Upper and Lower Gastrointestinal Bleeding
Richard J. Noel
Gastrointestinal (GI) bleeding occurs rarely in children; severity varies from the insidious bleed, with only iron-deficiency anemia suggestive of occult hemorrhage, to dramatic hemorrhage with rapidly evolving, life-threatening hypovolemic shock. Upper GI bleeding is bleeding from a source proximal to the ligament of Treitz (duodenojejunal junction). Hematemesis is the vomiting of frank blood and suggests a rapidly bleeding lesion. Coffee-ground emesis describes the appearance of vomited blood that has been coagulated by gastric acid. Hematochezia is blood passed with stool from the anus. Blood limited to the outside of otherwise unremarkable stool suggests a rectal origin; blood mixed throughout the stool suggests a colonic source. Melena is black, tarry stool produced by the oxidation of heme by intestinal flora; as little as 50 mL of blood may result in melena, and it may persist for 3 to 5 days following resolution of the bleed. Maroon-colored stool is associated with rapidly bleeding small bowel lesions in which the transit of blood is too fast for complete oxidation. Currant-jelly stool is associated with ischemic small bowel or proximal colonic lesions such as may be seen in intussusception. Occult GI bleeding is bleeding that occurs in the absence of overt bleeding and is usually suspected due to chronic iron-deficiency anemia or is identified by hemoccult examination.1
 CLINICAL FEATURES AND DIFFERENTIAL DIAGNOSIS
CLINICAL FEATURES AND DIFFERENTIAL DIAGNOSIS
Upper GI Bleeding
Disorders causing upper gastrointestinal (GI) bleeding occur with varying frequency depending on the age of presentation (Table 387-1).2 In the newborn several unique disorders not usually considered in the differential diagnosis of older infants and adults must be considered. Swallowed maternal blood, either from parturition or from feeding from a fissured nipple, may cause what appears to be GI bleeding. Hemorrhagic disease of the newborn may occur when neonatal vitamin K is not administered at birth, and it should be considered in newborns born outside of traditional medical settings or who required acute resuscitation at birth such that routine administration was neglected. Peptic disease may occur in newborns and result in gastritis or ulceration. Dietary protein intolerance (often cow milk) may result in mucosal inflammation and hemorrhage. GI obstruction such as may be seen in pyloric stenosis or midgut volvulus may present with GI bleeding.
GI bleeding in the infant may occur from disorders similar to those in the newborn. Recurrent vomiting from other etiologies may result in physical tearing, leading to a Mallory-Weiss tear or traumatic (prolapse) gastropathy. Infants may also develop GI bleeding associated with congenital conditions that are delayed in clinical presentation, such as vascular anomalies, GI duplications, webs, or midgut volvulus associated with malrotation. Variceal hemorrhage may occur in infancy as the presenting sign of liver or portal vascular disease; a history of umbilical catheterization may be seen in cases of cavernous transformation of the portal vein.
Children and adolescents may present with GI bleeding associated with peptic disease, Mallory-Weiss tears, and varices. A Dieulafoy lesion may result in vigorous hemorrhage. Variceal hemorrhages occur with liver disease. Foreign body ingestions may result in bleeding associated with mucosal erosion, particularly from esophageal impaction of coins or other foreign bodies. Similarly, caustic ingestions may present with GI bleeding. Vasculitis may result in GI bleeding. Hemobilia from biliary disease or endoscopic retrograde cholangiopancreatography (ERCP) may result in hemorrhage into the descending duodenum with either an upper or lower GI presentation. Inflammatory bowel disease may result in upper GI bleeding with Crohn disease or immunodeficiency-related inflammation.
Lower GI Bleeding
Disorders causing lower GI bleeding also vary in frequency depending on the age of presentation (Table 387-2).2 Large-volume upper intestinal hemorrhage may present with lower GI bleeding, particularly in infants, so it is important to consider causes of upper GI bleeding in the differential diagnosis. Hematochezia or melena in newborns should prompt concerns for necrotizing enterocolitis, particularly in premature or critically ill newborns. Bowel obstruction, such as with midgut volvulus, should also be considered.
Table 387-1. Etiology of Upper Gastrointestinal Bleeding by Pediatric Age*
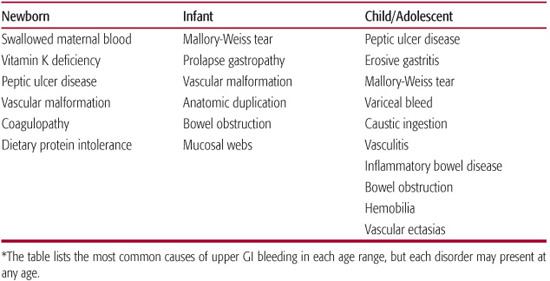
Table 387-2. Etiology of Lower Gastrointestinal Bleeding by Pediatric Age*
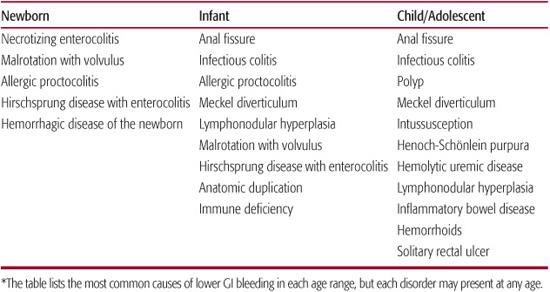
Eosinophilic proctocolitis may result from dietary protein intolerance and may present with painless hematochezia in otherwise healthy-appearing newborns. A history of constipation in an infant presenting with bloody diarrhea may suggest a diagnosis of enterocolitis associated with Hirschsprung disease. Hemorrhagic disease of the newborn should be considered in newborns not receiving vitamin K at birth.
Older infants may also develop lower GI bleeding from bowel obstruction, enterocolitis (possibly Hirschsprung-related), or dietary protein intolerance. Intussusception may present with currant-jelly stools and a palpable abdominal mass. Bleeding that is apparently painful may be associated with anal fissures, infectious colitis, or immunodeficiency-related colitis. Painless bleeding may be seen with a Meckel diverticulum, intestinal duplication, or lymphonodular hyperplasia.
Painful bleeding in children and adolescents may be associated with an anal fissure or infectious colitis. Constipation may result in rectal mucosal tears. Hemolytic-uremic syndrome may result from Shiga toxin–producing bacteria, including Escherichia coli 0157-H7. Inflammatory bowel disease (proctitis, ulcerative colitis, or Crohn disease) may be diagnosed in young children but typically presents later in childhood or adolescence. Intestinal inflammation from Henoch-Schönlein purpura may be seen in children and adolescents. Painless bleeding suggests a Meckel diverticulum or polyp; the latter are typically nonmalignant hamartomas.
 DIAGNOSTIC EVALUATION AND TREATMENT
DIAGNOSTIC EVALUATION AND TREATMENT
Initial Assessment and Management
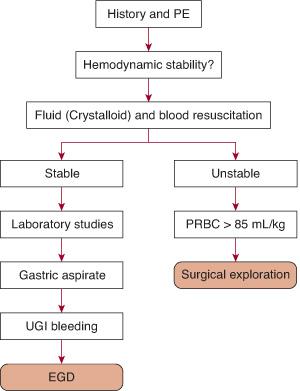
A systematic approach, including assessment of hemodynamic parameters, history, physical examination, diagnosis, and treatment of the source, is required. The care of pediatric patients with GI bleeding is summarized in Figures 387-1 and 387-2 and begins with a clinical assessment of hemodynamic status. An initial survey of the patient’s alertness should rapidly screen for those who are lethargic and may merit aggressive resuscitation. Tachycardia suggests hypovolemia. Hypotension is worrisome, as it may be a late sign of impending hypovolemic shock (see Chapter 103). Patients with the acute onset of GI bleeding often require hospitalization for monitoring. If hemodynamically unstable, volume resuscitation with crystalloid is a priority, followed by replacement of blood. Medical management of upper GI bleeding may include administration of intravenous proton-pump inhibitors.3 A patient who remains hemodynamically unstable after crystalloid resuscitation and transfusion of up to 85 mL/kg of packed red blood cells should be considered for immediate endoscopy and/or surgical exploration without delay in order to make an extensive evaluation.
Clinical Features
The history is initially focused on assessment of the severity of bleeding, but it may provide clues regarding the underlying cause of bleeding if the patient has a condition known to predispose to bleeding, such as hepatic cirrhosis, a disorder associated with vascular malformations, a bleeding disorder, or use of medications such as nonsteroidal anti-inflammatory drugs.4,5 Bleeding associated with a history of pain is more likely associated with an inflammatory lesion or ischemia, whereas painless bleeding is more likely associated with a vascular lesion or bleeding from a Meckel diverticulum. However, the history generally is inadequate to determine the cause of GI bleeding.
Physical examination should assure hemo-dynamic stability with vital signs within normal parameters for the child’s age. Attention should focus on signs of chronic liver disease that may present with esophageal variceal hemorrhage; such signs include ascites, hepatosplenomegaly, and spider telangiectasias. Vascular malformations of the skin suggest the possibility of similar internal (GI, pulmonary, or airway) lesions. Cutaneous purpura suggests clotting or vascular dysfunction that may also affect the GI tract. Nasal and oropharyngeal examination may reveal mucosal or gingival sources that result in hematemesis of swallowed blood.
A laboratory assessment should include a complete blood count with a reticulocyte count that may help differentiate acute from chronic conditions. Coagulation indices (prothrombin, partial prothrombin times, international normalized ratio) will help identify a bleeding disorder. Elevation of serum aminotransferases may indicate liver disease.6 Serum albumin may be decreased in both liver and inflammatory bowel disease. Blood urea nitrogen and creatinine will indicate renal disease and may also be elevated due to resorption of blood from the GI tract. Blood should be typed and crossmatched for transfusion.
Apparent blood seen in the emesis, gastric aspirate, or stool may be rapidly tested for blood using cards impregnated with guaiac, a colorless resin that is oxidized in the presence of both peroxidase (test reagent) and peroxidase activity from hemoglobin. False-positive results may arise from nonhuman hemoglobin peroxidase activity from red meat, melons, grapes, radishes, turnips, cauliflower, and broccoli. Iron supplements may result in a dark color but do not cause false-positive reactions. Heme-positive gastric aspirates may indicate a gastric or esophageal source or swallowed blood from the lungs or airway. A negative aspirate does not rule out duodenal bleeding. In the assessment of GI bleeding from neonates, the Apt-Downey test can help identify swallowed maternal blood via the differential denaturation of maternal and fetal blood exposed to alkali.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


