Use of aEEG/NIRS
AMPLITUDE-INTEGRATED ELECTROENCEPHALOGRAPHY
What Is Amplitude-Integrated Electroencephalography?
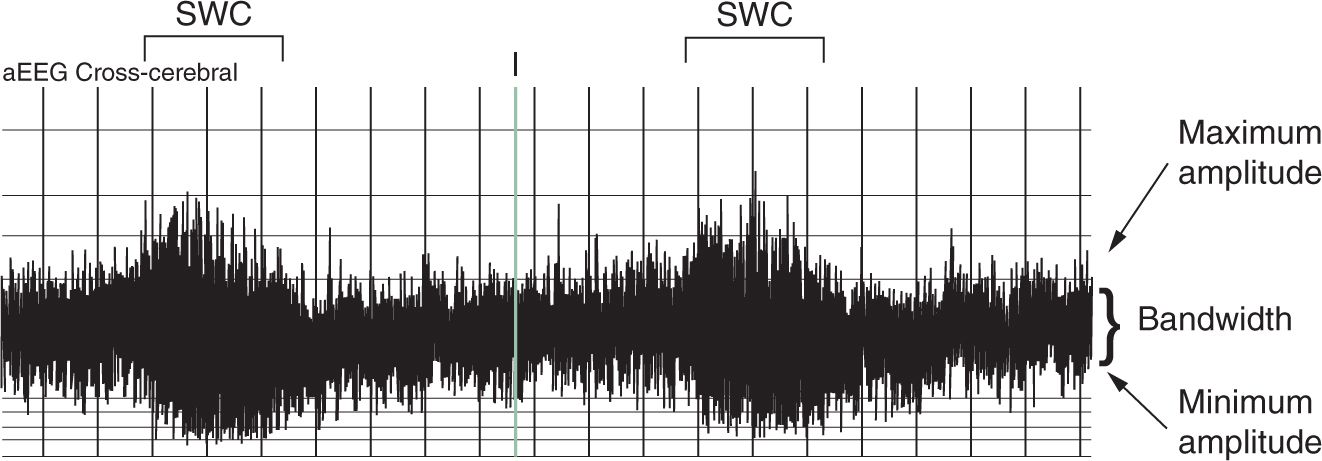
Amplitude-integrated electroencephalography (aEEG) is a simplified, bedside EEG device used to continuously monitor brain function. Brain wave activity is recorded from scalp electrodes, and the raw EEG data are processed using a filter to attenuate frequencies less than 2 Hz and greater than 15 Hz, transform the amplitudes into a rectified and time-compressed signal, and display on a semilogarithmic scale in microvolts (µV). This results in patterns that are easily recognizable without formal training in EEG analysis. Interpretation of the aEEG recording includes assessment of the minimum amplitude, maximum amplitude, bandwidth, and the presence of sleep-wake cycles (SWCs) (Figure 78-1).
FIGURE 78-1 Determination of the presence of sleep-wake cycles (SWCs). aEEG, amplitude-integrated electroencephalogram.
Indications for aEEG Monitoring
The following are indications for aEEG monitoring:
1. Confirmation of suspected clinical seizures, especially when formal EEG is not available
2. Assessment for subclinical seizures in high-risk infants
3. Continuous monitoring of therapeutic effects of antiepileptic medication
4. Prediction of outcomes in hypoxic ischemic encephalopathy (HIE)
5. Other potential, but not well-studied, uses for aEEG include metabolic encephalopathy, patients on extracorporeal membrane oxygenation (ECMO), assessment of neuromaturation in preterm infants, assessment of posthemorrhagic hydrocephalus, surgical anesthesia, and postoperative recovery
Placement of aEEG
1. Types of electrodes
a. Hydrogel: disposable electrodes similar to regular electrocardiographic (ECG) electrodes; used in most commercial aEEG devices
b. Cup-disk: reusable; requires EEG conductive paste
c. Needle: minimal skin preparation required and achieves low impedances; invasive, with theoretical risk for infection
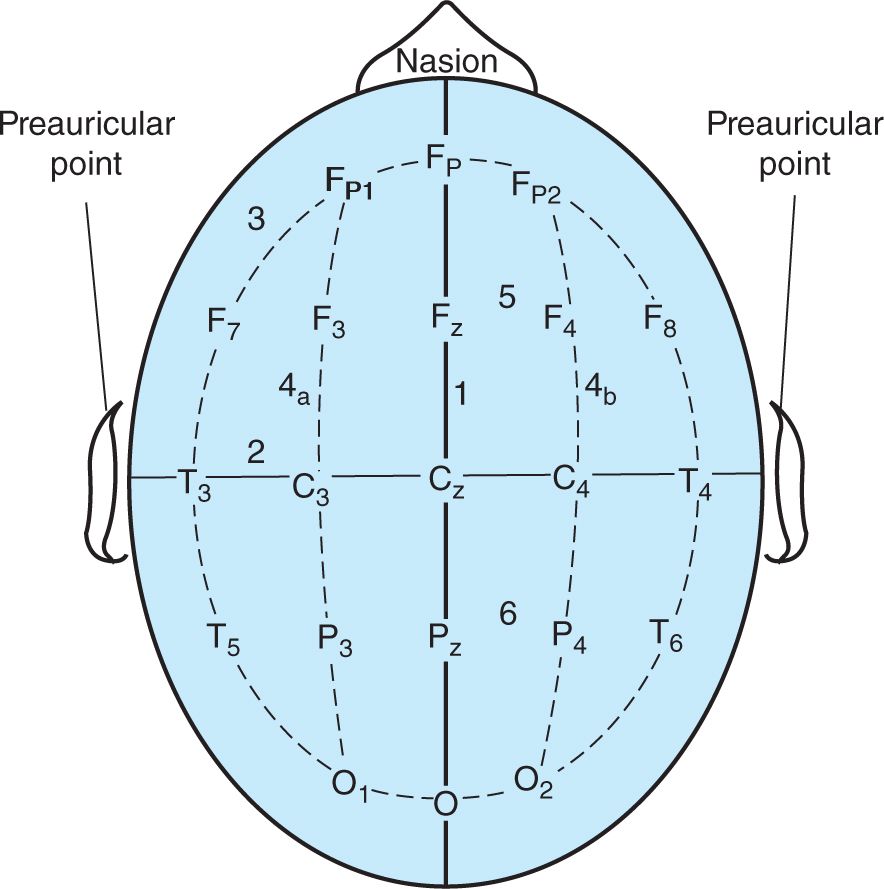
2. Recording montages: location of electrodes based on the 10–20 international classification system modified for neonates (Figure 78-2)
a. Single channel: Traditionally, electrodes are positioned at P3 and P4, which is the area overlying the cortical watershed zone in infants with HIE; alternatively, if using the CoolCap® System, electrodes may be modified to Fp1 and Fp2.
b. Three channel: Electrodes positioned at C3, P3, C4, P4 create two biparietal channels (C3-P3, C4-P4) and a cross-cerebral channel (P3-P4).
c. All devices require an additional ground electrode, usually placed on the back or forehead. Some devices may also require a reference electrode on the scalp (typically Cz).
d. Other EEG recording systems may utilize additional channels.
3. Skin preparation: When cup-disk or hydrogel electrodes are used, skin should be cleaned and exfoliated prior to application.
4. Data quality: Impedance is continuously measured during the aEEG recording. Impedances greater than 10 kΩ indicate poor electrode contact, insufficient skin preparation, or electrical interference, and the electrodes should be checked.
FIGURE 78-2 One-channel amplitude-integrated electroencephalogram (aEEG) typically utilizes the P3-P4 channel. Three-channel aEEG utilizes electrodes at C3, C4, P3, and P4 to create a right-side channel (C4-P4), a left-side channel (C3-P3), and a cross-cerebral channel (P3-P4).
Interpretation of aEEG Recordings
1. Background pattern interpretation
a. Basic background pattern descriptions (Figure 78-3)
(1) Continuous: minimum amplitude greater than 5 µV and maximum amplitude greater than 10 to 25 µV
(2) Discontinuous: minimum amplitude less than 5 µV but demonstrating variability; maximum amplitude greater than 10 µV
(3) Burst suppression: minimum amplitude less than 3–5 µV with minimal variability; bursts greater than 25 µV of variable density
(4) Low voltage: continuous background with both minimum and maximum amplitudes less than 10 µV
(5) Inactive/flat: primarily isoelectric tracing with amplitudes less than 5 µV
b. Term infants with hypoxic-ischemic encephalopathy and prediction of outcome
(1) Background pattern: Recovery of a normal background pattern (either continuous or discontinuous) within 36–48 hours has been associated with a good outcome.
(2) Sleep-wake cycles: Shorter time to recovery of SWCs (before 36 hours) is associated with a good outcome. Never developing SWCs is strongly predictive of a poor outcome.
(3) Recovery of background pattern and SWCs may be delayed for infants treated with hypothermia.
c. Preterm infants: In healthy preterm infants, the aEEG matures from a discontinuous pattern to a continuous pattern with advancing gestational and postmenstrual age (Figure 78-4). In other words, the minimum amplitude increases, the bandwidth and maximum amplitude decrease, and there is interval development of SWCs. Isoelectric and low-voltage patterns have been associated with the development of intraventricular hemorrhage.
2. Seizures
a. An isolated seizure is reflected by an increase in the minimum amplitude; repetitive seizures appear as a “sawtooth” pattern (see Figure 78-5).
b. It is important to confirm seizure activity on the raw EEG tracing (see the section on limitations).
3. Sleep-wake cycling
a. Immature SWCs may begin to appear as early as 25 to 27 weeks’ gestational age, as evidenced by sinusoidal fluctuations in the minimum amplitude.
b. SWCs that are more mature in healthy infants appear between 30 and 34 weeks’ gestational age but are often shorter in duration compared to mature SWCs, which emerge at 36–37 weeks’ gestational age.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree