Fig. 22.1
Obstructive longitudinal vaginal septum (LVS)
Type 3 with a complete vaginal obstruction but with a laterally communicating double uterus (Fig. 22.2).
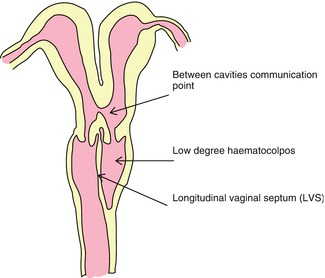
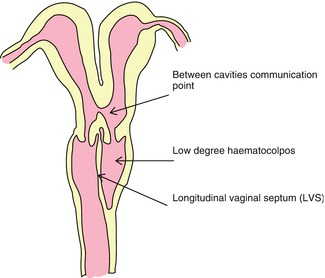
Fig. 22.2
Longitudinal vaginal septum (LVS) with communicating uterine cavities
Types 1 and 3 have similar clinical symptoms with regular menses, dysmenorrhoea, lower pelvic pain, paravaginal mass. Type 2 patients characterized by occasional intermenstual bleedings, dysmenorrhoea and lower pelvic pain, and excessive foul mucopurulent vaginal discharge [16].
Operation of the Obstructed Hemi-vagina
The treatment of choice is surgery and by vaginal approach. Resection of the septum and opening of the hemi–vagina can treat successfully 84–87 % of the patients [5, 7]. The target should be one curative operation rather than a sequence of operations. Usually the results of the surgery are excellent and retraction of the septal pedicles is almost complete. Prophylactic antibiotics administrated before initiation of the operation. Once the vaginal pouch is excised and open, suction and lavage evacuate the entrapped blood and mucous. About 10 % of the patients will need a second operation due to reclosure of the hemi-vagina or due to vaginal stricture. When the septum is thick the operation can be difficult with unsatisfactory results. Complications such as post-operative haemorrhage and a partially successful or unsuccessful operation may occur. Small incision or inadequate opening of the blind septum may result in ascending infection and hemi-vagina abscess and septicaemia hence skilful surgeons should operate these cases.
Attention to leave a generous vaginal pedicle during resection and avoid unnecessary suturing. Sutures are placed only to secure slippage of the tissue. Keep in mind that remained pedicles retract during healing, decreasing the risk of post operative vaginal stenosis. Post operative vaginal mould is not always necessary but frequent follow ups are helpful to control post operative results. In cases of pyocolpos or severe haematocolpos distention and stretching of the septal tissue increases the risk of inadequate resection and possible post operative vaginal stenosis. Haddad et al. recommended for difficult cases, two step surgery small septum resection of 3 cm to allow adequate drainage and after 1 month to remove any remaining septum [7]. Behind the obstruction is mucous-lined vaginal epithelium and cervical type glandular crypts that progressively transform to mature squamous epithelium, hence increased vaginal secretions will continue until cell maturation [17]. Uterine reconstruction is not indicated for cases with type 3, lateral communication of the uterine horns. Some authors have reported the use of hemi-hysterectomy in patients with a high thick walled obstruction, severe forms of pelvic endometriosis or adenomyosis however this approach is not recommended for young patients.
Formation of Transverse Vaginal Septae (TVS)
Incomplete vertical fusion between the Müllerian duct component of the vagina and the urogenital sinus component forms a transverse vaginal septum that varies in both the level and thickness. The incidence estimated to be 1 in 2,100 to 1 in 72,000, while this phenomenon is unclear. Probably is one of the rarest anomalies of the female genital tract but it is much less common than congenital absence of the vagina and uterus [13]. Like imperforate hymen the transverse vaginal septum is not associated with Müllerian malformations [1]. The TVS is associated with imperforate anus and bicornuate uterus and very few urologic anomalies [18]. Most cases are suspected to have a genetic background indicating a female sex-limited autosomal recessive transmission [14] and associated with other congenital anomalies such as coarctation of the aorta, atrial septal defect and malformations of the lumbar spine. Scrutinized family history and physical examination of each patient are mandatory [4]. Transverse vaginal septa (TVS) may be complete or incomplete and found 46 % in upper vagina, 40 % in midvagina and 14 % in lower vagina [19–21] (Table 22.1) (Fig. 22.3). Septa found in the upper vagina and closer to the cervix are usually thicker and most of the times are over 1 cm in thickness [2, 15]. Patients with mid and lower vaginal septa, perineal bulging and a pelvic mass along with a cervix and uterus might be detected during gynaecological examination [1]. Higher the position of the septum in the vagina higher is the risk of presence and extension of pelvic endometriosis, infertility and miscarriage rates. These results probably are explained by the fact that patients with high TVS experience retrograde menstrual blood flow via endometrial cavity and fallopian tubes in much younger age and for a long time [17] (Table 22.1).
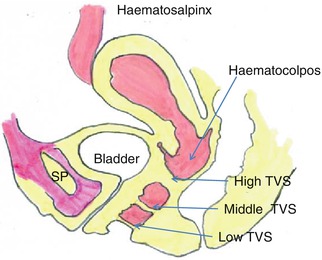
Table 22.1
Frequency of TVS according to vaginal height
Position of the TVS | Lower vagina (%) | Mid vagina (%) | Upper vagina (%) |
|---|---|---|---|
Lodi et al. [20] | 14 | 40 | 46 |
Rock Zakur [21] | 19 | 35 | 46 |
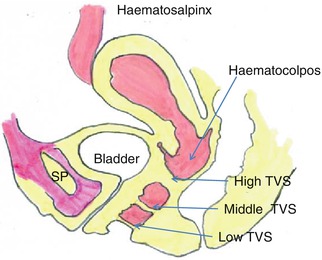
Fig. 22.3
Present the locations of the transverse vaginal septa (TVS)
TVS in Infancy
Neonates with TVS are at risk due to higher morbidity and mortality since formation of a large mucocelle above the septum may compress the ureters, rectum and vena cava. The lower surface of the septum is covered with glandular epithelium which under the influence of the maternal estrogens secretes mucous. The fluid collected might be enormous but the flexibility of the vagina may allow its asymptomatic distention upto a year after birth [22]. When the septum is formed higher in the vagina and closer to the cervix, perineum bulging is absent and hydrocolpos develops towards the upper vagina and beyond. Long standing compression may lead to urethro-vaginal and other urinary tract system fistulas [2]. Clinical examination, image and endoscopic investigation usually demonstrate a large pelvic and lower abdominal mass as a result of the distended vaginal septum. The bladder is displaced anteriorly while hydroureters and hydronephrosis are prominent. Severe compression to the gastrointestinal tract and indirectly to the diaphragms respiratory movements, inevitably lead to respiratory distress and to an emergency operation to save the life of the neonate. The septum should be operated trans perineally and close post operative follow up for short and long term sequellae is advised [22]. Surgery under these difficult and complex conditions endanger high recurrence rate of vaginal stenosis and urinary tract obstruction while vaginal reconstruction might be required later in life [5]. In general TVS excision prior to puberty is associated with a high rate of vaginal stenosis, demanding another operation in adolescence to improve coitus and ease menstruation flow [5, 14].
TVS in Puberty and Adolescence
History at the time of puberty with increasing cyclical abdominal pain in the absence of menstruation is highly suspicious for TVS and diagnosis may be missed for several months. In adolescent girls already by their first few menstruations blood is collected above the septum and haematocolpos is formed. Usually adolescents with TVS present in the emergency room with acute abdominal pain and/or urinary retention. Clinical symptoms are cyclic pelvic pains, development of a central abdominal or pelvic mass and primary amenorrhoea while the incidence of endometriosis is high. The mass is tender to palpation and sonography confirms the presence of a haematocolpos and a haematometra. A haematosalpinx may be detected and even more rarely an endometrioma. Clinical examination of a low and middle TVS will probably reveal a ‘pink’ bulging membrane while in case of an imperorated hymen the bulging membrane is dark bluish. Occasionally a small spontaneous crack of the septum allows menstrual blood partial evacuation and symptoms are then variable [23]. Patients that already tried to have intercourse complain of very short vagina, difficult coitus and place a tampon. In case of a fistula between bladder and upper vagina cyclic haematuria might be observed. Non obstructing transverse septa that will eventually allow a pregnancy, severe dystocia is expected during labour. Gynaecological examination when is possible, vaginoscopy, rectal and abdominal sonography can help to obtain the correct diagnosis. Magnetic resonance image can measure the thickness of the septum and detect pelvic mass and other associated malformations [9, 22].
Surgical Treatment of the TVS
Once the diagnosis of TVS is established both in asymptomatic and symptomatic pubertal girls, vaginoplasty is indicated. Surgery will allow natural menarche and alleviate dysmenorrhoea, will prevent pelvic mass formation and endometriosis. It has been reported that many patients psychologically may feel better to delay definitive surgical therapy once diagnosis has been established however, this is possible only in asyptomatic children below age of 10 [14, 19, 24]. Vaginoplasty for TVS demonstrated high rate of post operative vaginal strictures because of the absence of large vaginal segment and poor motivation of the pubertal patients to perform frequent vaginal dilatation after the operation.
Surgery is the only treatment for a TVS and is relatively easy when the septum is thin and found in lower vagina. The principle of the TVS surgery is to excise the septum and reconnect the vagina by end-to-end anastomosis between the upper and lower vaginal parts. A transverse incision in the centre of the vault of the lower short vagina leads into the upper vagina and haematocolpos is exposed. Using a vaginal speculum will facilitate progress within the vaginal space while presence of areolar tissue may create some uncertainty to anatomical structures and disorientation. Simultaneous bi-digital vaginal and rectal examination, palpating the urine catheter on the anterior vaginal wall will guide the direction of dissection. Lateral dissection permits complete excision of the septum. When the septum is low then the upper vaginal wall is brought easily to oppose the lower vaginal segment and leaving a neo-vagina with normal calibre. Some surgeons at the site of the anastomosis place a firm vaginal mould for 10 days after the operation to reduce the risk of ring stenosis. In addition, cases with lower and middle transverse septal defects and the use of vaginal dilators for 2–3 months subsequent to the removal of the mould, increase the chances for excellent functional vagina in the future [25]. The post operative satisfactory sexual function success rate after TVS obstruction vaginoplasty has been reported as 100 % (27/27) for the lower TVS, 45 % (12/27) for the mid TVS and 41 % (11/27) for high TVS [25]. The major post operative problems of these patients remain vaginal stenosis, dyspareunia and infertility. The pregnancy success rate reported, after septectomy of a low TVS was 100 %, mid TVS 40 % and for the high TVS was only 20 % [23]. Most probably the high incidence of endometriosis especially found in patients with the high TVS explains the high dyspareunia and infertility rates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


