Viral Infections of the Central Nervous System
John F. Modlin
Viral infections of the central nervous system (CNS) may be variously categorized by type of onset (ie, acute, subacute, recurrent, or chronic), by the level of the CNS involved (ie, brain, brain stem, or spinal cord), and by the viral agent causing disease. The approach to diagnosis and management of CNS viral infection depends greatly on the age, immunization history, and immune status of the patient, and also the epidemiologic setting including season, location, and exposure to viruses that are circulating in the community or transmitted by arthropod vectors.
VIRAL MENINGITIS
ACUTE VIRAL MENINGITIS
 ETIOLOGY
ETIOLOGY
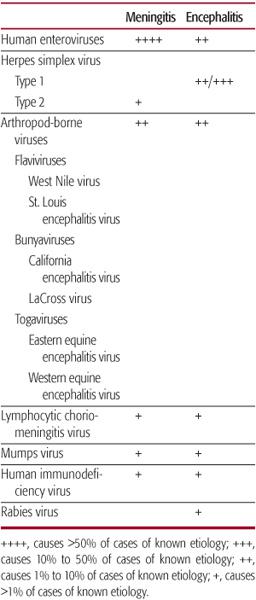
Community-acquired viruses and arthropod-borne viruses are the major causes of the acute “aseptic meningitis” syndrome that, by definition, is accompanied by symptoms and signs of meningeal inflammation in the absence of acute bacterial or fungal meningitis. Although meningitis may occur in the course of infection with many viruses (Table 232-1), the human enteroviruses have been shown to be responsible for the majority of cases of viral meningitis, most prominently the group B enteroviruses, polioviruses, and enterovirus 71. Other well-known causes of viral meningitis include mumps virus, lymphocytic choriomeningitis virus, herpes simplex virus, and the arthropod-borne viruses (including West Nile virus, St. Louis encephalitis virus, La Cross virus, and eastern equine encephalitis virus).
Because enteroviruses cause more than 90% of cases, even during periods of peak arbovirus transmission, the epidemiology of viral meningitis usually reflects the trends of enterovirus infection in the population, including seasonal peaks in late summer and fall and a strong inverse correlation between age and observed rates of disease. Overall rates of enterovirus infection are severalfold higher for infants under 12 months of age than older children. The observed rates of meningitis among children with documented enterovirus infection are highest under 4 months of age when approximately 50% of infants undergoing lumbar puncture in the course of an evaluation for fever will have laboratory evidence of meningitis.1
Mumps virus infection, once a common cause of viral meningitis, is now seen only in locations where mumps virus circulation is not controlled by immunization (see Chapter 318). More than half of cases of clinical are accompanied by cerebrospinal fluid (CSF) pleocytosis, although symptoms and signs of meningeal irritation occur in approximately 5% of patients identified in mumps outbreaks.2
Children acquire lymphocytic choriomeningitis virus (LCMV) infection from exposure to a household environment contaminated by rodent (eg, mouse, rat, hamster) urine. LCMV infection is more common during winter months.
A viral meningitis syndrome caused by herpes simplex virus occurs mainly in adolescents and young adults with primary HSV type 2 genital infection, but it is also reported in young children (see Chapter 309).
 CLINICAL FEATURES AND DIAGNOSTIC EVALUATION
CLINICAL FEATURES AND DIAGNOSTIC EVALUATION
The clinical manifestations of enterovirus meningitis vary with age. For young infants, fever and other nonspecific symptoms may be the only complaints.1,3,4 Older children may first experience a brief prodrome of fever and sore throat followed by headache that is often severe. Signs of meningeal irritation are variable. Complications such as complex seizures, lethargy, coma, and movement disorders that are reported in 5% to 10% of patients with viral meningitis may suggest a more precise diagnosis of meningoencephalitis.4,5 Children with LCMV infection usually present with an influenza-like systemic illness in addition to headache and signs of meningeal irritation.
Table 232–1. Important Causes of Viral Meningitis and Encephalitis in North America
Although the diagnosis of viral meningitis may be suspected from clinical findings, examination of cerebrospinal fluid is necessary when bacterial meningitis must be excluded. The cerebrospinal fluid white blood cell (WBC) count may range from 0 to >1000 WBC/mL in proven cases of viral meningitis. There may be a predominance of neutrophils during the first 1 to 2 days of illness with an inevitable shift to a lymphocyte predominance later.6 In most cases, the cerebrospinal fluid glucose concentration is normal, but values slightly lower than normal are reported in 18% to 33% of cases, and the CSF protein concentration is normal or mildly elevated. Confirmation of the diagnosis of enterovirus infection depends on detection of virus in the cerebrospinal fluid by polymerase chain reaction (PCR) or by virus isolation. For LCMV, diagnosis usually depends on documentation of seroconversion to infection in paired serum samples.
 TREATMENT AND OUTCOME
TREATMENT AND OUTCOME
Patients with viral meningitis may be given analgesics for headache and are often hospitalized in order to receive intravenous antibiotics until bacterial disease can be ruled out with confidence. Pleconaril, an experimental, orally administered antipicornavirus agent, has been shown to reduce the duration of headache and other symptoms in older children and adults with enterovirus meningitis, but this drug is not currently available. There is no specific antiviral therapy for lymphocytic choriomeningitis virus. The symptoms of acute viral meningitis may be more severe and may persist longer in adults compared with young children. Subtle disturbances of motor function such as limitation of passive motion, muscle spasm, and poor coordination may persist for weeks after resolution of the acute illness, but slowly resolve. Despite concern raised by early studies, viral meningitis does not lead to long-term neurologic or cognitive sequelae.7
RECURRENT ASEPTIC MENINGITIS
Recurrent aseptic meningitis (Molleret syndrome) is a rare disease characterized by 3 or more distinct episodes of lymphocytic meningitis of 2 to 5 days duration which are separated by weeks to years.8 HSV-2 has been strongly associated with recurrent meningitis by identification of virus in CSF by PCR, but many patients do not have evidence of genital lesions at the time of presentation. A small number of cases are reported to be caused by HSV-1 and Epstein-Barr virus (EBV), and many have no established etiology. Prophylactic treatment with acyclovir or another anti-HSV drug may suppress recurrent episodes.
ACUTE ENCEPHALITIS
The terms encephalitis, meningoencephalitis, and encephalomyelitis are generally used interchangeably to denote inflammation of the brain, brain stem, and/or spinal cord. National Hospital Discharge Survey data reveal that children under 12 months of age have the highest rate of encephalitis and that males have a slightly higher risk than females.9 There is a general presumption that most acute encephalitis cases are caused by viral infections, although active surveillance studies are able to identify a specific viral etiology for only 9% to 22% of cases, and the cause of approximately 60% of cases cannot be determined.9-11 The list of viruses proven or suspected to cause acute encephalitis is extensive and prominently represented by herpesviruses, enteroviruses, flaviviruses, togaviruses, bunyaviruses, adenoviruses, mumps virus, lymphocytic choriomeningitis virus, human immunodeficiency virus, and rabies virus that all replicate in neural cells causing neuronal destruction and inflammation, primarily in gray matter (Table 232-1).
The terms postinfectious encephalitis and acute demyelinating encephalomyelitis (ADEM) are interchangeably applied to acute central nervous system (CNS) disease that rarely complicates infection with some common viruses, including measles virus, rubella virus, influenza viruses, and other respiratory viruses. Evidence for CNS viral replication is generally lacking, and immunopathologic mechanisms are considered to be responsible for the characteristic perivascular inflammation and demyelination associated with postinfectious encephalitis.
HERPES SIMPLEX VIRUS ENCEPHALITIS
Herpes simplex virus (HSV) causes only 8% to 12% of encephalitis cases of known etiology9-11 but deserves special consideration because HSV is identified in population-based studies as the most common cause of viral encephalitis.9 Unlike other viral infections, the outcome of HSV encephalitis can be improved with prompt and safe antiviral therapy. HSV type 1 (HSV 1) and HSV type 2 (HSV 2) are closely related alpha herpesviruses that share a tropism for muco-cutaneous sites, the ability to establish latency in neural tissues, and the ability to reactivate repeatedly, causing recurrent disease. HSV encephalitis is characterized by inflammation with perivascular lymphocytic cuffing, edema, and hemorrhagic necrosis of affected areas of the CNS.
 CLINICAL FEATURES
CLINICAL FEATURES
Neonates In neonates, HSV encephalitis may occur as isolated CNS disease or may develop in the course of disseminated HSV disease; altogether about half of infants with neonatal HSV infection develop encephalitis. Viremia probably represents the major route of transmission to the CNS during disseminated neonatal HSV infection resulting in diffuse, patchy CNS involvement. In contrast, transport to the brain is likely to occur via peripheral sensory neurons in neonates who present with localized CNS disease. In either case, the absence of preexisting immunity and immature T cell responses permits a high level of virus replication and spread within the immature brain. Both HSV 1 and HSV 2 can be transmitted to the newborn in the perinatal period, but encephalitis occurs more commonly and is more severe with HSV 2 infection. Overall, infants less than 4 weeks of age are at risk, although disseminated HSV infection typically begins within the first 10 days of life, and infants with disease limited to the CNS are more likely to have onset of disease in the second or third week of life.12 Neonates with HSV encephalitis typically present with lethargy, poor feeding, and focal and/or generalized seizures. Motor abnormalities in the form of tremors, paresis, and hypo- or hyperreflexia may be noted on exam.
Infants and Children About one third of HSV encephalitis cases beyond the newborn period occur in children and adolescents with an approximate annual incidence of 2 to 4 per 1,000,000.12 Virtually all are a consequence of sporadic HSV 1 disease that may occur as either primary or recurrent infection. Unlike other herpesviruses, HSV is not associated with a propensity to cause encephalitis in immuno-compromised patients. The hallmark of HSV encephalitis is focal neurological disease that may affect any part of the brain, brain stem, or spinal cord13,14 but most commonly involves one or both temporal lobes. More than 90% of patients present with fever and altered consciousness, and more than two thirds exhibit headache, personality change, dysphagia, and focal or generalized seizure activity. Other common early findings are hemiparesis, memory loss, ataxia, and cranial nerve palsies.
 DIAGNOSTIC EVALUATION
DIAGNOSTIC EVALUATION
The initial evaluation of suspected HSV encephalitis includes brain imaging, electroencephalography (EEG), and CSF examination. Magnetic resonance imaging (MRI) is reported to be more sensitive than computerized tomography (CT) for detection of focal brain lesions. The periodic lateralized epileptiform discharges (PLEDs) demonstrated by EEG represent sensitive but relatively nonspecific evidence of HSV encephalitis. At least 90% of patients will have an abnormal CSF examination with an elevated CSF WBC and elevated protein concentration on presentation.
Confirmation of HSV encephalitis depends on detection of HSV virus in CSF or CNS tissue. Polymerase chain reaction (PCR) detection of viral DNA in CSF is highly sensitive and specific when compared with virus isolation from brain biopsy specimens.15 PCR testing early in the course of HSV encephalitis may produce a false-negative result, but HSV DNA has been shown to persist in CSF in virtually all patients who have repeat lumbar punctures up to 7 days, even when on effective antiviral therapy.15 Infectious virus can also be isolated when brain biopsy is performed 4 or more days after the start of antiviral therapy. HSV is rarely isolated in cell culture from CSF from patients with encephalitis.
 TREATMENT AND OUTCOME
TREATMENT AND OUTCOME
Untreated HSV encephalitis is fatal for more than two thirds of cases, and only about 10% of survivors recover with normal neurological function. Intravenous acyclovir therapy given at a dose of 10 mg/kg q8h for 10 days reduces mortality to approximately 25% and improves the prognosis for survivors.16 A higher acyclovir dose of 20 mg/kg qh8 for 21 days may improve survival for neonates when compared with the standard dose, although this has not been studied in a direct comparative trial.17
Relapse of central nervous system disease with recurrent fever, focal neurologic symptoms, and CSF pleocytosis is reported in 10% to 25% of patients with acute herpes simplex virus (HSV) encephalitis. Relapse occurs within days to months of discontinuation of antiviral therapy and is associated with similar signs and symptoms compared with the initial episode. Although HSV can be recovered from some cases of recurrent disease, the inability to demonstrate the presence of HSV by virus isolation or PCR in many others suggests a second mechanism that may be immunologically mediated.
In addition, long-term studies of infants who have onset of encephalitis in the neonatal period find a high risk of periodically reactive CNS disease with severe adverse neurological sequelae (especially among infants experiencing recurrent herpetic skin lesions) in the first year of life. It is uncertain whether these infants benefit from long-term antiviral prophylaxis beyond the neonatal period (see Chapter 309).
ARTHROPOD-BORNE ENCEPHALITIS
Several families of positive-strand RNA viruses cause acute encephalitis in humans and other mammals following the bite of an infected mosquito or tick, including certain flaviviruses, togaviruses, and bunyaviruses. These taxonomically distinct viruses are often collectively referred to as “arboviruses” due to the common requirement for an arthropod vector, and all exist within diverse ecologic systems that include animal reservoirs in nature. More than 20 arboviruses cause acute encephalitis worldwide; among the most prevalent are Japanese encephalitis virus that is responsible for widespread disease throughout East and Southeast Asia and West Nile virus that has been the predominant cause of arthropod-borne encephalitis in North America during the past decade.
 JAPANESE ENCEPHALITIS VIRUS
JAPANESE ENCEPHALITIS VIRUS
Japanese encephalitis virus, a flavivirus, is responsible for thousands of human encephalitis cases throughout South and Southeast Asia. Culex mosquitoes that breed in marshy environments including rice patties serve to maintain a sylvatic cycle involving water fowl and domestic pigs. The ratio of symptomatic to asymptomatic infections is approximately 1:250 and most illness is mild and self-limited. However, encephalitis cases, which occur mainly among children less than 15 years old, are severe with an estimated mortality of 25% and significant neurological and cognitive sequelae in 30% of survivors. The spectrum of CNS manifestations includes meningismus, altered consciousness, seizures, extrapyramidal signs, and acute motor neuron disease.18
The laboratory diagnosis of Japanese encephalitis virus infection is based on demonstration of specific antibodies in serum or CSF which appear by 7 to 10 days after onset of symptoms. There is no available specific antiviral therapy. Approximately 30% of hospitalized patients die from Japanese encephalitis, and up to 50% of survivors have neurological sequelae.
Although the risk of Japanese encephalitis is low for most travelers to endemic areas, immunization is recommended when there is a high risk of exposure, such as with travel to rural areas during the rainy season when mosquito activity is high. An inactivated vaccine produced in mouse brains (Biken) was licensed in the United States in 1992 for travelers and military personnel. A new cell-culture-grown inactivated vaccine is expected to be available soon.
 WEST NILE VIRUS
WEST NILE VIRUS
West Nile virus (WNV) is a member of the same flavivirus complex as Japanese encephalitis virus and St. Louis encephalitis virus. Human infections with WNV occur widely in Africa, Europe, South Asia, and Australia, but were unknown in the Americas until 1999 when an outbreak occurred in the New York City metropolitan area caused by a virus with close genetic identity to WNV circulating in Israel and elsewhere the Middle East.19 The virus has since spread across the North American continent causing hundreds to thousands of cases each year. In most locations, human disease coincides with a summer–fall sylvatic cycle that includes viral amplification in birds and transmission via Culex species mosquito vectors. Person-to-person spread may occur via transfusion of blood and blood products, organ transplantation, transplacental transmission, and breastfeeding.
Introduction of WNV following a mosquito bite is followed by migration of WNV to regional lymph nodes where viral replication leads to a viremia that seeds many organs including the central nervous system. Approximately 20% of infected persons develop illness that in the majority of patients is limited to fever, malaise, arthralgias, and rash that last for 3 to 10 days. Neurologic disease occurs in a smaller proportion of laboratory-confirmed infections, perhaps 1 in 150, but in a higher percentage of reported cases due to the propensity to test and report cases with serious disease. Children are at lower risk of developing CNS disease than adults, and risk is increased among persons with chronic disease and immunodeficiency, including patients with solid organ transplants and patients with hematological malignancies. West Nile encephalitis may coincide with a number of manifestations indicating different levels of CNS involvement, including seizures, movement disorders (tremor, myoclonus, parkinsonism), optic neuritis, chorioretinitis, cranial nerve palsy, cerebellar ataxia, acute motor neuron disease, radiculopathy, Guillain-Barré syndrome, and demyelinating peripheral neuropathy.
A specific laboratory diagnosis depends on demonstration of either WNV IgM antibodies or RNA in serum or CSF. There is no specific antiviral therapy for WNV infection, and no vaccine is yet available. Full recovery from WNV neuroinvasive disease occurs in less than half of survivors. Long-term sequelae include alterations in cognition, inability to concentrate, and residual muscle weakness.
Recovery from infection is thought to be associated with long-term immunity. As with many other acute viral infections, humoral antibody correlates with protection from disease, and T cell responses are important in the host’s response to infection.
 OTHER NORTH AMERICAN ARTHROPOD-BORNE VIRUS DISEASES
OTHER NORTH AMERICAN ARTHROPOD-BORNE VIRUS DISEASES
California encephalitis virus (CE), eastern equine encephalitis (EEE) virus, western equine encephalitis (WEE) virus, and St. Louis encephalitis (SLE) virus are mosquito-borne viruses that are also important causes of CNS infection. Each of these viruses has a distinct sylvatic cycle, geographic distribution, and spectrum of disease, and each is associated with a high ratio of inapparent infections compared with clinical disease. CE, EEE, and WEE have higher clinical attack rates among children, and SLE virus, like its close relative West Nile virus, is more often observed in adults.
CE virus is a bunyavirus that causes a reported 50 to 100 cases of encephalitis each year in the United States. The La Crosse strain of CE virus which is transmitted from small mammals by tree hole mosquitoes is endemic in Midwest states. In contrast, EEE and WEE viruses are members of the alphavirus genus (family: Togaviridae) which cause sporadic and unpredictable regional outbreaks of human encephalitis when conditions are optimal for breeding of mosquitoes that maintain these viruses in a natural cycle that includes migratory birds. Compared with other causes of arthropod-borne encephalitis, disease due to CE virus is relatively mild, and most children recover from infection with minimal or no neurologic sequelae. In contrast, disease caused by both EEE and WEE viruses is more severe in children with high rates of death and disability among survivors.
Virus-specific IgM antibody is present in the serum and cerebrospinal fluid at the time of presentation for most arthropod-borne virus encephalitis cases. Serologic testing for regionally prevalent arthropod-borne virus diseases is generally available in state and provincial public health laboratories in the United States and Canada. Treatment is limited to supportive measures because no antiviral therapy is available.
POSTINFECTIOUS ENCEPHALITIS
Postinfectious encephalitis (or acute disseminated encephalomyelitis) is an acute, inflammatory brain disease that occurs as a complication of certain respiratory and systemic viral infections and is observed following administration of several vaccines, including smallpox (vaccinia virus) vaccine, rabies vaccine, pertussis vaccine, tetanus toxoid, and influenza vaccine. The pathological features of postinfectious encephalitis are accurately replicated in the experimental allergic encephalomyelitis animal model in which an immune-mediated reaction against myelin protein can be demonstrated.20 Antimyelin basic protein antibodies can be demonstrated in some patients with postinfectious encephalitis, but evidence of viral replication within the CNS is virtually never demonstrated.
Postinfectious encephalitis is estimated to represent about 10% to 15% of acute encephalitis cases in the United States. The current incidence is probably lower than in the past when smallpox vaccines were universally administered and measles, rubella, and varicella infections still affected most children. Abrupt onset of fever, altered mental status, seizures, or focal neurologic signs may occur before, during, or, more commonly, within 3 weeks after a respiratory, gastrointestinal, or rash illness. The inflammatory changes in cerebrospinal fluid do not distinguish postinfectious encephalitis from other causes of acute encephalitis, but contrast-enhanced MRI examination often reveals characteristic white matter abnormalities on T2 and fluid-attenuated inversion recovery (FLAIR) images in white matter, cerebellum, basal ganglia, and brain stem. Although widely used, there is no evidence that steroid treatment is effective. Recovery may occur very slowly, but most patients survive without severe disability. Patients who develop recurrent episodes may ultimately receive a diagnosis of multiple sclerosis.
ACUTE HEMORRHAGIC LEUKOENCEPHALITIS
Acute hemorrhagic leukoencephalitis is a rare form of acute encephalitis of unknown etiology characterized by abrupt onset, a rapid course, and often a fatal outcome. The pathological changes reflect those of postinfectious encephalitis with edema, demyelination, and perivascular inflammation but also include extensive hemorrhagic lesions within white matter. Compared with postinfectious encephalitis, the cerebrospinal fluid findings in acute hemorrhagic encephalitis include a relatively higher white blood cells, predominance of polymorphic leukocytes, and the characteristic presence of red blood cells (RBCs). Because patients with acute hemorrhagic encephalitis are usually treated with high-dose steroid therapy based on anecdotal experience, it is important to rule out herpes simplex virus encephalitis that has many similar clinical features.
ACUTE CEREBELLAR ATAXIA
Acute cerebellar ataxia is a common, distinct clinical entity of young children usually caused by acute cerebellitis without evidence of other serious central nervous system disease. Both direct infection and postinfectious, immunopathologic mechanisms are postulated to occur.21 Acute varicella infection is a prominent cause; other reported coincident infections include enterovirus infection, measles, mumps, rubella, parvovirus, and Epstein-Barr virus.
The typical patient is a toddler or young child who develops a truncal ataxia and a wobbly gait 5 to 10 days after onset of the inciting infectious episode, which may have resolved. More severe cases may be accompanied by nausea, vomiting, nystagmus, dysarthria, or dysmetria, but fever and other signs of CNS disease are rare. Disability is often maximal at onset. Even though symptoms resolve slowly over days to weeks, most children recover completely without residual deficits. The most important task of the pediatrician is to rule out a more serious cause for ataxia.
BRAIN STEM ENCEPHALITIS
Enterovirus 71 possesses a unique ability to invade the ventral brain stem, cerebellum, and spinal cord, producing a spectrum of serious neuromotor syndromes including acute flaccid paralysis of one or more extremities, cranial nerve paresis, tremors, myoclonus, ataxia, and a devastating, often fatal syndrome of acute neurogenic pulmonary edema that may result from destruction of medullary vasomotor and respiratory centers. Although enterovirus 71 infections have occurred worldwide, most cases of brain stem encephalitis have occurred among infants and young children during large outbreaks of enterovirus 71 hand-foot-mouth syndrome in Southeast Asia since 1997.22
MYELITIS
ACUTE VIRAL MYELITIS
Acute viral infection of the spinal cord occurs in two different forms: segmental (or “transverse”) myelitis of a section of the cord producing motor and sensory dysfunction at a level below the involved segment, and disease limited to gray matter producing acute motor neuron disease.
Transverse myelitis in children is most often associated with herpesvirus infection, although evidence for infection with other viruses has been presented, and some cases may be caused by immunopathologic mechanisms.23 Direct infection with HSV1, HSV2, VZV, CMV, and Epstein-Barr virus has been demonstrated by detection of virus in cerebrospinal fluid by virus isolation or by PCR. Acute myelitis has also been observed to occur in association with infections with hepatitis A virus, hepatitis B virus, lymphocytic choriomeningitis virus, measles virus, mumps virus, rubella virus, and adenovirus. HSV is the most common cause of acute transverse myelitis in children, and VZV myelitis is more common in patients who are immunosup-pressed. Transverse myelitis most frequently occurs in the thoracic spinal cord and involves the entire width of the cord within a limited number of segments. Rapid onset of bilateral leg weakness occurs with loss of sensation below the level of the lesion and impairment of bladder and bowel function. CSF pleocytosis is present in most cases. The presence of oligoclonal immunoglobulin bands on CSF protein electrophoresis in a minority of patients may suggest a diagnosis of multiple sclerosis. Contrast-enhanced MRI is a sensitive and specific technique for demonstrating the inflammatory changes and swelling of the involved cord segments. Anti-herpes virus drugs and steroids are often administered without clear evidence of benefit or harm. Recovery is slow and often incomplete with as many as 40% of patients experiencing some permanent disability.
The prototype of acute motor neuron disease is poliomyelitis caused by one of three poliovirus serotypes. However, other viruses cause acute paralysis by the same pathophysiologic mechanism, including enterovirus 71 and other enteroviruses, and flaviviruses including Japanese virus and West Nile virus.24 Illness in children often follows a biphasic course over 5 to 12 days with initial nonspecific symptoms including fever, headache, and (for enteroviruses) sore throat followed by a brief period of improvement. The second phase is heralded by onset of intense myalgia, headache and meningismus, followed by motor weakness that progresses over 1 to 3 days. Paresis may range from mild weakness to complete flaccid paralysis and characteristically involves one or more extremities in an asymmetric manner. Deep tendon reflexes are diminished in the affected extremities, but sensation remains intact. Lumbar puncture reveals a moderate CSF pleocytosis. Magnetic resonance imaging of the spinal cord demonstrates evidence of acute inflammation in the anterior horns, especially in the regions innervating the arms and legs. Acute motor neuron disease must be differentiated from Guillain-Barré syndrome that causes symmetrical paralysis and sensory abnormalities in the absence of fever and meningitis.
VIRUS-ASSOCIATED MYELOPATHY
The human retroviruses human immunodeficiency virus (HIV) and human T-cell lymphotropic virus type I (HTLV-1) are both associated with a chronic, progressive myelopathy that is more common in adults than in children. HIV myelopathy is a complication of advanced acquired immunodeficiency syndrome (AIDS) disease and is often associated with AIDS dementia.25 The pathogenesis is not well understood, but symptoms often improve with institution of effective antiretroviral therapy. HTLV-1-associated myelopathy (which is also known as tropical spastic paraparesis) is common in areas where HTLV-1 is endemic. It is associated with a high serum HTLV-1 viral load and the presence of HTLV-1 infected cells within spinal cord inflammatory lesions. In both HIV and HTLV-1 myelopathy, affected patients develop a slowly progressive spastic paraparesis with urinary dysfunction and lateral corticospinal tract abnormalities.
REFERENCES
See references on DVD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


