Fig. 24.1
ESHRE/ESGE classification of uterine horns with cavity: hemi-uterus with rudimentary cavity (Class U4a) and aplastic uterus with rudimentary cavity (Class U5a)
On the other hand, uterine aplasia is classified as ESHRE/ESGE Class U5. Cavitated or non-cavitated rudimentary horns could be also present in those women; cases of uterine aplasia with uni- or bilateral rudimentary cavity are clinically significant variants and they are sub-classified as ESHRE/ESGE Class U5a (Fig. 24.1) [31, 32].
Incidence of Rudimentary Horns
The true incidence of female congenital malformations is unknown. The use of diagnostic methods with different accuracy, the subjectivity in the criteria used for diagnosis and classification of the anomalies and the drawbacks of the existing classification systems represent the main biases for that [33, 64]. Moreover, in some studies the population was not representative whereas the existence of undiagnosed cases is another potential bias, as many of the patients with malformations may be asymptomatic without ever reporting any gynaecological or reproductive problem.
Reports in the literature estimate that the incidence of female genital anomalies in general population varies between 4.3 and 6.7 %, while in women with fertility problems between 3.4 and 10.8 %. In patients that suffer from recurrent miscarriages, congenital anomalies are reported to range between 12.6 and 18.2 % [34, 64]. In a more recent review of 94 observational studies comprising 89.861 women, the prevalence of uterine anomalies diagnosed by optimal tests (investigations that are capable of accurately identifying and classifying congenital uterine anomalies accurately) was found to be 5.5 % [95 % confidence interval (CI), 3.5–8.5] in the general/unselected population, 8.0 % (95 % CI, 5.3–12) in infertile women, 13.3 % (95 % CI, 8.9–20.0) in those with a history of miscarriage and 24.5 % (95 % CI, 18.3–32.8) in those with miscarriage and infertility [9].
In a systematic review of studies using high-accuracy diagnostic methods, the mean prevalence of unicornuate uterus (currently ESHRE/ESGE hemi-uterus) was found to be 0.4 % in general population; in infertile patients it was 6.1 % and in recurrent miscarriage patients 2.3 % respectively [64]. In another more recent review overall 0.1 % (95 % CI, 0.1–0.3) of the unselected population had a unicornuate uterus diagnosed by an optimal test. It is important to note that unicornuate uterus was found to be significantly more common in women with a history of miscarriage (0.5 %; 95 % CI, 0.3–1.1; P = 0.025), miscarriage in association with infertility (3.1 %; 95 % CI, 2–4.7; P < 0.001) and infertility (0.5 %; 95 % CI, 0.3–0.8, P < 0.01) when compared with the unselected population [9]. Rudimentary horns with cavity are found in 74 % of unicornuate uteri. The prevalence of non-communicating horns is 70–90 % [39].
Patients with aplastic uterus usually have co-existent defects and mainly vaginal aplasia, the well-known Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome (ESHRE/ESGE Class U5/C4/V4). The reported incidence of MRKH syndrome is 1/4,000 [3]. The presence of uterine remnants is not rare; in a cohort of 284 patients with MRKH syndrome 84.2 % had bilateral and 9.5 % had unilateral rudimentary or aplastic horns [52]. However, only a minority of them are rudimentary horns with functional cavity; in a cohort of patients with MRKH syndrome, 7.5 % of them had rudimentary cavity >4 cm (ESHRE/ESGE Class U5a) [23].
Diagnosis
The diagnosis of these anatomical malformations is not an easy task. Bimanual examination can miss the presence of a small non-communicating horn and possible luck of symptoms may disorient the clinicians from the correct diagnosis. The extensive use of transvaginal ultrasound proved an effective diagnostic tool to evaluate the presence of a rudimentary horn. Traditionally, Magnetic Resonance Imaging (MRI) has been considered the best noninvasive method for diagnosing those Müllerian anomalies (Fig. 24.2). MRI provides excellent delineation of both the internal and external uterine contours and enables measurement of the intercornual diameter, visualization of the endometrial contour, and identification of a uterine horn should one be present [17]. MRI has been quoted as having an accuracy of up to 100 % in correctly identifying müllerian anomalies [58].
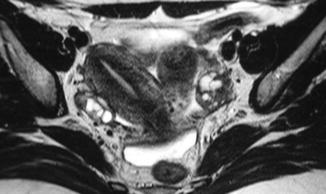
Fig. 24.2
Right hemi-uterus with a left non-communicating rudimentary horn with cavity: magnetic resonance imaging (MRI) findings
Like MRI, three-dimensional ultrasound (3D US) allows the assessment of both the internal and external uterine contours. The addition of the coronal plane enables visualization of the cavity and fundus; 3D US and Doppler studies further enable the study of vascularization and the calculation of the uterine cavity volume. The accuracy of 3D US in the diagnosis of uterine malformations has been reported to be very high with a sensitivity of 98 % and specificity of 100 % [18]. In another study comparing MRI with 3D US for the diagnosis and classification of uterine anomalies, images obtained from each modality were practically equivalent. The authors argued that 3D ultrasound was a valid alternative to MRI, considering its lower cost and that it improves patient tolerability [7].
As there is an association between obstructive müllerian anomalies with renal abnormalities and endometriosis, pre-operative assessment for renal anomalies by renal ultrasonography or intravenous pyelography should be performed routinely. MRI may also aid in the diagnosis. Once the diagnosis is made, other useful information includes the type of attachment and communication between the rudimentary horn and unicornuate uterus, the presence of a cavity in the horn, and the size of the hematometra.
Hemi-uterus with Rudimentary Cavity (ESHRE/ESGE Class U4a)
Clinical Presentation
Hemi-uteri with rudimentary cavity are susceptible to many gynecologic and obstetric complications; endometriosis, primary infertility, hematometra, and urinary tract anomalies are common in those women [25, 36]. However, non-communicating cavitated rudimentary horns are the most clinically significant as they are more likely to be associated with pelvic pain from hematometra or from endometriosis due to retrograde menstruation from the existing functional endometrium. It seems that, the prevalence of endometriosis in patients with hemi-uterus was significantly greater than that in patients with other non-obstructive Mullerian anomalies [24, 36]. Such horns often require surgical resection for symptoms relief. The symptoms associated with functional non-communicating horns result mainly from cryptomenorrhea. The presentation varies from progressive or chronic pelvic pain following menarche, to a more acute-onset abdominal pain or a more delayed-onset of dysmenorrhea [39].
Treatment
Excision of the Rudimentary Cavity
The excision of the rudimentary horn is the proposed treatment; since its first documentation [8], laparoscopic management of unicornuate uterus with rudimentary horn is the preferred alternative method to laparotomy. The ipsilateral fallopian tube should be removed to prevent tubal pregnancy in the future [26, 70] (Fig. 24.3). If the contralateral tube is damaged then microsurgical Fallopian tube transposition can be considered [28].
Fig. 24.3
Laparoscopic view after removal of a left non-communicating rudimentary horn with cavity together with the ipsilateral tube
Laparoscopy offers the advantage of a shorter hospital stay, quick recovery, less postoperative pain and fewer short- and long-term complications such as infections and adhesions. In addition, smaller incisions are made leading to minimal abdominal scar formation. The shift to laparoscopic surgery for uterine rudimentary horns excision follows a similar trend in the introduction of minimally invasive surgical approaches for hysterectomy and myomectomy.
Preoperative treatment with a GnRH-analogue or danazol has been suggested aiming to reduce the size of hematometra before surgery [44, 50]. Other authors reported excellent laparoscopic results without application of any medical treatment prior to surgical laparoscopic management [26, 70].
The laparoscopic procedure is greatly influenced by the extent of the anatomical connection between the rudimentary horn and the unicornuate uterus. When the attachment is very broad, the endoscopic procedure tends to be tougher. In fact, the cleavage plane between the unicornuate uterus and the rudimentary horn is not well defined. The firmly attached rudimentary horn is likely to receive its blood supply not only from the ipsilateral uterine artery, but also from the myometrial arcuate arteries of the contralateral uterine artery, which need to be carefully occluded during dissection [22, 59].
A key aspect during laparoscopic surgery is avoidance of damage to the remaining hemi uterus so as to preserve fertility. Surgical removal of the attached horn may leave a myometrial defect that has to be repaired. Application of sutures requires good laparoscopic skills, and experience in intra-corporeal or extra-corporeal suturing is essential. If such intervention occurs, Caesarean section should be the mode of delivery in future pregnancies, due to increased risk of rupture of the repaired hemi-uterus. The use of both scissors and electrosurgery for the dissection has been reported [22, 26, 70]. However, with the recent advances in laparoscopic equipments, an ultracision energy scalpel has been also used for more accurate and easier dissection [12]. The simultaneous use of hysteroscopy to separate the two horns and the use of automatic endoscopic staplers instead of diathermy have also been reported [44, 50, 59]. The procedure can also be assisted by robotic technology [66].
In cases that the non-communicating rudimentary horn is firmly attached to the hemi uterus laparoscopic surgery becomes more complex. Cautious surgery to avoid damage to the remaining uterus can result in retention of functional tissue from the contralateral side and later recurrence with further menstrual obstruction [48].
In all cases identification of the ureter is essential and in some cases anatomical dissection might be necessary to prevent their injury [22, 26, 48, 70]. The excised rudimentary horns can be removed through an enlargement of the suprapubic trocar site [70]. This procedure is easy to perform and also ensures an excellent cosmetic result. Colpotomy or morcellation may be alternative methods, especially in cases where the specimen is large or solid and malignancy is not suspected [26].
Restoration of Continuity
In cases of a cavitated rudimentary horn that is firmly attached to the hemi-uterus, an alternative and more conservative surgical procedure can be applied. Dilatation of the cervix is performed followed by insertion of resectoscope. Preferably under ultrasonograhic guidance, incision is made at the uterine cavity surface that is in contact with the rudimentary cavity, till the continuity of the cavities is restored. As soon as the rudimentary cavity is identified, the incision is extended up to the rudimentary cavity margins.
This technique most likely eliminates the clinical symptoms from haematometra and allows functionality of the cavity. On the other hand, if such interventions are applied attention should be given in the possibility of a future pregnancy in the restored rudimentary horn cavity and its consequenses.
Rudimentary Horn Pregnancy and its Management
Pregnancy in the rudimentary horn is a rare complication and can become possible when sperm migration occurs through the peritoneal cavity. The natural course of a rudimentary horn pregnancy is rupture during the first or mid-second trimester; in the majority of cases, horn rupture occurs before 20 weeks resulting in a life threatening heavy intra-peritoneal bleeding associated with high maternal mortality rates [14]. Reports of rupture in the third trimester of pregnancy have been also described. The term “ectopic” is adopted for horn pregnancies due to their dramatic natural course. Rupture is attributed to the compromised thickness of the poorly developed horn musculature and impaired distensibility of the myometrium [14, 41, 54].
Fetal survival could not be excluded, but even then the prognosis is poor, with an increased risk of miscarriage, fetal growth restriction, oligohydramnios, preterm labor and fetal malpresentation. Intrauterine growth restriction and intrauterine fetal death are presumed to be secondary to the poor vasculature of the horn and, placenta accreta secondary to the poorly formed endometrium [27, 36, 38, 49].
Its estimated prevalence is one out of 76,000–150,000 pregnancies; 5.3 % of them are twins [49]. The mortality rate has been reduced from 23 % at the turn of the twentieth century to 0.5 % nowadays. Fetal survival was only 6 % [49]. The dramatic improvement in maternal mortality rates is likely to be related to an increase in pre-rupture diagnosis and prompt intervention. However, sensitivity of ultrasound for the diagnosis of rudimentary horn pregnancies remains poor and is less than 30 % [10, 39, 40].
Delay in diagnosis and hemorrhage may result in an adverse pregnancy outcome in such cases. Prompt intervention is necessary to remove the horn and its tube when a diagnosis of pregnancy is made. Because in most cases of uterine horn rupture occurs in the second trimester, early diagnosis in the first trimester provides time to take measures that can minimize surgical risks. Laparotomy in these cases is always mandatory. However, early diagnosis of pregnancy has recently facilitated management of rudimentary horn pregnancy by laparoscopic means [20].
Most cases of rudimentary horn pregnancies provide a diagnostic challenge and are diagnosed after rupture, leading to emergency surgery, blood transfusion, and increased morbidity [68]. Three-dimensional ultrasound imaging and MRI are useful tools with improved diagnostic accuracy, guiding both counseling and surgical planning. It is important to emphasize that, although cases of neonatal survival have been reported, life-threatening uterine rupture and hemorrhage at early gestational weeks remain the most likely outcomes, and neonatal survival is still rare [5, 41, 54].
Differential diagnosis of rudimentary horn pregnancy includes ectopic pregnancy, appendicitis, intestinal perforation, and even peptic ulcer disease. The common misdiagnoses on ultrasound includes bicornuate uterus with pregnancy in one horn, uterus didelphys, abdominal pregnancy, or even normal intrauterine pregnancy with an adnexal mass undergoing torsion [11, 21, 38, 62, 68].
The contour of the uterine cavity, the number of interstitial tubes, communication between the gestational sac and uterine cavity, continuity of the myometrium surrounding the sac with the uterus, the presence of a connecting vascular pedicle, and the mobility of the gestational sac could help in distinguishing intrauterine pregnancy in an anomalous uterus, from tubal, interstitial, abdominal, and cornual pregnancies [46]. Pseudo pattern of asymmetrical bicornuate uterus, absent visual continuity between cervical canal and lumen of pregnant horn, and the presence of myometrium surrounding the gestational sac can be also criteria for the antenatal diagnosis of rudimentary horn pregnancy [71]. Other criteria that can help in ultrasonographic diagnosis include greater distance between the horns, US with the use of intrauterine Foleys, hyper-vascularity of the placenta, the presence of very thin surrounding myometrium, the presence of placenta accreta, intraperitoneal free fluid, and the presence of an empty uterus and an ectopic gestational sac [68].
Three-dimensional ultrasound imaging and MRI have proved useful for a detailed evaluation of the fetus and the placenta and they both characterize more accurately the pregnant and non-pregnant uterine malformations [60, 63, 71]. MRI, though many times is limited by expense and availability, is a better diagnostic tool as it provides better differentiation of the anatomical structures inside and outside the uterus in both axial and coronal sagittal planes. It can be used for diagnosing uterine anomalies, communication of the uterine cavity and horn, and for planning surgery by localizing the position of its attachment [53].
Prompt intervention is necessary to remove the horn and its tube when a diagnosis of pregnancy is made. Surgical excision of the rudimentary horn and ipsilateral fallopian tube is the gold standard of management. Traditionally, such surgical resection has been accomplished via laparotomy, but with increasing expertise in laparoscopic surgery there have been several reports of endoscopic management of the pregnant rudimentary horn. Removal of the ipsilateral fallopian tube is essential [13, 19, 20, 37, 56, 65, 73].
The principles of surgery are similar to that in the non-pregnant state. However, in the pregnant woman the pedicles are likely to be more vascular. Medical management with methotrexate and potassium chloride followed by gonadotrophin-releasing hormone injections have also been used pre-operatively to reduce the blood loss from the associated placenta accreta. This enables a delayed laparoscopic excision of the uterine horn in a safe and less invasive manner [13, 21, 56, 69].
Aplastic Uterus with Rudimentary Cavity (ESHRE/ESGE Class U5a)
Clinical Presentation
Women with aplastic uterus, associated usually with cervical and vaginal aplasia in the context of MRKH syndrome, present with primary amenorrhea. The presence of a rudimentary cavity is an important factor as it can be responsible for symptoms in the clinical presentation of women with such malformations, mainly cyclic recurrent lower abdominal pain. The escalating pain inevitably leads to the need of surgical intervention; removal of the remnant hematometra and in some cases of the coexisting hematosalpinx as well is an established treatment alternative [6, 29].
Treatment
Excision of the Rudimentary Cavity
Treatment strategy for these patients is not well defined. Removal of the remnants of the müllerian ducts by laparoscopic means in patients with MRKH has been described in the literature [45, 57, 72]. Prophylactic removal of uterine rudiments in women with MRKH is still controversial. The pain is clearly not dependent on the presence of endometrium within the uterine rudiments. In a recent study of women with MRKH only 46.2 % of patients reported cyclic lower abdominal pain and 41.4 % of asymptomatic patients had evidence of endometrium in the rudimentary horn [61]. Cyclically recurrent lower abdominal pain resulting from endometrial proliferation within uterine rudiments, from endometriosis and myomas has been described in 6–10 % of patients with MRKH syndrome [47, 30, 55, 15, 16, 42, 43]. The incidence of pelvic endometriosis resulting from retrograde menstruation in patients with MRKH having rudimentary cavity is high and laparoscopic excision has been proposed as the preferred procedure when the uterine remnants and pelvic endometriosis cause cyclic pelvic pain [2].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


