Ureteral Obstruction and Malformations
Hydronephrosis and ureteral malformations are among the most common anomalies in the urinary tract in children. Most are now detected prenatally. Urinary tract dilation is present in 1 in 100 fetuses, but significant uropathy is found in only 1 in 5001,2 (Fig. 54-1).

FIGURE 54-1 Normal kidneys are typically identifiable by 18 weeks in all fetuses. Dilated kidneys can be seen as early as 12–14 weeks of gestation. The arrow demonstrates left-sided caliectasis on a coronal fetal image.
Ureteropelvic Junction Obstruction in Children
Historically, the incidence of UPJ obstruction has been estimated at 1 in 5,000 live births. However, with the advent of antenatal ultrasonography (US), the prevalence of dilation has been found to be much higher. Retrospective reviews show that although the incidence of detected dilation has increased, the actual number of operations for UPJ obstruction has been relatively constant at 1 : 1,250 births.3,4 UPJ obstruction is more common in boys (2 : 1), and two-thirds occur on the left side. Bilateral dilation occurs in 5–10% of patients, and is much more frequently seen in younger children. Bilateral obstruction is much less common.5
Etiology
During development of the upper ureter, the lumen of the ureteral bud solidifies with ureteral lengthening and later recanalization.6 Failure to recanalize adequately is thought to be the cause of most intrinsic UPJ obstructions. Other causes of intrinsic UPJ obstruction include ureteral valves, polyps, and leiomyomas.7
The most common observation is ureteral narrowing of a variable length that joins the renal pelvis above the expected dependent position.8 At low volume, peristaltic waves of urine cross the UPJ. However, as the flow increases beyond a threshold, the renal pelvis dilates.9 The dilated pelvis may functionally kink the ureter further, increasing the pelvic pressure. In 20–30% of patients, the ureter is draped over a lower-pole vessel, producing an extrinsic UPJ obstruction. In most situations, there is also a coexisting luminal narrowing of the ureter.10
Histologic evaluation reveals a decrease or complete absence of smooth muscle fibers at the UPJ.11 Electron microscopy may show an increase in collagen deposition between the muscle fibers that is most likely a response to the obstruction as opposed to the cause.12 Fibrosis and interruption of the smooth muscle continuity block transmission of the peristaltic wave, while defective innervation also may play a role.13 UPJ obstruction also can be secondary, i.e., related to other ureteral pathology. It can be found in conjunction with high-grade vesicoureteral reflux (VUR), after cutaneous ureterostomy, and after decompression of the dilated urinary tract. VUR is present in 14% of patients with UPJ obstruction (Fig. 54-2).14,15
Clinical Presentation
Most renal dilation and obstruction are detected prenatally. Less frequently, it is detected because of an abdominal mass, urinary tract infection (UTI), or associated with other congenital anomalies (i.e., VACTERL syndrome). In older children, vague, poorly localized, cyclic or acute abdominal pain associated with nausea is common (Fig. 54-3). Some of these children are initially seen by gastroenterologists. The cause for the intermittent obstruction is unclear, but renal function is almost always preserved. Hematuria after minor trauma or vigorous exercise may be a presenting feature, most likely secondary to rupture of mucosal vessels in the dilated collecting system.5
Diagnosis
When the antenatal diagnosis of UPJ obstruction is made, the initial postpartum evaluation should be performed at 10 to 14 days of life to avoid false-negative studies resulting from the transitional nephrology of the newborn. Bilateral dilation is rarely associated with significant enough obstruction to cause oligohydramnios and warrant antenatal intervention. Ultrasound confirms the presence of pelvic and calyceal dilation, with variable thinning of the renal parenchyma. The Society for Fetal Urology (SFU) classification is typically used to describe the degree of dilation (Fig. 54-4).16 The presence of corticomedullary junctions is indicative of preserved function.15 Ultrasound is used to evaluate the contralateral kidney, the bladder, and the distal ipsilateral ureter to avoid confusion with a ureterovesical junction (UVJ) obstruction, but it does not provide functional information.
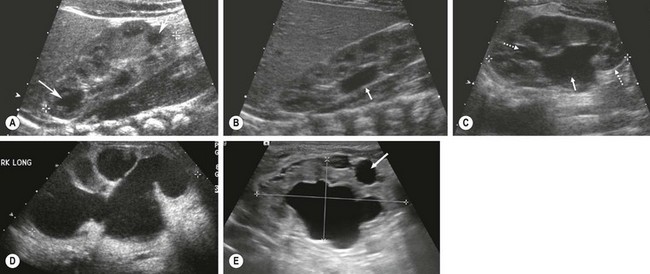
FIGURE 54-4 These neonatal ultrasound images come from infants with a history of prenatally detected renal dilation. (A) This ultrasound is normal for comparison purposes. There are dark renal pyramids (arrow) and no renal pelvic dilation. (B) This image shows isolated renal pelvic dilation (arrow) (SFU grade I). (C) This image shows dilation of the renal pelvis (solid arrow) and upper and lower-pole calyces (dotted arrows) (SFU grade II). (D) Calyceal dilation and cortical thinning are seen (SFU grade IV). (E) Hydronephrosis with peripheral cysts (arrow) indicating dysplasia is seen. This kidney had no function on renal scan.
In the past, routine antibiotic prophylaxis was utilized in all infants with prenatal dilation but the risk of UTI is very small in the absence of reflux.17 A voiding cystourethrogram (VCUG) was previously recommended in all patients being evaluated for UPJ obstruction. VUR increases the chance that infection will occur, even in a partially obstructed system. Between 5–30% of infants with prenatally detected dilation will have reflux, and the majority will spontaneously resolve without an infection.15 Children with isolated pyelectasis and no ureteral dilation have a very low incidence of reflux and do not need a screening VCUG.
The diuretic isotopic renogram is very useful for evaluating hydronephrosis, differential renal function, and renal drainage (Fig. 54-5). In this study, the transit of an injected radioisotope through the urinary tract is monitored by a gamma camera. The early uptake (first 1 to 2 minutes) of the tracer indicates the split renal function, while the washout, augmented by the administration of a diuretic, is evaluated and plotted by a computer to demonstrate drainage.18–20 The study is obtained with either 99mTc-mercaptoacetyltriglycine (99mTc-MAG3), whose clearance is predominantly via proximal tubular secretion, or with technetium-99m-labeled diethylenetriamine pentaacetic acid (99mTc-DTPA), whose renal clearance is by glomerular filtration. 99mTc-MAG3 is more efficiently excreted than 99mTc-DTPA and gives better images, particularly in patients with impaired renal function.19,20
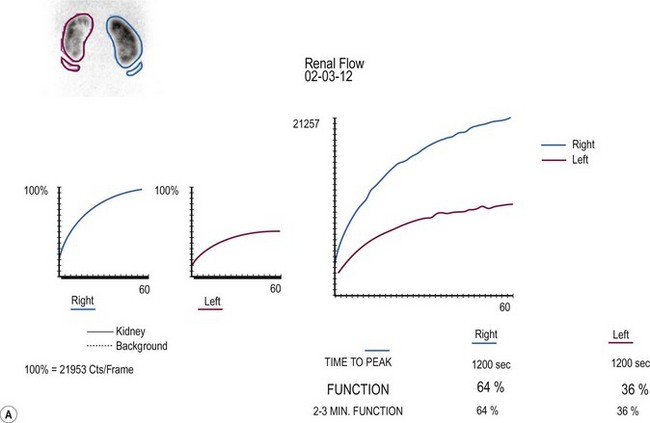

FIGURE 54-5 Renal scan in the evaluation of prenatally identified hydronephrosis. The ultrasound study showed diffuse caliectesis and pelvic dilation consistent with UPJ obstruction. (A) The dilated left kidney has reduced function. (B) Lasix should be administered once the renal pelvis is completely distended. In this case, it appears there is further accumulation (increased counts) after Lasix administration. Observation was chosen because the dilation was predominantly extrarenal, the kidneys were not palpable even after Lasix administration, and concern that the drainage time was perhaps falsely elevated. One year later, the renal dilation was markedly improved.
The technique for diuretic renography is standardized.20 Patients should be hydrated intravenously (15 mL/kg) 15 minutes before injection of the radionuclide. An indwelling catheter maintains an empty bladder and monitors urine output. The diuretic (1 mg/kg furosemide, up to 40 mg) is not administered until the activity peaks in the hydronephrotic kidney and renal pelvis. The tracer activity is then monitored for an additional 30 minutes, and a quantitative analysis is performed. Historically, persistence of more than 50% of the tracer in the renal pelvis 20 minutes after diuretic administration ( >20) is diagnostic of obstruction, although the applicability of this threshold in pediatric patients is debatable. False-positive results may occur when the immature neonatal kidney fails to respond to diuretic, when the diuretic is administered prior to maximal renal pelvic distension, when the patient is dehydrated, when the bladder is distended, or when the pelvis is significantly dilated.
>20) is diagnostic of obstruction, although the applicability of this threshold in pediatric patients is debatable. False-positive results may occur when the immature neonatal kidney fails to respond to diuretic, when the diuretic is administered prior to maximal renal pelvic distension, when the patient is dehydrated, when the bladder is distended, or when the pelvis is significantly dilated.
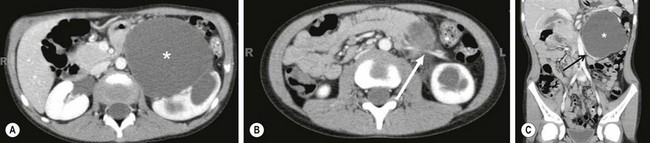
Magnetic resonance urography (MRU) can be used at any age. T2-weighted images are independent of renal function, and hydronephrosis is readily detected. The anatomic images are excellent (Fig. 54-6). Enhanced MR images with gadolinium can give information regarding differential function if one kidney is anatomically and functionally normal.21

FIGURE 54-6 In this 6-month-old infant, an ultrasound showed a dilated ureter below the kidney, but not at the level of the bladder. This coronal image shows marked dilation of the proximal ureter (arrow) and pelvis (asterisk) due to a proximal ureteral valve.
Rarely, when imaging is equivocal, invasive pressure flow studies may be indicated.22 These tests assume that obstruction produces a constant restriction to outflow that necessitates elevated pressure to transport urine at high flow rates. However, not all obstructions are constant. If the obstruction is intrinsic, a linear relationship exists between pressure and flow. However, in some cases, the results reflect only the response of the renal pelvis to distention and may be positive in the absence of obstruction. These studies require general anesthesia in children and have limited applicability.
Retrograde urography at the time of operative correction is helpful if uncertainty exists regarding the site of obstruction. This is rarely required because a well-performed ultrasound evaluation and radionuclide study will exclude distal obstruction.23 As there are risks with using instruments in the infant male urethra and the ureteral orifice, these retrograde studies are not usually performed.
Management
Indications for Intervention
Intermittent obstruction and pain are probably the most reliable indication for operation. Diminished function, delayed drainage, progression of pelvic and calyceal dilation on ultrasound, and loss of renal function are all potential indicators of obstruction. Randomization to operative and observational arms is complicated by a difficult decision that a parent has to make for the asymptomatic child.24 The morphologic appearance of a dilated renal pelvis on excretory urography or ultrasound is not a good indication for operation because many of these findings will resolve without the need for operation (see Fig. 54-5).25 Neonatal hydronephrosis can often be explained by physiologic polyuria and natural kinks and folds in the ureter.
The ongoing debate in the management of neonatal UPJ obstruction centers on the definition of significant obstruction. Diuretic renography has limitations in the neonate, although using the ‘well-tempered’ approach increases its value.20 The standard half-time of 20 minutes for obstruction in the neonate is misleading in many cases.
Differential renal function or individual kidney uptake is the most useful information obtained during renography.24–26 An indication for operation is diminished renal function in the presence of an obstructive pattern on renography. The threshold is arbitrary, but most surgeons believe that less than 35–40% function in the hydronephrotic kidney warrants correction. However, one series of patients with dilated kidneys and no more than 25% total renal function were found to improve to more than 40% of total function in all cases without operative correction.25 Long-term studies of kidneys with greater than 40% function have shown that fewer than 15–20% will require operation for diminishing function, UTIs, or unexplained abdominal pain.26,27 Some of these kidneys will regain some of the lost function.
If the child is initially seen with acute pain or infection, it is advisable to wait one to two weeks to allow the inflammation to resolve. Percutaneous drainage or stent placement for sepsis is rarely required preoperatively. It should be avoided in the absence of infection because of the inflammation that develops from a tube in the renal pelvis. Exploration of a poorly functioning kidney requires assessment of the renal parenchyma. If the parenchyma is grossly dysplastic or frozen-section analysis shows only dysplasia, then nephrectomy should be performed. No test accurately predicts recovery of function. Thus, nephrectomy is rarely performed in the infant with UPJ obstruction.
Operative Techniques
A dismembered pyeloplasty is the preferred technique to correct UPJ obstruction (Fig. 54-7). A successful outcome is achieved with construction of a funnel-shaped, dependent UPJ complex. The renal pelvis and upper ureter are mobilized and the ureter is divided just below the obstructed segment. It is spatulated on its lateral border through the aperistaltic segment. Usually, it is necessary to resect some of the renal pelvis to avoid postoperative obstruction. If this segment is particularly long, a flap of renal pelvis can be created. Foley YV-plasty and the Culp spiral flap were designed to maintain the continuity of the ureter and the pelvis.28,29 These techniques are used in unusual cases of malrotation, fusion anomalies, or long, stenotic segments.
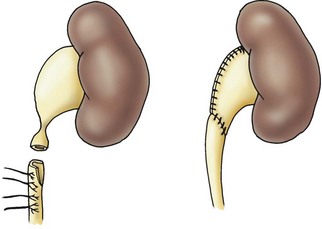
FIGURE 54-7 Dismembered pyeloplasty showing reduction of the renal pelvis and spatulation of the ureter (see the text).
Pyeloplasties are frequently performed without diversion so it is important to be as gentle as possible.30 Excessive handling of the pelvis and ureter increases edema. A stent is typically left in place after a laparoscopic repair. Even if leakage from the anastomosis occurs, a satisfactory outcome can usually be expected. A Penrose drain is left near the anastomosis and can usually be removed within 48 hours. If drainage is prolonged, the child can be discharged with the drain in place. Renal drainage is indicated in solitary kidneys or when simultaneous bilateral pyeloplasties are performed. In reoperation, it is technically more difficult to achieve a watertight anastomosis and internal drainage (stent, nephrostomy or nephrostent) is indicated.
Extrinsic UPJ obstruction associated with an aberrant lower-pole vessel requires division of the ureter at the UPJ and performance of a standard dismembered pyeloplasty after transposing the ureter to a nonobstructed position. This is preferable to laparoscopic transposition of the crossing vessel. In the case of an intrarenal pelvis or when significant scarring is found at reoperation, a ureterocalicostomy is a useful technique.31 A portion of the lower pole should be resected to prevent a postoperative stricture. The ureter is spatulated and then anastomosed to the exposed calyx in the lower pole.
The open approach still has a role in infants and young children. Laparoscopic pyeloplasty has been performed in all ages and the age of the patient is inversely related to benefits of decreased pain and convalescence.32 Open pyeloplasty can be performed through a flank, anterior extraperitoneal approach, or posterior lumbotomy approach. The anterior approach involves a transverse incision from the edge of the rectus to the tip of the 12th rib.33 The retroperitoneum is entered and the UPJ is exposed, with the kidney left in situ. In infants, this is a muscle-splitting incision with low morbidity. The posterior lumbotomy also can be easily performed in infancy and provides direct access to the UPJ.34 The kidney does not require mobilization, and the ureter and renal pelvis can usually be delivered into the incision. In bilateral cases, the child does not need to be repositioned. The lumbotomy approach should not be used with a malrotated kidney or a kidney that has an intrarenal pelvis. An anterior or flank approach is always preferred for reoperation although laparoscopy and endopyelotomy have largely replaced open re-operative pyeloplasty.35
Endoscopic approaches (endopyelotomy) for UPJ obstruction were popularized in the 1980s and 1990s, but have been replaced by laparoscopic approaches.36,37 Endopyelotomy successfully relieves primary UPJ obstruction in 70% of children.38 As the success pales in comparison to pyeloplasty, it is not routinely utilized for primary repair. Endopyelotomy clearly has a role in recurrent UPJ obstruction, in which the success rate is >95%.38 Depending on the age of the patient and the size of the ureter, this can be performed in either an antegrade or retrograde fashion (Fig. 54-8).

FIGURE 54-8 Retrograde endopyelotomy. Sixteen-month-old infant with persistent hydronephrosis and preserved function, but no washout on renal scan 6 months after undergoing a dismembered pyeloplasty. (A) The retrograde pyelogram shows a UPJ configuration with dilute contrast in a dilated renal pelvis (arrow). (B) A balloon catheter is passed retrograde and inflated. The black arrow shows the narrowing (waist) and the white arrow demonstrates the cutting wire that is positioned laterally. (C) An indwelling stent is positioned after the endopyelotomy is performed. The white arrow points out the extravasation that is indicative of an appropriate depth of incision.
The first laparoscopic pyeloplasty in a child was reported in 1995 by Peters.39 The first series was published by Tan in 1999.40 Laparoscopic pyeloplasty has been reported in children as young as 2 months.41 The introduction of robotic surgery with articulating instruments and three-dimensional visualization has made intracorporeal suturing easier and more precise. The success rate with minimally invasive techniques is equivalent to open pyeloplasty.42,43 The benefits of laparoscopic and robotic surgery over an open approach may include a decreased length of hospitalization, decreased analgesic requirements, improved cosmesis, and quicker return to normal activity.42
Laparoscopic pyeloplasties are mostly performed using the Anderson–Hynes dismembered technique (Fig. 54-9). This can be performed through either a transperitoneal or retroperitoneal approach using a similar technique once access and exposure are obtained. With both transabdominal and retroperitoneal approaches, the child is placed in a flank or modified flank position.
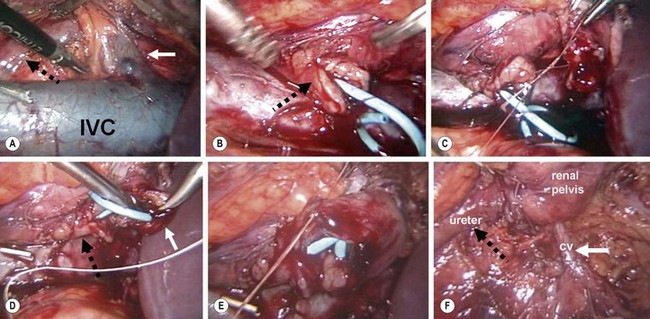
FIGURE 54-9 Laparoscopic pyeloplasty. (A) Transperitoneal view of crossing vessel (solid white arrow) that is causing intermittent obstruction of the ureter (dotted black arrow). IVC, inferior vena cava. (B) The ureteropelvic junction has been transected and the ureter spatulated (arrow), and a double J stent has been positioned in the bladder and out the proximal ureter. This can be accomplished via a retrograde or antegrade approach. (C) The posterior anastomosis between the renal pelvis and ureter is being performed. (D) The proximal end of the stent is inserted into the renal pelvis (solid white arrow). The ureter is marked with the dotted black arrow. (E) The anterior anastomosis is being performed. (F) The completed anastomosis is seen with the crossing vessel (white arrow, CV) now located posterior to the pyleloplasty. Again, the ureter is marked with the dotted black arrow. (Images courtesy of R. Sherburne Figenshau, MD.)
UPJ Obstruction in a Duplex Kidney
In a duplex kidney, the lower pole is most commonly affected because the upper pole lacks a true pelvis.44 Ultrasound may not be reliable for diagnosis because the duplex nature of the kidney may not be identified. A pyelogram or renogram will show a small nonobstructed upper segment.
Surgical Results and Complications
The results of operative correction have been uniformly successful when performed at children’s hospitals.27,30,35 The rate of recurrent UPJ obstruction is less than 1%, and the nephrectomy rate is less than 2%. The most common early complications are prolonged urinary extravasation and delayed drainage through the anastomosis. If a significant leak develops, either a stent or a percutaneous nephrostomy tube can be inserted. Once diversion is instituted, the leak will usually cease within 48 hours. Late scarring at the anastomotic site is common, but rarely occurs due to a leak.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree