Background
Residency programs struggle with integrating simulation training into curricula, despite evidence that simulation leads to improved operating room performance and patient outcomes. Currently, there is no standardized laparoscopic training program available for gynecology residents.
Objective
The purpose of this study was to develop and validate a comprehensive ex vivo training curriculum for gynecologic laparoscopy.
Study Design
In a prospective, single-blinded randomized controlled trial (Canadian Task Force Classification I) postgraduate year 1 and 2 gynecology residents were allocated randomly to receive either conventional residency training or an evidence-based laparoscopy curriculum. The 7-week curriculum consisted of cognitive didactic and interactive sessions, low-fidelity box trainer and high-fidelity virtual reality simulator technical skills, and high-fidelity team simulation. The primary outcome measure was the technical procedure score at laparoscopic salpingectomy with the use of the objective structured assessment of laparoscopic salpingectomy tool. Secondary outcome measures related to performance in multiple-choice questions and technical performance at box trainer and virtual reality simulator tasks. A sample size of 10 residents per group was planned (n = 20). Results are reported as medians (interquartile ranges), and data were compared between groups with the Mann-Whitney U , chi-square, and Fisher’s exact tests ( P ≤ .05).
Results
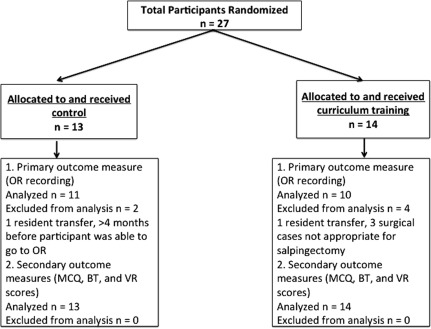
In July 2013, 27 residents were assigned randomly (14 curriculum, 13 conventional). Both groups were similar at baseline. Twenty-one residents (10 curriculum, 11 conventional) completed the surgical procedure-based assessment in the operating room (September to December 2013). Our primary outcome indicated that curriculum-trained residents displayed superior performance at laparoscopic salpingectomy ( P = .043). Secondary outcomes demonstrated that curriculum-trained residents had higher performance scores on the cognitive multiple-choice questions ( P < .001), the nontechnical skills multiple-choice questions ( P = .016), box trainer task time ( P < .001), and all virtual reality simulator parameters.
Conclusion
Participation in a comprehensive simulation-based training curriculum for gynecologic laparoscopy leads to a superior improvement in knowledge and technical performance in the operating room compared with conventional residency training.
Related editorial, page 137 .
There is strong evidence to support the use of simulation in teaching laparoscopic surgery. Simulators allow novice trainees to progress along the early part of the learning curve before entering the operating room (OR). This is important because the learning curve is prolonged for novice and intermediate surgeons. Simulation training has the potential to translate into improved patient safety, decreased OR resources, and better patient outcomes. According to a recent Delphi survey, comprehensive simulation curricula should include cognitive, technical, and nontechnical components. Regulatory bodies have emphasized that the expanding scope of laparoscopy should be coupled with validated training programs that incorporate built-in measures of performance before progression to real procedures.
Training can be time-based, repetition-based, or proficiency-based. The move towards competency-based education in North America has increased the need for objective assessment and predetermined proficiency standards. Studies in the general surgery literature have shown structured proficiency-based training in simulation-enhanced curricula to be superior to conventional residency training, with regards to knowledge and technical skills acquisition. However, this has yet to be demonstrated in gynecology. The aim of this study was to determine whether a comprehensive laparoscopy skills curriculum for gynecology residents translates to improved performance in the OR, compared with conventional residency training.
Materials and Methods
Trial design
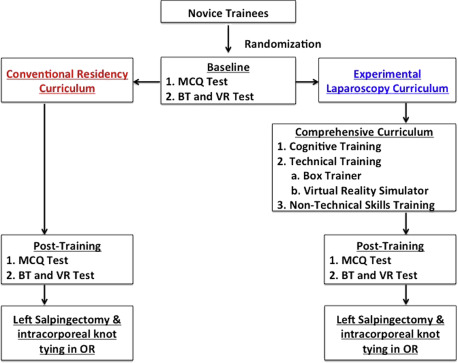
This randomized, single-blinded, 2-armed trial was conducted at a tertiary academic center ( Figures 1 and 2 ). Ethics approval was obtained from St. Michael’s Hospital (12-159C) and University of Toronto (28831) Institutional Review Boards. Written informed consent was obtained from all participants. The study was registered with a clinical trial registry ( clinicaltrials.gov NCT01916343 ).
Participants
All residents who entered their first or second postgraduate year of training in obstetrics and gynecology were invited by e-mail message to participate in June 2013. Residents who had completed >10 laparoscopic salpingectomies as the primary surgeon were excluded from the study. These parameters have been used previously to ensure inclusion of novice trainees with minimal previous experience in the performance of laparoscopic surgery.
Randomization
Residents were allocated the next available number in the concealed sequence of a computer-generated randomization plan with the use of 1-to-1 randomization. Residents were assigned to either the usual residency curriculum (conventional) or the experimental comprehensive curriculum (curriculum). Residents were not blinded to their group because of the nature of the intervention.
Interventions
Conventional training group
Residents in the conventional training group progressed through residency training in the usual fashion. They continued to attend weekly departmental academic half-days, participate in the OR, and partake in rotation-based learning. Rotation-based learning could include rounds, simulation sessions, journal clubs, or other educational activities, depending on the rotation during the study period. There were no learning restrictions during the study period to ensure that their experiences were representative of traditional residency training. All residents have access to a surgical skills laboratory that is open 24/7 at 1 of the major teaching hospitals. Residents in the conventional group were assured that, after study completion, they would receive the same training as the curriculum group to maintain an equal educational experience and encourage study participation.
Curriculum training group
Residents in the curriculum group completed the comprehensive basic laparoscopy curriculum for gynecology residents in addition to conventional residency training. The curriculum was determined with the use of the Delphi consensus method, which is based on work-in-progress data by the same group of authors at the time of study initiation. The curriculum consisted of 4 components: (1) cognitive training, (2) box trainer (BT) technical skills, (3) virtual reality (VR) simulator technical skills, and (4) nontechnical skills. Three-hour sessions took place weekly for 7 weeks in July and August 2013, with an opportunity for make-up sessions.
Cognitive training
The cognitive training component consisted of lectures, self-directed readings, and video-based learning. Residents attended 7 weekly 1-hour lectures that covered the following topics: laparoscopic equipment, electrosurgery, pelvic anatomy, patient selection, medicolegal issues, intraoperative considerations, and complications. All sessions were interactive and facilitated by an expert (E.M.S.) who had advanced training in minimally invasive gynecologic surgery. The final lecture summarized information from the previous 6 weeks and included sequential video-instructed laparoscopic salpingectomy and intracorporeal suturing of the round ligament because video instruction has been associated with faster achievement of proficiency.
Technical skills
BT
A BT curriculum was developed that was based on a previous study. Residents were paired to allow practice with manual skills and camera navigation. Residents rotated through 7 stations (peg transfer, pattern cutting, pretied knot, ovarian cystectomy, intracorporeal knot tying, extracorporeal knot tying, and Roeder knots). Attention was directed to specific skills on a weekly basis and reflected the resident’s individual training needs. Expected time limits were based on the definitions by Ritter and Scott of proficiency in fundamentals of laparoscopic surgery (FLS) tasks. There were 7 weekly 2-hour BT and VR skills practice sessions. Three content experts (E.M.S., H.H., L.S.) supervised all training sessions and provided individualized constructive feedback. All repetitions were recorded to monitor progress towards preset proficiency benchmarks.
VR
Before initiation of the study, a proficiency-based VR simulator curriculum for basic laparoscopic skills was established and included expert-derived benchmarks for each task at basic, intermediate, and advanced levels. The included tasks were camera navigation, instrument navigation, coordination, grasping, lifting and grasping, and cutting.
The recorded time and the instrument movements (left and right instrument angular path and path length) for each task at each level were included, because these parameters have been shown to display construct validity. Study participants practiced the tasks in any order but did not practice for >45 minutes at a time or continue the same task at the same level if they failed > 3 times in a row.
Nontechnical skills
Residents were paired and participated in a high-fidelity OR simulation of a carbon dioxide embolus during a laparoscopic procedure (10-15 minutes). Simulations were conducted in a fully equipped simulated OR. Scripted confederates played the roles of anesthesiologist and scrub technician. A human patient simulator was used with palpable pulses and audible breath sounds (SimMan; Laerdal Medical, Stavanger, Norway) whose vital signs (eg, heart rate, blood pressure, pulse oximeter) were controlled in an adjacent control room. At the conclusion of the simulation, residents underwent a debriefing session and participated in an interactive seminar with a content expert (N.J.D.). The topics that were covered in the seminar included elements of effective teamwork, specifically closed-loop communication and shared mental models, situation awareness, adverse events in healthcare and error prevention using briefing and checklists, decision-making strategies, and management of acute stress.
Primary outcome measure: intraoperative performance
To assess the impact of the experimental curriculum on cognitive skill, technical skill, and nontechnical skill acquisition, all participants performed a laparoscopic right salpingectomy and intracorporeal knot tying of the left round ligament (or proximal end of fallopian tube in the case of bilateral salpingectomies) on a human patient. A complete knot was defined as a double throw followed by 2 single throws performed in <10 minutes. A faculty member assisted the resident in the usual fashion, which included verbal direction and takeover as required. The faculty members were blinded to the randomization of the residents. The complete operation was video-recorded with the laparoscopic camera. As such, no identifying data of the patient or the operating team was recorded; sound was not recorded. One member of the study team (E.M.S., H.H., L.S.) was present during each of the cases to facilitate the recording and record take-overs by the faculty member. The videos were reviewed by an experienced video assessor (C.D.M.), who was blinded to the residents’ randomization, who used the objective structured assessment of laparoscopic salpingectomy (OSA-LS) for the salpingectomy component and a global rating scale and FLS cut-off times for the intracorporeal knot-tying component. All surgeries were scheduled within a 4-month period (September–December 2013) of the conclusion of the curriculum. Informed consent was obtained from all patients.
Secondary outcome measures
Demographic information and laparoscopic experience at the beginning of the study were collected through a questionnaire. Residents in the conventional and curriculum groups underwent baseline and final assessments of cognitive knowledge, technical skills, and nontechnical skills. Final assessments were completed within 10 weeks of the baseline assessment (August and September 2013).
Cognitive knowledge assessment
The cognitive knowledge assessment consisted of 2 different 10-point multiple-choice question (MCQ) tests that pertained to gynecologic laparoscopy.
Technical skills assessment
The technical skills assessment consisted of performance of a laparoscopic intracorporeal knot with the use of a BT and completion of 2 basic skills ([1] cutting and [2] lifting and grasping) on the VR simulator (LapSim; Surgical Science, Gothenburg, Sweden). All participants were oriented to these tasks by a video demonstration of the tasks.
Intracorporeal suturing was chosen because it is 1 of the most difficult skills to master in laparoscopy.
Nontechnical skills assessment
The nontechnical skills assessment included 2 different 14-point MCQ tests that focused on aspects of communication, surgical briefing, and teamwork. Residents also completed the Team-STEPPS (Strategy and Tools to Enhance Performance and Patient Safety) Team Attitudes Questionnaire. In addition, preoperative nontechnical skills were recorded by 1 of the members of the study team (E.M.S., H.H., or L.S.). The risk of bias because of lack of blinding of the study team members was reduced by the use of a checklist that allowed for a relatively standardized and objective assessment of performance ( Appendix ).
Sample size
The power calculation was based on a previous validation study of the procedure-specific scale of the OSA-LS. This study showed a difference of 10 points between novice laparoscopists and intermediate experienced laparoscopists. For a predefined alpha score of .05 and a power of 0.8, the sample size for a 2-sided test was calculated as 10 in each treatment arm. To account for drop-outs, 12 residents were recruited for each arm, which is also the number of residents enrolled in the first and second year of the residency program at the first author’s institution.
Data analysis
Data were analyzed with the use of modified intention-to-treat, as a result of drop-outs because of inability to complete the surgical procedure. Descriptive statistics were calculated for all survey items. Q-Q plots were used to assess for normal distribution. Nonparametric data were reported as median (interquartile range) and were analyzed with the use of the Mann-Whitney U test for between-group comparison. Chi-squared analysis and Fischer Exact tests were used to analyze the difference in categoric data between groups. The level of significance for a 2-sided test was defined as α = .05. Subgroup analysis was performed for the residents who were able to tie an intracorporeal knot in the OR. All statistical analyses were performed using SPSS statistical software (version 22; IBM, Armonk, NY).
Results
Initial assessment
At the initiation of the study, demographic data and laparoscopic experience data were similar between groups ( Table 1 ). Groups were similar with respect to previous FLS training, animal laboratory training, VR simulator training, and team training (Advanced Cardiac Life Support, Advanced Trauma Life Support, Neonatal Resuscitation Program). There were no differences between groups with respect to their baseline testing MCQs, Team-STEPPS Team Attitudes Questionnaire, intracorporeal knot-tying times, or time and economy and movement parameters on the VR tasks ( Table 2 ).
| Characteristic | Conventional (n = 13) | Curriculum (n = 14) | P value |
|---|---|---|---|
| Age, y a | 27 (25–29) | 29 (25.5–31.25) | .583 |
| Gender—male:female b | 2:11 | 1:13 | .596 |
| Postgraduate year level—PGY1:PGY2 b | 6:7 | 6:8 | 1.000 |
| Handedness—right:left b | 12:1 | 14:0 | .481 |
| Musical ability—yes:no b | 5:8 | 7:7 | .704 |
| Video gaming ability—yes:no b | 3:10 | 1:13 | .326 |
| Box trainer experience—yes:no b | 5:8 | 8:6 | .449 |
| Virtual reality experience—yes:no b | 2:11 | 2:12 | 1.000 |
| Comfort performing laparoscopic salpingectomy—yes:no b | 0:13 | 0:14 | 1.000 |
| Salpingectomies baseline, n a | 0 (0-2) | 0 (0-0) | .094 |
| Basic laparoscopic surgeries performed, n a | 0 (0-8) | 0 (0-0.5) | .302 |
| Basic laparoscopic surgeries assisted, n a | 1 (0-10) | 4.5 (1.5-9.25) | .519 |
| Intermediate laparoscopic surgeries performed, n a | 0 (0-0.5) | 0 (0-0) | .325 |
| Intermediate laparoscopic surgeries assisted, n a | 0 (0-4) | 2 (0-3.75) | .583 |
| Advanced laparoscopic surgeries performed, n a | 0 (0-0) | 0 (0-0) | 1.000 |
| Advanced laparoscopic surgeries assisted, n a | 9 (0-2) | 0 (0-2) | .981 |
a Continuous data summarized as median values (interquartile range) and compared between groups with the use of the Student t test or Mann-Whitney U tests
b Categoric data summarized as numbers (n) and compared between groups with the use of the chi-squared test.
| Assessment | Training a | P value | |
|---|---|---|---|
| Conventional | Curriculum | ||
| Multiple-choice question | |||
| Laparoscopy | 7 (6–8) | 6 (5–7) | .054 |
| Nontechnical | 9 (8.5–11) | 8.5 (7–10) | .202 |
| Team-STEPPS questionnaire | |||
| Team structure | 25 (23.5–26.5) | 24.5 (23.75–26) | .458 |
| Team leadership | 28 (25–29) | 27 (24.75–28.5) | .650 |
| Situation | 24 (24–27) | 25 (24–27) | .720 |
| Support | 26 (24–27.5) | 25 (24–27) | .905 |
| Communication | 20 (19–22) | 20 (19–22) | .650 |
| Intracorporeal knot tying (box trainer), s | 600 (398–600) | 600 (497.5–600) | .756 |
| Lifting and grasping (virtual reality) a | |||
| Median time, s | 200 (148–241) | 190 (145–234) | .728 |
| Median path length, m | 3.69 (2.66–5.38) | 2.95 (2.59–4.63) | .538 |
| Median angular path length, degree a | 921 (638–1263) | 703 (643–1084) | .503 |
| Cutting (virtual reality) | |||
| Median time, s | 138 (113–193) | 152 (123–183) | .550 |
| Median path length, m | 1.84 (1.11–2.89) | 1.84 (1.41–2.09) | 1.000 |
| Median angular path length, degree | 427 (259–641) | 434 (334–507) | .867 |
a Continuous data summarized as median values (interquartile range) and compared between groups with the use of the Student t test or Mann-Whitney U test.
Intervention
Time to reach proficiency in the VR and BT portions of the curriculum
All residents in the curriculum group demonstrated improvement in VR and BT tasks. Twelve residents missed at least 1 session, with a mean of 1.3 sessions (8 residents missed 1 session, 3 residents missed 2 sessions, and 1 resident missed 4 sessions). At the end of the intervention, 10 residents (71%) passed all basic VR tasks; 8 residents (57%) passed all intermediate VR tasks, and 1 resident (7%) passed all advanced VR tasks ( Table 3 ). Pass rates of the BT component can be seen in Table 4 . Information was not collected on the amount of time dedicated to simulation practice outside of the study sessions or regular resident teaching for either group.
| Variable | Curriculum, n (%) a | ||
|---|---|---|---|
| Basic (n = 14) | Intermediate (n = 14) | Advanced (n = 14) | |
| Camera navigation | 14 (100) | 11 (79) | 4 (29) |
| Instrument navigation | 14 (100) | 9 (64) | 3 (21) |
| Coordination | 14 (100) | 9 (64) | 5 (36) |
| Grasping | 12 (86) | 10 (71) | 6 (43) |
| Cutting | 13 (93) | 9 (64) | 4 (29) |
| Lifting and grasping | 12 (86) | 9 (64) | 7 (50) |
a Categoric data summarized as total number of residents (n) and frequency (%).
| Task | Goal, s | Pass rate, n (%) a | Best time, s b | Trials, n a |
|---|---|---|---|---|
| Peg transfer | 48 | 0 | 88 (67–105) | 9 (6–13) |
| Pattern cutting | 93 | 4 (29%) | 165 (94–211) | 5 (4–9) |
| Ligating loop | 53 | 0 | 88 (65–111) | 3 (2–4) |
| Extracorporeal knot tying | 136 | 3 (30%) c | 147 (124–175) | 1.5 (0–2) |
| Intracorporeal knot tying | 112 | 5 (36%) | 140 (111–166) | 12 (9–13) |
a Categoric data summarized as total number of residents (n), frequency (%), and range (n)
b Continuous data summarized as median values (range)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


