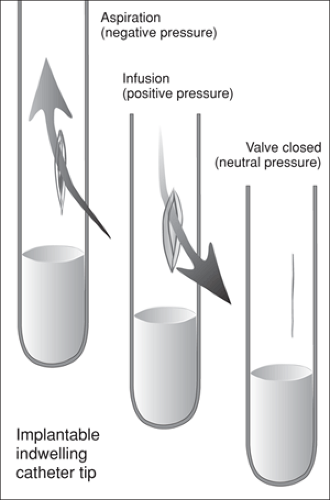
The first partially implanted catheter was developed in 1973 by Broviac and consisted of a Silastic catheter that was used to administer total parenteral nutrition (TPN). The Broviac catheter was 18 gauge (1.0 mm internal diameter) and was inserted into the external jugular, subclavian, or cephalic vein, with the distal tip positioned in the right atrium. The proximal end was tunneled under the skin to exit on the chest (1). The same procedure for placement is used today. A Dacron cuff located on the catheter is positioned in the subcutaneous tunnel and serves two purposes: (a) a fibrin sheath develops around it within about 2 weeks that anchors the line in the tunnel, and (b) it acts as a mechanical barrier to infection (1,2). In 1979, Hickman enlarged this catheter (16 gauge, 1.6 mm) to administer chemotherapy and to facilitate blood drawing (1,2). More recently, single-, double-, and triple-lumen catheters with a wider range of sizes (0.5 to 2.6 mm internal diameter) have been developed. In addition to the Broviac (Evermed) and Hickman (Fig. 74.1), other commonly used catheters include the Leonard, Raaf, Hemed, and Corcath (2). Another recent advance is the development of the Groshong catheter, which has an antireflux slit valve near the distal (implanted) tip (Fig. 74.2). The slit opens outward for administrating fluid and inward for aspirating blood, but it otherwise remains closed. The advantage of this type of catheter is that blood does not remain in the lumen of the catheter after it is flushed, so only saline flushes (no heparin) are used (2).
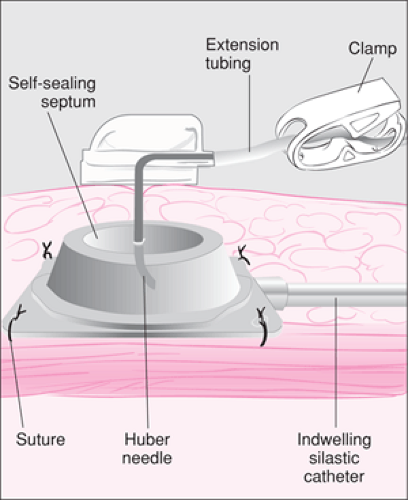
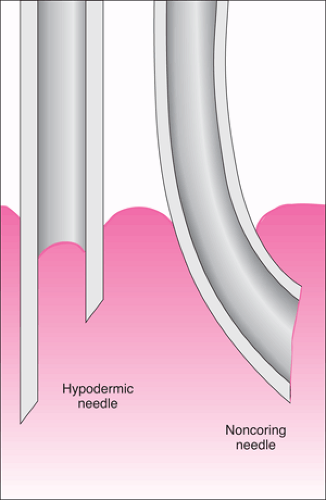
In 1982, the totally implantable central venous access device was introduced. It consists of a silastic catheter attached to a subcutaneous injection port or reservoir (Fig. 74.3). The catheter is placed in a central vein until the distal tip is at the junction of the superior vena cava and right atrium. The proximal portion is tunneled under the skin, but rather than exiting the skin, it is attached to a reservoir that is sutured into a subcutaneous pocket on the chest (1,2). The reservoir, which can be single or double lumen, is covered with a silicone septum that is self-sealing for up to 2,000 punctures (1). A special needle (Huber), which is noncoring and has a solid tip and a side hole opening, is used for access (Fig. 74.4). Most have a 90-degree bend, although some are straight (1,3). The reservoirs are made of plastic, stainless steel, or titanium. The plastic and titanium ports are light and do not interfere with magnetic resonance imaging studies (4). The Port-A-Cath (Pharmacia) comes in two sizes—an infant size (outer diameter 2 mm, internal diameter 0.5 mm)
and a child size (outer diameter 2.8 mm, internal diameter 1 mm) (1,3). Other available devices include the Infuse-A-Port, Mediport, and Babyport (1,2,4).
and a child size (outer diameter 2.8 mm, internal diameter 1 mm) (1,3). Other available devices include the Infuse-A-Port, Mediport, and Babyport (1,2,4).
Two additional types of central line that have seen increased use in the neonatal and pediatric populations include the peripherally inserted central catheter (PICC) (see also Chapter 19) and the percutaneous central venous catheter (PCVC). The PICC is made of either silicone (Intrasil) or polyurethane (Intracath). These catheters may be single or double lumen and are generally 2 to 7 Fr in size (1,3). A Hohn PICC has a Dacron cuff, similar to the Broviac and Hickman catheters, which is placed in the subcutaneous tissue and is used to help hold the PICC in place (3). The PCVC is used in neonatal patients, with sizes 1.1, 1.9, and 2.8 Fr. Because of their small size and risk of clot formation, use of the 1.1 and 1.9 Fr PCVC lines for blood sampling or blood transfusions is not recommended (3). Also because of their small size, PCVC lines require a heparin flush every 12 hours (3). Use of the PCVC is limited to the neonatal intensive care unit and therefore will not be discussed here; however, the 2.8 Fr PCVC can be treated in the same way as a small PICC, described below.
Anatomy and Physiology
The basic purpose of using these catheter systems is to have a long-term intravenous line positioned within a central vein with a port that can be readily accessed. The benefits of accessing the central circulation over a peripheral vein include the ability to administer certain antibiotics and chemotherapeutic agents that may cause sclerosis of peripheral veins and the ability to infuse solutions containing higher concentrations of dextrose or potassium than can safely be administered through a peripheral vein. The decision about which type of catheter to use is based on several factors, including the age and
developmental level of patient, the frequency of access that will be required, patient and parent desires, and comfort issues regarding the necessary flushes and dressing changes.
developmental level of patient, the frequency of access that will be required, patient and parent desires, and comfort issues regarding the necessary flushes and dressing changes.
For the partially implanted external catheters, the most common sites include the external jugular, subclavian, and cephalic veins. For the implantable device, the catheter is usually placed in the subclavian vein, although the internal jugular vein also can be used. With both of these types of catheter, the distal tip is positioned at the junction of the superior vena cava and right atrium or within the right atrium (1,2). The PICC and PCVC are inserted in the upper arm through the basilic, brachial, or cephalic vein and passed to the superior vena cava until the tip of the catheter lies at the junction of the superior vena cava and right atrium. Another option for these catheters is insertion in the lower leg through the saphenous vein to the inferior vena cava, with the tip positioned at the junction of the inferior vena cava and right atrium (3,5).
Indications
Children undergo placement of an indwelling line for a variety of reasons, including chronic illnesses requiring long-term intravenous antibiotic therapy (e.g., osteomyelitis, pulmonary infection associated with cystic fibrosis); administration of chemotherapy treatments for childhood cancers; difficult intravenous access in a child who frequently requires blood draws or intravenous medications; and parenteral nutrition for those with conditions such as short-bowel syndrome, malnutrition, and other gastrointestinal or hepatic disorders. In the ED, these lines can be accessed for phlebotomy or administration of fluids, antibiotics and other medications, and blood products. Catheter-related problems that may result in ED visits include catheter occlusion or breakage, unintentional displacement, and skin irritation and/or infection at the site of insertion. Contraindications to access for therapy would include a dislodged catheter, an inability to confirm that a catheter has been placed properly, and a suspicion of significant clot or infection within the catheter that may be dislodged with use.
Equipment
Partially Implantable Catheters (Broviac, Hickman), PICC, and 2.8 Fr PCVC
Sterile gloves (two pairs), mask, gown and eyewear
10% povidone-iodine solution and alcohol or 2% chlorhexidine (for those older than 2 months and not sensitive to this product)
Sterile drapes
10-mL syringe filled with normal saline
Heparin flush
For patients up to 6 months of age, 3 mL heparin (10 U/mL)
For patients over 6 months of age, 5 mL heparin (100 U/mL)
For 2.8 Fr PCVC, 2 mL heparin (10 U/mL)
Note: for the Groshong catheter, 5 mL saline is used to flush the catheter, not heparin
Catheter clamp or hemostat without teeth
Fluids and medications to be administered
Dressing and tape for procedure completion (gauze or transparent dressing such as Opsite or Tegaderm), povidone-iodine ointment
10-mL syringes (2 to 3 empty) if blood drawing is desired
Heparin lock, normal saline flush, and cap
Totally Implanted Devices (Port-A-Cath)
Sterile gloves (two pairs), mask, gown, and eyewear
10% povidone-iodine solution and alcohol or 2% chlorhexidine (for those older than 2 months and not sensitive to this product)
Sterile drapes
10-mL syringe filled with normal saline
Heparin flush
For patients up to 6 months of age, 3 mL heparin (10 U/mL)
For patients over 6 months of age, 5 mL heparin (100 U/mL)
Two noncoring (Huber) needles with a 90-degree bend, using (preferably) the following sizes:
20-gauge for drawing blood
22-gauge for administration of intravenous fluids or medications or 19-gauge for administration of blood
Note: in an emergency, a standard 19-gauge needle can be used
T-extension tubing with side clamp
Several sterile gauze squares (2″ × 2″) to stabilize needle
Tape
Gauze dressing for procedure completion
10-mL syringes (2 to 3 empty) if blood drawing is desired
Additional Equipment Needed for Special Procedures
Dissolving a Clot in the Catheter
Recombinant tissue plasminogen activator (CathFlo, Alteplase), 2 mg
Broken Catheter Repair
Catheter repair kit (Evermed) containing plastic clamps, silicone adhesive, injection caps, and 12 Fr catheter replacement segment (three sizes of catheter repair kits are available, based on the internal diameter of the patient catheter– 0.8, 1.0, and 1.3 mm)
Procedure
Several key points should be made about accessing an indwelling line: (a) a sterile field and sterile technique should be maintained during the entire procedure; (b) acetone or tincture of iodine should not be used on the external catheter, as this can lead to drying or cracking of the catheter (povidone-iodine is acceptable); (c) forceps with teeth should not be used on the external catheter, as these can damage the catheter and cause breakage or make holes; (d) a catheter clamp should always be readily available to access partially implantable devices; (e) only 10-mL syringes should be used to draw fluid or flush the catheter, as smaller syringes generate higher pressure, which can rupture the catheter; (f) heparin flush and parenteral fluids should be ready to administer; (g) fluids should not be administered if no blood return is obtained after the catheter is flushed; and (h) the clinician should infuse 10 mL of saline flush between any medications to flush the catheter, except PCVC lines, for which a 2-mL flush is adequate (1,2,3,5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree