- Thermoregulation
- Skin care on the neonatal intensive care unit
- Optimizing the neonatal environment
- Procedural pain and analgesia
- Developmental care
Introduction
Human newborn babies, especially preterm newborns, are exquisitely vulnerable to the environment around them. They are born at a relatively more immature stage than many mammals and are dependent on immediate warmth and nutrition being provided by their mother. When this is not possible, for example in the context of a sick infant admitted to the neonatal intensive care unit (NICU), it is vital that the environment around the baby is controlled to provide the optimum care and nurture and to avoid causing any harm. The importance of early parental involvement, good positioning, noise reduction and avoiding painful stimuli in facilitating normal development is increasingly being understood. This chapter explores the key issues.
Thermoregulation
Normal Physiology
Full-term infants are able to regulate their own body temperature but less effectively thanolder children or adults. The small for gestational age (SGA) infant, and particularly the preterm infant, has greater problems in maintaining body temperature. After birth, the core and skin temperature of the term newborn can drop at a rate of approximately 0.1 °C and 0.3 °C per minute respectively, unless immediate precautions are taken.
The temperature of an infant will depend on the site at which it is measured. Normal core temperature ranges between 36.7 °C and 37.3 °C, and can be measured by a rectal thermometer; however, this is not routine practice and should usually be avoided. Axillary temperature approximates to core temperature and is the preferred site for recording temperature in newborn babies. Skin temperature is lower than core temperature and is recorded by taping a thermistor to the abdomen. Normal abdominal temperature is 35.5–36.5 °C in a term infant and 36.2–37.2 °C in small premature infants. If the difference between abdominal and peripheral (e.g. toe) temperature is large, then the infant is vasoconstricted to conserve heat (or because he/she is infected or shocked). If the difference is small, the infant may be vasodilated and attempting to lose heat. The World Health Organization classifies a core body temperature for newborns of 36–36.4 °C as mild hypothermia, 32–35.9 °C as moderate and less than 32 °C as severe hypothermia. At these temperatures a special low-reading thermometer will be required to obtain an accurate reading.
Mechanisms of Heat Loss
Heat is lost from the body to the environment in four different ways: conduction, convection, evaporation and radiation. These mechanisms are illustrated in Fig. 24.1 and the ways to minimize their effects in the nursery are described in Table 24.1.
Figure 24.1 Heat loss: (a) by conduction, (b) by convection, (c) by radiation, (d) by evaporation.
From Warren, I. Nursing the Neonate, 2nd Ed. 2010. Wiley Blackwell.
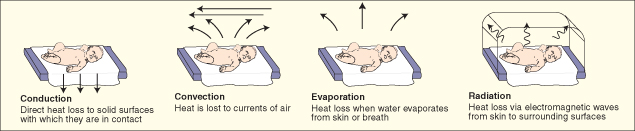
Table 24.1 Mechanisms of heat loss and prevention
| Mechanism | Example | Prevention |
| Conduction | Heat loss into a cold surface directly under the baby. Heat loss into cold(er) equipment | Warm the Resuscitaire towels prior to delivery Discard wet towels Prewarm the incubator Do not place cold radiography plates directly in contact with the baby’s skin Warm hands and stethoscope before examining the baby Kangaroo care – placing baby directly against a parent’s chest |
| Convection | Heat loss directly into currents of air | Place newborn preterm infants in a plastic bag or wrap Do not place the baby near open windows or air vents Use closed incubators rather than open platforms if possible Close the doors to the nursery Close the incubator doors after a procedure |
| Evaporation | Heat lost when water evaporates from the baby’s skin as water vapour Evaporation of water (and therefore heat loss) from the lungs during expiration | Place newborn preterm infants in a plastic bag or wrap Dry newborn term infants immediately with warm, dry towels Humidify the environment (e.g. the incubator) Humidify and warm ventilation gases Cover open tissue (e.g. skin burns or gastroschisis) |
| Radiation | Heat loss (via infrared radiation) to another surface, which is not in contact with the baby or down a concentration gradient via surrounding air | Maintain the whole nursery at a warm temperature Use double-walled incubators Do not come between the baby and an overhead heater Cover the baby’s head (large surface area) with a hat |
Physiological Mechanisms to Conserve Heat
When exposed to cold the normal baby tries to conserve heat by a variety of means:
- Peripheral vasoconstriction.
- Increased heat production through increased basal metabolic rate, increased voluntary muscular activity, involuntary muscular activity – shivering. Shivering is virtually non-existent in preterm infants and their ability to increase muscular activity is limited.
- Non-shivering thermogenesis. Full-term infants are born with a layer of brown fat, mainly around the neck, between the scapulae and along the aorta. Brown fat can be rapidly metabolized to generate heat. This is under the control of the sympathetic nervous system.
Why is the Newborn Prone to Heat Loss?
The newborn is particularly susceptible to heat loss for a number of reasons: see Box 24.1
- Babies have (like all small mammals) a relatively large body surface area to weight ratio. A preterm infant’s limited ability to flex limbs and trunk increases the exposed surface area for heat loss
- Babies have a limited ability to shiver
- Babies (especially preterm and SGA babies) have a lack of subcutaneous fat
- Babies (especially preterm and IUGR babies) have a deficiency of brown fat and reduced glycogen stores
- Babies are born wet (liquor, meconium, blood), predisposing to evaporation
Prevention of Excessive Heat Loss
The ways in which heat loss can be prevented in general are described in Table 24.1. Specific issues are described below.
Labour Ward
The provision of warmth and prevention of heat loss is the first essential step in stabilization of the newborn. It comes before airway and breathing in all resuscitation algorithms. The baby must either be dried completely with a prewarmed, clean towels or (if preterm <32 weeks) be placed, still wet, into a large plastic bag which provides a ‘mini-incubator’ around the baby and prevents evaporative and convective heat loss. The bag must clearly not cover the baby’s head, which should be covered with a hat. Radiant wamers or heated mattresses are used. Heating gel packs can be used for extreme preterm babies.
Figure 24.2 Demonstration of the use of a plastic wrap and hat to aid thermoregulation in the newborn preterm infant. With thanks to Dr Fiona Wood.

For a healthy term newborn skin-to-skin contact immediately after birth is recommended. The infant is thoroughly dried and placed on the mother’s chest and abdomen with a light blanket around them. This reduces radiant and conductive heat loss, promotes temperature stabilization and improve bonding and lactation.
Nursery
Very low birthweight (VLBW) infants do not have a superficial layer of keratin, and consequently water and heat are lost through the permeable skin. Adequate ambient humidity in the incubator prevents this. Infants should be dressed, including a hat, to reduce radiant and convective heat loss whenever possible. Modern incubators provide a thermoneutral humidified environment and have warm air ‘curtains’ that minimize convection currents when doors are opened for procedures.
Closed Versus Open Incubators
Babies are generally provided with a thermoneutral environment by nursing them in either a closed incubator (with doors and ports to allow access) or on a servo-controlled heated platform, with an overhead radiant heater or heated mattress. The thermoneutral temperature is that at which the baby expends least additional energy maintaining body temperature. The thermoneutral range is much narrower in preterm infants than in older children (Fig. 24.3).
Figure 24.3 Thermoneutral temperature range for different birthweight infants. The upper graph represents infants nursed naked and the lower is for clothed babies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


