Fig. 71.1
Micturating cystourethrogram (MCUG) showing VUR secondary to urethral stricture
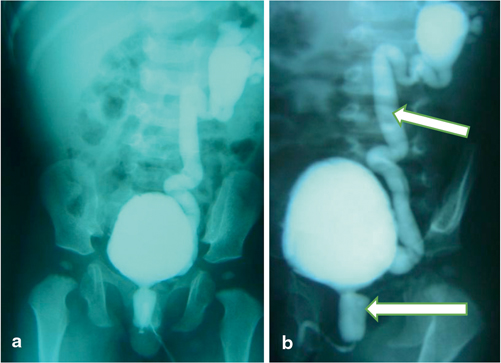
Fig. 71.2
a MCUG in a patient with posterior urethral valve showing unilateral VUR. b MCUG showing severe VUR in a child with posterior urethral valve. Note the dilated posterior urethra
Neurogenic bladder (e.g., myelomeningocele, spinal cord injury)
Detrusor instability and overactive urinary bladder
Classification
The International Reflux Grading system classifies VUR into five grades, depending on the extent of retrograde filling and dilatation of the ureter and renal collecting system. This classification is based on the radiographic appearance during a voiding cystogram, as follows:
Grade I : There is retrograde filling up into the ureter only. The renal pelvis and calyces appear normal (Fig. 71.3).
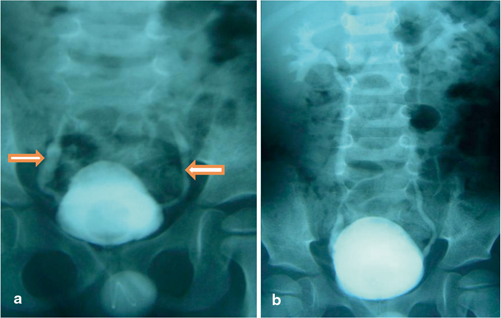
Fig. 71.3
MCUG showing bilateral grade I VUR in (a) and bilateral grade II and III VUR in (b)
Grade II : There is retrograde filling of the ureter, renal pelvis, and calyces. The renal pelvis and calyces appear normal.
Grade III : There is retrograde filling of ureter and collecting system. The ureter and renal pelvis appear mildly dilated, and the calyces are mildly blunted.
Grade IV : There is retrograde filling of the ureter and collecting system. The ureter and renal pelvis appear moderately dilated, and the calyces are moderately blunted.
Grade V : There is retrograde filling of the ureter and collecting system. The renal pelvis is severely dilated, the ureter appears tortuous, and the calyces are severely blunted (Fig. 71.4).
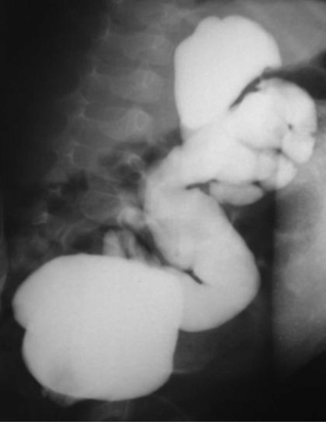
Fig. 71.4
MCUG showing severe grade V VUR
Pathophysiology
VUR results from retrograde flow of urine from the urinary bladder up to the ureter and depending on the severity up into the renal collecting system.
Unrecognized VUR may lead to long-term effects on the kidneys.
This is more so in the presence of concomitant UTI.
VUR leads to increased intrarenal reflux with increased intrarenal pressure and subsequent renal scarring and reflux nephropathy.
This ultimately leads to impaired renal function, proteinuria, and hypertension.
The presence of infection exacerbates the formation of renal fibrosis and scarring.
VUR with intrarenal reflux of sterile urine that is not associated with increased intrapelvic pressures has not been shown to produce clinically significant renal scars.
Sterile reflux however may also produce renal scarring when associated with high intravesical pressures.
Pyelonephritic scarring may, over time, cause serious hypertension due to activation of the renin–angiotensin system.
Renal scarring related to VUR is one of the most common causes of childhood hypertension.
Hypertension develops in 10 % of children with unilateral renal scars and in 18.5 % in those with bilateral renal scars (Fig. 71.5).

Fig. 71.5
MCUG showing sever bilateral VUR
Renal growth is also impaired in those with high grades VUR which if bilateral ultimately leads to impaired renal function and renal failure.
Approximately 4 % of children with VUR progress to end-stage renal failure.
Clinical Features
VUR may be suspected prenatally on ultrasound demonstrating transient dilatation of the upper urinary tract in conjunction with bladder emptying.
Approximately 10 % of neonates diagnosed prenatally with dilatation of the upper urinary tract will be found to have VUR postnatally.
In general, VUR may be asymptomatic and does not cause any specific signs or symptoms unless complicated by UTI .
Older children may more clearly communicate signs and symptoms associated with a UTI (e.g., urgency, frequency, dysuria, incontinence), but, unless the UTI is associated with a fever, there is little reason to suspect VUR .
Investigations and Diagnosis
Urine analysis and culture to rule out UTI .
Blood urea, creatinine, and electrolytes.
Abdominal and pelvic ultrasound.
To evaluate the presence and degree of hydronephrosis and ureter.
A dilated ureter in the presence of hydronephrosis may indicate VUR.
Hydronephrosis with an undilated ureter indicates pelviureteric junction obstruction.
To evaluate the bladder and bladder thickness.
To evaluate the lower urinary tract and bladder function.
Micturating cystourethrogram.
Provides accurate grading of the degree of reflux.
Provides information regarding the urethra, voiding dysfunction and the presence or absence of posterior urethral valves.
Nuclear renal scan.
DMSA
◦ To visualize the renal cortex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


