FIGURE 37-1 Healed diaphyseal forearm fracture in patient with complete ulnar nerve palsy at 7 months postinjury.
CLINICAL QUESTIONS
- Which nerves are most commonly injured with which fractures or dislocations?
- What are the chances of spontaneous recovery of a major (axillary, median, ulnar, or radial) peripheral nerve injury associated with an upper limb fracture and/or dislocation?
- How long should an impaired nerve in a child be observed expecting recovery?
- What are the indications for exploration of a nonfunctioning nerve after blunt trauma?
- When should open lacerations be explored for vital soft tissue injuries?
- What are the surgical options for reconstruction of a chronic nerve palsy?
- What are the indications for nerve decompression, neuroma resection and grafting, or nerve transfers for a peripheral nerve palsy?
- What are the indications for tendon transfers for median, ulnar, and radial nerve palsies?
- Which tendon transfers give the best results?
THE FUNDAMENTALS
Etiology and Epidemiology
Every nerve and blood vessel can be injured by localized blunt or sharp trauma. Nerve injuries can be partial or complete and transient or permanent. Seddon classified, and Sunderland modified, nerve injuries by the extent of anatomic injury and implied recovery. Seddon defined injuries as neurapraxia, axonotmesis, and neurotmesis.1 Sunderland defined five degrees of injury based on nerve fascicular layers with first-, third-, and fifth-degree injuries closely approximating Seddon neurapraxia, axonotmesis, and neurotmesis categories, respectively.2 First- and second-degree (neurapraxia) injuries will recover completely, as the endoneurium is intact. Third- and fourth-degree injuries (axonotmesis) will probably have incomplete recovery, as the perineurium is variably intact, and the endoneurial sheath heals with some degree of scar (neuroma in continuity). Fifth-degree (axonotmesis) injuries do not heal because the nerve is no longer in continuity. The trick is figuring out which injury the patient has as early as possible. In children, the odds are that their blunt trauma nerve injuries will be neurapraxia or minor axonotmesis (Sunderland first- and second-degree)2 injuries and recover fully. The key is figuring out the entrapped, compressed, kinked, or lacerated nerve (about 2% of all nerve injuries associated with non-hand, nonamputation, pediatric upper limb fractures or dislocations) before irreversible nerve and muscle impairment occur. Of note, open fractures are higher risk for nerve entrapment or laceration. Deep glass lacerations are unusual if they do not cut vital soft tissues. A high index of suspicion and precise, thorough exams are imperative to recognize the nerve injuries that will not resolve on their own.
Clinical Evaluation
A complete neurovascular exam is mandatory in the acute setting for every patient presenting with musculoskeletal trauma. The same is true for postreduction and postoperative evaluation of every patient under your care. All patients with an acute nerve injury require important care discussions and decisions regarding further testing, observation, or surgery.
It is imperative that all pediatric upper limb and hand surgeons know human nerve anatomy and innervation patterns. Neurovascular injuries with musculoskeletal trauma are geographic. If you precisely know the anatomy, you will be able to isolate, protect, mobilize, decompress, and/or reconstruct each nerve in the upper limb. You obviously have to know specifically how to test for each nerve on physical exam for accurate pre- and postoperative assessment.
The radial nerve innervates the triceps; wrist extensors (extensor carpi radialis longus [ECRL] and extensor carpi radialis brevis [ECRB]); digital extensors (extensor digitorum communis [EDC], extensor indicis proprius [EIP], and extensor digiti quinti [EDQ]); thumb (extensor pollicis longus [EPL]); and long thumb abductor (abductor pollicis longus [APL]). Sensibility is in the dorsal first web space. The radial nerve departs from the posterior cord of the brachial plexus and enters the upper arm between the medial and long heads of the triceps while innervating both muscles. The radial nerve, after innervating the lateral head of the triceps, enters the intermuscular septum of the humerus, goes around the spiral groove, and exits anteriorly between the brachioradialis (BR) and brachialis. The main nerve innervates the BR and ECRL in the distal humerus before branching into the posterior interosseous nerve (PIN) and superficial radial sensory nerve. The radial sensory nerve courses down the forearm beneath the BR and then emerges above the wrist between the ECRL and BR. The PIN passes around the radial head and neck and enters the supinator. The PIN’s branches are to the ECRB, extensor carpi ulnaris, EDC, EDQ, EIP, EPL, extensor pollicis brevis (EPB), and APL. Thumb retropulsion and IP joint extension, MCP joint extension, and wrist extension are the pertinent physical exam tests for radial nerve motor function in the wrist and hand.
The ulnar nerve arises from the medial cord of the brachial plexus and passes from the axillae down the posteromedial aspect of the arm. The nerve courses through the arcade of Struthers in the intermuscular septum of the diaphyseal humerus, passes behind the medial epicondyle of the elbow, and courses through the flexor carpi ulnaris (FCU). The ulnar nerve innervates the FCU and the flexor digitorum profundus (FDP) to the ring and small fingers (FDP IV/FDP V). The ulnar nerve is joined with the ulnar artery in the midportion of the forearm, and they course together through Guyon canal at the wrist to enter the palm. The ulnar nerve branches into the hypothenar motor, ulnar fourth and fifth digit sensory, and deep intrinsic motor branches just beyond the pisiform. Reliable ulnar nerve motor testing is by examining the FDP V (extrinsic) and first dorsal interosseous (intrinsic) muscles.
The median nerve is formed from medial and lateral cord contributions of the brachial plexus. The median nerve courses down the anteromedial upper arm adjacent to the brachial artery. The nerve passes beneath the lacertus fibrosus and then between the two heads of the pronator teres (PT). The anterior interosseous nerve (AIN) motor branch exits posteriorly and eventually innervates the flexor pollicis longus (FPL), FDP to the index finger, and pronator quadratus (PQ). After giving off the PT and AIN, the median nerve courses under the flexor digitorum superficialis (FDS) arch, between the FDP and FDS muscles and tendons in the forearm, and then at the wrist, enters the carpal canal. The palmar cutaneous nerve branch arises from the median nerve, courses on the radial side of the palmaris longus (PL) in the distal forearm and innervates the radial palmar skin. In the carpal canal, the nerve supplies the thenar motor branch for opposition and then exits to provide sensibility to the thumb, index, long, and radial half of the ring finger. Reliable motor testing for the median nerve is performed by examining thumb FPL-IP joint flexion (extrinsic) and opposition (intrinsic).
Surgical Indications
Displaced fractures and dislocations with a neurovascular injury require prompt reduction of the bony displacement. Nerve injuries that do not show signs of recovery by 3 to 6 months postinjury require exploration, decompression, and reconstruction as appropriate. Median and ulnar neuromas in continuity that do not provide functional muscle activity and good sensibility within the first 6 months postinjury require resection and nerve grafting. Chronic radial neuropathies require nerve (first 6 months) or tendon transfers to improve grip and key pinch function. Opposition and FPL/FDP II transfers are appropriate for chronic median neuropathy. Intrinsic transfers and rebalancing are appropriate for chronic ulnar nerve deficiencies.
SURGICAL PROCEDURES
 Observation of Nerve Injuries after Closed Reduction of Fractures and Dislocations
Observation of Nerve Injuries after Closed Reduction of Fractures and Dislocations
In order not to miss an iatrogenic nerve entrapment, laceration, or impairment caused by a closed reduction or pin placement after closed reduction, a complete, precise exam of each nerve prior to reduction and pinning is mandatory. Fortunately, most nerve injuries associated with closed fracture dislocations of the upper limb are not entrapments or lacerations and will resolve over a short time with observation. The usual mechanisms of injury to the nerve are direct trauma (contusion) from the displaced bone at the time of the acute trauma and ongoing traction ischemia while the nerve is tented, kinked, and/or compressed by the unreduced bone. Quickly reducing the fracture and/or dislocation to an anatomic alignment lessens the dysvascular effect on nerve function. Nerve injuries are localized to the traumatic anatomic region and correspond to the direction and degree of bony displacement. In the upper limb, these include, among others:3,4 (see each specific chapter for more detail) (1) axillary nerve with shoulder dislocations;5,6 (2) brachial plexus and axillary nerve with proximal humeral fractures;7,8 (3) radial nerve with humeral shaft fractures;9–11 (4) median, ulnar, and radial nerves and combinations thereof with supracon-dylar humerus fractures;12–16 (5) median and ulnar nerves with elbow dislocations;17–20 (6) radial PIN with anterior Monteggia fracture dislocations;21–25 (7) median and ulnar nerves with diaphyseal forearm fractures;26–28 and (8) median nerve with distal radial physeal fractures.29,30 All of these specific nerve injuries tend to recover as the bone(s) and soft tissues heal.
The nerve recovery can be in days for minor neurapraxia injuries and weeks for more significant neurapraxia or axonotmesis injuries. Signs of a recovering nerve will be (1) an advancing Tinel sign along the anatomic path of the nerve after a brief (up to 30 days) hiatus, (2) initial hypesthesia followed by dysesthesia and then recovering sensibility in the anatomic nerve distribution, and (3) progressive proximal to distal anatomic motor recovery. The nerve recovery pattern, as outlined, needs to begin by 3 to at the latest 6 months after injury. If the nerve does not at least start significant recovery during that time, nerve exploration is warranted. On average, 95% to 98% of the nerve injuries in the upper limb associated with blunt trauma will recover fully with bone and joint treatment and close observation of neural recovery.
 Open Reduction and Nerve Decompression
Open Reduction and Nerve Decompression
Ability may get you to the top, but it takes character to keep you there.
—John Wooden
If a nerve is out preoperatively, and an open reduction of the fracture and/or dislocation is indicated, nerve exploration and decompression is a safe and effective way to resolve entrapped nerves, repair lacerated nerves, and be certain an impaired nerve is not further injured by operative treatment of the displaced bone (see Figures 27-2 and 27-19). Open fractures have a higher incidence of lacerated or incarcerated nerves than closed fractures. The majority of entrapped acute peripheral neuropathies with skeletal trauma only need an acute decompression to fully recover. Since most nerve injuries are geographic to the bone and joint injury extending the incision to decompress, mobilize, and protect the injured nerve(s) with operative fixation is appropriate. A tension-free nerve will recover quicker and be less likely to be further injured by retraction during operative reduction and stabilization. Also, be certain at the end of the case that the nerve(s) is not kinked, compressed, and/or entrapped in the bone or joint or by a pin or plate. Of note, it is our practice to visualize, decompress, mobilize, and protect all nerves in the anatomic region of operative fixation. We also fret about and protect nerves on the contralateral side of the bone we are fixing so as to avoid compression, traction, or penetration injury from a retractor, pin, and/ or screw.
 Management of Acute Hemorrhage
Management of Acute Hemorrhage
Penetrating trauma, most commonly glass or knife lacerations, can injure both blood vessels and nerves. Open fractures can do the same from the inside out. Complete lacerations of arteries will usually bleed dramatically for a short time and then tamponade with pressure and vasospasm. Side-hole arterial and venous lacerations, and major arterial and venous lacerations above the hand, can continue to bleed, sometimes to the extent of life- threatening hemorrhage. The marked hemorrhage lacerations that do not respond to pressure are operative emergencies. A brief tourniquet to control the bleeding may be required between the emergency room and the operative suite, similar to in-field military transport tourniquet indications. Rapid sequence general anesthesia may be necessary. Pressure is maintained over the laceration until sterile conditions and tourniquet control are established. The open wound is extended proximally and distally Unessential bleeding vessels are ligated with sutures and/or vascular clips. Essential arteries or veins are repaired with appropriate magnification and suture size. Contaminated wounds are extensively debrided. Open fractures are thoroughly cleansed and treated with external fixation, closed or open reduction depending on the situation. Associated nerve and tendon injuries are repaired primarily or in a delayed fashion as is best for outcome.
 Microscopic Nerve Repairs (See Sidebar)
Microscopic Nerve Repairs (See Sidebar)
Glass and knife lacerations are the most common causes of traumatic nerve injuries in children and adolescents. Many of these penetrating injuries are associated with vascular and/or muscle-tendon unit lacerations. Thin shards of glass are very sharp and can penetrate deeply through a minor skin laceration. So too can long, thin knife blades. The relatively benign appearance of the skin laceration will fool the emergency caregiver into believing there are no deep lacerations. Without extension of the minor skin laceration, the deeper lacerated structures will not be visible. (Remember, cut tendons, nerves, and blood vessels move away from the laceration site with changes in digital and wrist position.) A tendon- and nerve-specific clinical exam is necessary for each anatomic structure in the region of the laceration in order to make an accurate diagnosis and provide timely treatment. The children and teenagers just will not tell you, “Hey Doc, my nerve and tendon have been cut.” And as with many bad things in these young children’s lives, their parents may not find out until much later.
Surgical Magnification and Microsurgical Instruments
All hand surgeons must have a pair of loupes. Surgical magnification loupes are manufactured by several companies and are of varying magnification size (2.5×, 3.5×, and 4.5× are the most common choices), depth of field (normal or expanded), optical working distance (usually 15 to 20″ for hand surgery), cost, and eye frame or head support options. The lower magnification loupes (2.5×) are less stressful to the surgeon’s neck over the course of a long case or career. The higher magnification loupes, especially with expanded field, allow for more precise surgical care. For many pediatric hand surgery cases, higher magnification expanded field view is preferred. Some nerve and vascular surgery cases, especially bigger nerves and vessels located in difficult places to position a microscope, can be done safely with 4.5× expanded field magnification.
However, most microsurgery cases should truly be performed with the aid of the microscope. Two-headed microscopes are important to actively involve a skilled assist in these complex cases. A three-headed microscope can help educate an additional microsurgical trainee. A fiber optic video connection to an operating room monitor keeps the entire team (surgical scrub, circulator, anesthesia, and trainees) engaged. Learning all the ins and outs of the microscope in your operating room is important for your surgical success. Not all of these cases occur in the light of day when all the knowledgeable help is around to set up and fix any equipment problems.
The saying, “A carpenter is only as good as his tools,” does apply to some degree to microsurgery. Precise handling of tissue is imperative to successful outcome. Well-maintained microscopic smooth-tipped forceps; straight, curved, and serrated scissors; straight and curved needle holders; atraumatic clamps, all of various sizes and without burrs or other defects, are critical to microsurgery techniques. A ready supply of 8-0, 9-0, 10-0, and even 11-0 nylon microsutures is necessary for pediatric microsurgery. The usual needle curve is in 75- to 100-μm range. Remember, hand surgery–preferred needles will be different in needle tip (blunt, sharp, tapered, cutting) and curvature than other subspecialty microscopic needles. Beware that you may be handed an ophthalmological 9-0 needle that could sabotage your repair techniques. Without being difficult, you have to be exacting regarding the equipment you need to do this type of surgery.
 Digital Nerve and Peripheral Sensory Nerve Lacerations
Digital Nerve and Peripheral Sensory Nerve Lacerations
Sharp digital nerve lacerations that are diagnosed and treated within 3 weeks of injury have an outstanding chance of full sensibility recovery in the pediatric and adolescent age group. Lacerations diagnosed later can even go on to full recovery (Figure 37-2), but some may require a segmental nerve graft to have a tension-free repair. Since these patients do so well in terms of sensibility recovery, and since neuromas can be painful and functionally limiting, we repair or reconstruct all digital nerve lacerations regardless of when they present to us. This is especially true of the ulnar side of the thumb; radial side of the index finger; and ulnar side of the small finger, as these are important areas for functional sensibility.
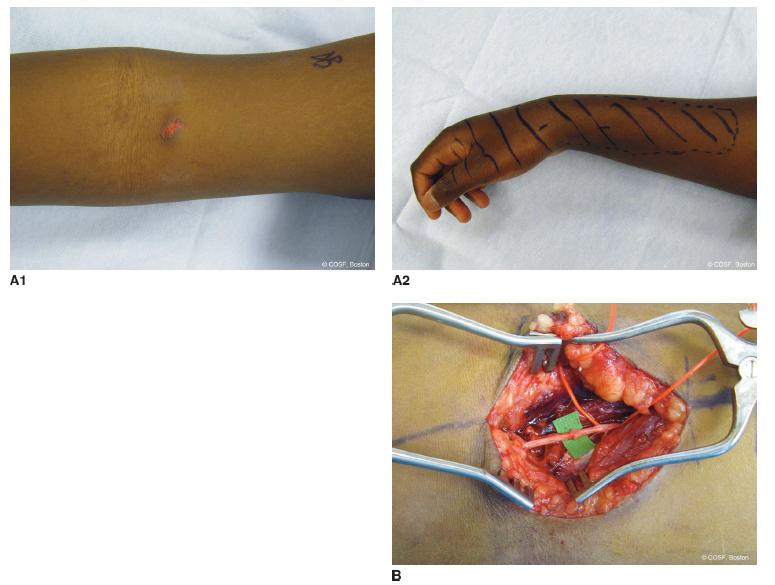
FIGURE 37-2 A1: Late-presenting laceration of the upper arm with symptomatic numbness and dysesthesia on clinical exam noted by shaded area (A2). B: Microscopic repair of lateral antebrachial cutaneous nerve.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


