Visual Impairment in Childhood
David S. Walton
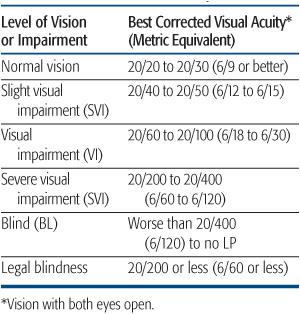
Vision is an essential sensory input from infancy and throughout childhood that allows for normal physical, cognitive, educational, and social development and for adult occupational training. Vision is present at birth at approximately a 20/200 level. Visual acuity develops rapidly during the first year, with normal acuity reached by 9 to 12 months of age. Blindness or visual impairment can be assessed in terms of the level of visual function and by scoring functional vision related to quality-of-life achievements. Assessment of visual acuity is the most often used parameter for estimating vision. The assessment of visual acuity in young children is imprecise. Therefore, it is necessary to define ranges of visual loss. Also test results may improve with advancing age and development. Levels of visual function, ranging from normal to visually impaired, have been categorized into five levels of performance (Table 584-1).
Unsteady eye movements may be evidence of poor vision since birth or with early onset before 2 years of age. When related to an ocular etiology such as cataracts, retinal abnormalities, or optic nerve defects, a pendular nystagmus is often present, which becomes a characteristic jerk nystagmus in lateral gaze. A jerk nystagmus demonstrates a slow-conjugate drift in one direction followed by a rapid-corrective return to fixation. If the vision is very poor, the abnormal eye movements are also conjugate but become more random in many planes and are less sustained. This is sometimes referred to as “wandering eye movements.” In the unique case of neuroblastoma, children may have a very disorganized rapid pattern of eye movements, often brought on by startle stimuli, known as opsoclonus. Infantile sensory nystagmus may be seen with extreme vision loss in only one eye, but in this setting is characteristically only jerk in type. In addition to infantile sensory nystagmus, other causes of nystagmus must be distinguished and include disturbances of motor origin. Congenital motor nystagmus is usually idiopathic but may also be seen as a hereditary disorder found in various Mendelian patterns. It is important to recognize the significance of early onset nystagmus as a key sign of vision loss since infancy. This nystagmus may lessen with visual improvement or with aging.
EPIDEMIOLOGY AND CAUSES OF CHILDHOOD BLINDNESS
It has been estimated that there are 1.5 million blind children worldwide and that 90% live in developing countries. Of the estimated 500,000 children who become blind annually, 60% to 80% are estimated to die within 1 to 2 years.1,2 The reported prevalence rate of blindness and mortality in children under 5 years are directly related. Reported rates of blindness in England and Scandinavia are 0.25/1000 and 0.4/1000, respectively, versus 0.65/1000 and 0.63/1000 in India and Nepal, respectively.3 The number of “blind years” in children worldwide has been estimated to be half the number of “blind years” caused by cataracts in adults.3
Table 584-1. Visual Function Based on Levels of Visual Acuity
The cause of blindness varies greatly between regions, countries, ethnic groups, and level of socioeconomic development. Causes of corneal scarring associated with infections and poor nutrition (eg, vitamin A deficiency) are more frequently seen in underdeveloped countries as compared to the predominance of hereditary disease in closed populations and the greater proportion of retinopathy seen with prematurity, perinatal brain-related abnormalities, and hereditary disease in more affluent populations. Local factors, gender differences, and changing behavior trends can significantly alter the incidence of childhood blindness. It is important to understand that a majority of the causes of childhood blindness are preventable or treatable.
 HEREDITARY CAUSES OF CHILDHOOD BLINDNESS
HEREDITARY CAUSES OF CHILDHOOD BLINDNESS
Bilateral congenital cataracts are often hereditary with autosomal dominant or recessive transmission. Sporadic cases without family history should be considered heritable, and other family members should be screened for evidence of similar cataracts associated with less severe expression. The possibility of related systemic disease should be actively considered, and where indicated, affected children should be carefully examined for evidence of associated anomalies or acquired defects that might suggest an etiology (eg, congenital rubella syndrome).
Hereditary retinal disease causing profound loss of vision should be suspected when the affected eyes appear initially normal in infancy and vision is later lost, although Leber congenital amaurosis, juvenile X-linked retinoschisis, and retinal dysplasia are examples of genetic disorders that can cause blindness at birth. Retinoblastoma neoplasms of the retina may be inherited and heritable. Albinism occurs in all populations and is usually accompanied by an obvious generalized deficiency of pigmentation when compared to family members, although isolated ocular albinism may occur with seemingly normal skin and hair. Childhood glaucoma is responsible for only 5% of childhood blindness but is treatable, so it is possible to preserve significant vision with early treatment.
 PRENATAL AND POSTNATAL CAUSES OF BLINDNESS
PRENATAL AND POSTNATAL CAUSES OF BLINDNESS
In the developing nations of Africa and Asia, blindness in young children secondary to infections and nutritional deficiency (vitamin A deficiency) are the most frequent causes of blindness in very young children. In the United States, cortical visual impairment (CVI), retinopathy of prematurity (ROP), and optic nerve hypoplasia (ONH) are the most prevalent causes.4 The most common etiologies of CVI are perinatal hypoxia (35%), prematurity (29%), hydrocephalus (19%), and central nervous system structural defects (11%).5 Most children with CVI have multiple causes. Minimal improvement in vision may occur after recognition in infancy.5 The potential vision-threatening complications of prenatal infections (eg, rubella, toxoplasmosis), perinatal infections causing ophthalmia neonatorum (eg, gonorrhea, chlamydia), and postnatal infections (eg, herpes keratitis, measles) are tragically seen too frequently in some populations. Many of these infections are preventable or treatable.
 ACQUIRED CAUSES OF BLINDNESS IN LATER CHILDHOOD
ACQUIRED CAUSES OF BLINDNESS IN LATER CHILDHOOD
Most commonly, vision is lost in older children secondary to strabismus amblyopia. Uncorrected refractive errors (eg, high hyperopia, unilateral high myopia) also may be associated with permanent vision loss. Traumatic ocular injury, including nonaccidental injury (child abuse), also becomes more frequent in older children. In addition to the infectious causes of corneal keratitis with opacification, vision loss may be secondary to meningoencephalitis or to hydrocephalus or brain tumor (eg, craniopharyngioma). Permanent visual loss secondary to unrecognized and untreated glaucoma is infrequent but preventable.
PREVENTION OF BLINDNESS IN CHILDREN
A majority of childhood blindness is preventable. That blindness is so prevalent should be considered evidence of our societal failure and should be the stimulus for more effective work for future children. The causes identify the necessary steps to succeed in decreasing the number of blind children. Pediatricians must embrace preventive eye care as an additional and essential responsibility. Prenatal maternal care must continue to work to reduce the incidence of prematurity and the circumstances associated with perinatal hypoxia. Good nutrition and immunizations must become universal. Attention must be paid to the risks and prevention of perinatal ocular infection, and families must be taught the hazards of alternative ocular treatments when known to be clearly hazardous. For example, the practice of using urine as an ophthalmic folk remedy may lead to gonorrhea conjunctivitis and, in turn, permanent corneal scarring or perforation. In addition to the prevention of childhood strabismus amblyopia, the administration of measles immunization, and the provision for dietary vitamin A, what is needed is the continued work of primary medical personnel directed to the goal of preventing blindness. With recognition of eye abnormalities, referral for ophthalmologic care should be always encouraged and rewarded, rather than scrutinized and advised with reservation. Ideally, tertiary centers should be available to provide high-quality care for eyes at risk due to prematurity and to manage corneal injury, cataracts, glaucoma, and ocular injuries.
Lastly, if a child has one eye that is irreparably 20/60 (6/18), then all efforts to protect the good eye must be made, including having the child wear appropriate protective eye wear for sports (eg, goggles, visors, face masks) and full-time glasses with break-proof polycarbonate lenses, even if the child does not need glasses to improve vision. There is evidence that children with one blind eye are more likely to injure their remaining eye. Pediatricians can be instrumental in ensuring that such children are protected.
PROGNOSIS FOR BLIND CHILDREN
In addition to efforts made to reduce blindness in children, care and assistance must also be made for children handicapped by limited vision. This care will require the dedication and work of parents, educators, physicians, and low-vision specialists to allow each child to reach his or her full potential for happiness and for personal development and fulfillment. Worldwide resources available for parents and others to assist with the care of the visually handicapped child and should be utilized.6
Providing service for visually impaired children should begin with a full ophthalmic evaluation at the time a problem is recognized. If the condition is not amenable to treatment, then supportive measures can be instituted even in infancy. For the completely blind child, parents can be trained in the use of alternate sensory stimuli such as sound and touch. Children who have some vision often function normally up to grade 1 or 2, at which point the visual demands begin separating them from their peers. Low-vision evaluation may then lead to training in the use of a wide range of adaptive technology. If a child can see 20/60 (6/18) or better with both eyes open, they will usually be able to function with normal print size. Particular challenges such as glare, depth perception, loss of contrast, and decreased vision in dim illumination may be characteristic of specific disorders, which require adaptations in the classroom and at home. Computers and low-vision optical and video aids enable many partially sighted, low-vision, and blind children to participate in regular class activities. Educational materials are available through large-print books, books on tape, and Braille books.
Students with visual impairments may need additional help with special equipment and modifications in the regular curriculum to emphasize listening skills, communication, orientation and mobility, vocation/career options, and daily living skills. Students who have low vision or who are legally blind may need help using their residual vision more efficiently and may need help working with special aids and materials. Students who have visual impairment combined with other types of disabilities have a greater need for an interdisciplinary approach and may require greater emphasis on self-care and daily living skills.
Schools for the blind concentrate on teaching students how to deal with issues such as maximum use of remaining vision, special technology providing education means (closed-circuit televisions), and practical vocational counseling. These schools must also make an effort to allow contact with sighted peers and to encourage incorporation of the blind child into the sighted society. Only in the most severe cases are interventions such as white canes, dogs, and Braille needed.
Children are remarkably adaptive. Rather than restrict activity and opportunity based on parental perception, visually impaired children should be allowed to flourish within their own comfort level. Long gone are the days of isolating and ostracizing these children who may be otherwise unimpaired. Although schools for the blind/visually impaired and low-vision organizations are extremely useful resources, the ultimate goal should be normalization and broadening of opportunity. Pediatricians must engage families to ensure that vision challenges are being addressed.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


