- Fetal responses during labour
- Fetal and neonatal responses to perinatal asphyxia
- Perinatal asphyxia
- Assessment of the infant at birth
- Stabilization at birth
- Resuscitation
- Postresuscitation care of the asphyxiated infant
Introduction
It is important to remember that the vast majority of babies are born in good condition and do not need any intervention. However, perinatal asphyxia is the most frequent and serious preventable problem for the newborn baby. Severe perinatal asphyxia may lead to a severely ill baby with major long-term sequelae such as mental retardation, cerebral palsy, blindness and epilepsy. Good perinatal care can minimize the risks of hypoxia. Neonatal depression at birth (Apgar score ≤6 at 1 min) occurs in about 14% of all births and is often unpredictable, so all professionals who are present at deliveries should have basic life support skills. Expert help capable of advanced resuscitation must be quickly available. Perinatal asphyxia remains a major source of neonatal morbidity in developed countries, and ranks with perinatal infection as the cause of at least two thirds of neonatal mortality in developing countries. Owing to problems with definition, reported incidences in full-term neonates vary from 2 to 4/1000 live births, even more so for very low birthweight (VLBW) infants, with rates of up to 60%.
Fetal Responses During Labour
Every contraction during normal labour interrupts flow in the uterine arteries and may cause relative hypoxia and hypoperfusion. This can be considered ‘physiological’ hypoxia–ischaemia. During these episodes the fetus deploys various protective mechanisms (Table 5.1). Only if these responses become overwhelmed does the fetus suffer injury. These fetal adaptations are designed to maintain function in vital organs such as the brain and myocardium. They include relative fetal bradycardia during contractions, and the ‘diving seal’ reflex. Transient periods of asphyxia may also induce anaerobic metabolism in the fetal brain and myocardium, with utilization of ketones and lactate as alternate fuels.
Table 5.1 Responses of the normal fetus to transient episodes of ‘asphyxia’ in labour
| Redirection of blood flow towards: | Brain |
| Myocardium | |
| Adrenals | |
| and away from: | Skin |
| Bowel | |
| Muscles | |
| ‘Diving seal reflex’ comprising: | Bradycardia |
| Increased blood pressure | |
| Anaerobic metabolism resulting in metabolic acidosis |
Fetal and Neonatal Responses to Perinatal Asphyxia
Once the normal adaptive mechanisms to perinatal hypoxia have been exhausted, the fetus will show profound but predictable reactions to ongoing hypoxia. These predominantly affect the respiratory and cardiovascular systems and are observed in babies born immediately after an acute intrapartum asphyxial event. However, with a severe insult early in labour or a delayed delivery many of these changes will be taking place in the unborn fetus (see Fig. 5.1). In the most extreme cases this leads to stillbirth, but for most babies adequate resuscitation can restore the infant to a normal physiological state.
Figure 5.1 The physiological effect of acute asphyxia and the response to resuscitation.
(Courtesy of Dr Sam Richmond.)
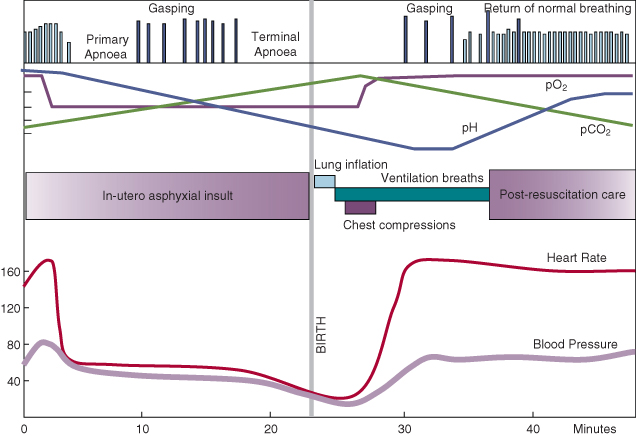
Respiratory Activity
Initially there is increased respiratory activity. When the respiratory centre in the brain becomes hypoxic there is then a period of apnoea (primary apnoea). Secondary respiratory centres in the spinal cord (which are normally inhibited by the brain) then trigger a series of slower gasps, which eventually become less frequent until terminal apnoea occurs. Spontaneous recovery can only occur if the baby is able to breathe through an open airway before terminal apnoea begins. Once terminal apnoea has occurred the baby will die without active resuscitation. The precise interval between a complete asphyxial insult and terminal apnoea in the human fetus is not known as this often occurs before birth, but extrapolation from animal studies and postnatal collapse suggests newborns can withstand 10–15 min of severe asphyxia.
Cardiovascular Activity
Heart rate changes occur simultaneously with the respiratory changes described above. Initially, there is tachycardia, followed by a decline to about 60 bpm. This is probably mediated by vagal stimulation and the heart is able to continue to beat by metabolising myocardial glycogen stores. Central blood pressure is maintained by peripheral vasoconstriction and by increasing stroke volume in response to bradycardia. Transient rises in heart rate and blood pressure occur when spinal gasps develop, but heart rate and blood pressure fall again as apnoea develops. This is due to myocardial anoxia, and without resuscitation the baby will die. The pulmonary vascular resistance increases dramatically with terminal apnoea, and the newborn circulation generally tends to revert to a fetal state. With effective resuscitation the oxygen level in the coronary arteries rises, the heart rate increases and the baby starts to breathe spontaneously (see Fig 5.1).
The interval between asphyxial insult and delivery is variable and the appearance of the newborn will depend on where they are on the ‘physiological graph’ shown in Fig. 5.1. A baby with primary apnoea will appear blue with some tone and reflex activity and the heart rate will be accelerating. The baby will usually recover spontaneously, provided the airway is open. This can be accelerated by physical stimulation.
In contrast, the baby with terminal apnoea will not recover without intervention. In this case the baby is white (vasoconstricted) or intensely cyanosed, unresponsive and flaccid; the heart rate is less than 100 bpm and perfusion is poor.
Unfortunately, in the delivery room we may not know the severity of the asphyxia and we often cannot distinguish between primary and secondary apnoea, so that prompt and effective resuscitation should be commenced in all apnoeic infants. As the baby responds it can usually be determined whether the apnoea was primary or secondary. Babies with primary apnoea have a rapidly accelerating heart rate, and will either show a few gasps or start to breathe normally. In contrast, babies with terminal apnoea will show some initial rise in heart rate in response to ventilation, start to gasp initially and then continue to do so for some time before normal, regular breaths ensue.
Perinatal Asphyxia
Defining Perinatal Asphyxia
It is vital that perinatal asphyxia is defined accurately, both from a clinical perspective, to guide appropriate treatment, and from a medico-legal point of view when establishing causation (see Box 5.1) Most asphyxiated babies will be born in a poor condition with birth depression, but conversely by no means every baby with birth depression has experienced an asphyxial insult. There are many alternative causes of birth depression (see Table 5.2).
- Evidence of birth depression: an Apgar score 0–3 at >5 min
- Evidence of intrapartum anaerobic metabolism:
- Umbilical cord arterial pH <7.0
- Umbilical cord arterial base deficit ≥16 mmol/L
- Umbilical cord arterial pH <7.0
- Neonatal neurological sequelae: early-onset encephalopathy characterized by hypotonia, seizures or coma)
- Evidence of multiorgan system dysfunction in the immediate neonatal period (evidence of hypoxic–ischaemic injury to other organs than the brain, such as the kidneys, heart and liver)
- Absence of an alternative aetiology (see Table 5.2)
Table 5.2 Causes of birth depression other than intrapartum asphyxia
| Cause | Example | Effect |
| Congenital brain malformation | Lissencephaly Polymicrogyria | Encephalopathy, seizures |
| Intracerebral bleeding | Unexpected haemophillia A Severe thrombocytopenia | Respiratory depression Seizures |
| Antenatal cerebral insult | Antenatal cerebral infarction | Cystic parenchymal damage |
| Congenital airway anomaly | Choanal atresia Tracheal agenesis (rare) Pharyngeal cyst | Failure to establish open airway |
| Extreme prematurity | RDS, inadequate respiratory effort | Pulmonary insufficiency |
| Extrinsic lung compression | Pleural effusion, congenital diaphragmatic hernia | Pulmonary insufficiency Pulmonary hypoplasia |
| Oligohydramnios | Potter’s syndrome, Posterior urethral valves PROM before 25 weeks | Pulmonary hypoplasia |
| Cardiac | Congenital heart block | Extreme bradycardia |
| Drugs | Anaesthetics, Opiates (as analgesia) Opiates (substance misuse) MgSO4 | Respiratory depression |
| Infection | Listeria Group B streptococcus Herpes simplex infection | Meningitis Pulmonary hypertension Encephalopathy |
PROM, premature rupture of membranes; RDS, respiratory distress syndrome.
Clinical Evidence of Asphyxia
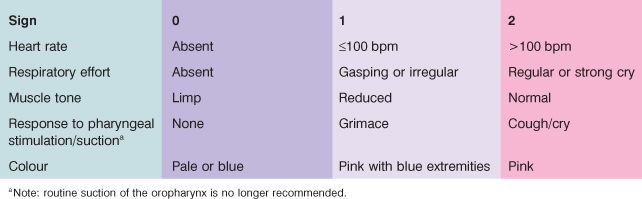
Virginia Apgar introduced the scoring system (see Table 5.3) that now bears her name in an attempt to describe the condition of the infant shortly after birth. Although she did not intend it to refer to asphyxia, it has nevertheless become widely used for that purpose, and in some centres asphyxia is defined (incorrectly) on the basis of a low Apgar score alone. Using an Apgar score of 3 or less at 5 min as the criterion, the incidence of asphyxia is 3–9/1000 full-term infants. If asphyxia is defined as the requirement for intermittent positive-pressure ventilation for more than 1 min, then 5/1000 full-term infants had this condition. If it is defined by hypoxic–ischaemic encephalopathy the rate drops to 1/1000 births.
Table 5.3 The five components of the Apgar score