Trauma to the Nervous System
Magdi M. Sobeih
The statement that children are not small adults particularly applies when considering the developing nervous system. The nervous system is constantly changing throughout childhood. Thus the way trauma to the developing nervous system affects the child depends on where along the neuraxis the trauma occurs, at what age and developmental stage, and the mechanism of the trauma. These specifics are important to consider in the context of the most frequent causes of trauma, the implications, and the outcomes. Trauma usually results in acute deterioration in neurologic function but late sequelae or delayed effects must also be anticipated. In this section, discussion will focus on the most commonly encountered scenarios of trauma to the nervous system in pediatrics. This includes accidental traumatic brain injury, inflicted neurotrauma, spinal cord injury, and associated injury to adjacent tissues, such as bone in skull fractures and blood vessels in hemorrhage. The acute management of these injuries is further discussed in Chapter 104. Trauma to the brachial plexus during delivery will be briefly discussed.
CRANIOCEREBRAL TRAUMA
Under normal circumstances, the skull protects the brain from minor trauma by cushioning the sensitive contents from external blows. The surrounding cerebrospinal fluid (CSF) assists in reducing any force by providing a fluid layer in which the brain may “float.” However, with more severe trauma, the differential rate of movement of the skull, brain, CSF, and blood vessels causes acute injury to the contents. Traumatic brain injury results from the sudden acceleration or deceleration of the brain relative to the skull or from penetrating injury. The degree of injury manifests along a spectrum from mild functional impairment without obvious visible injury (either on physical examination or neuroimaging) to severe, generalized, or focal/multifocal injury.
Head injury is one of the most common neurologic disorders in pediatrics. Millions of children and adolescents suffer an injury to the head each year but most do not seek medical attention or are seen by a primary physician well after the event. Thus, the incidence and characteristics of these head injuries are not fully known. Of those who seek care in a hospital-based setting, each year, approximately 475,000 traumatic brain injuries (TBIs) occur in children ages 0 to 14 years.1 More than 90% of these (435,000) present to emergency rooms for immediate care, 37,000 are hospitalized, and 2685 are fatal. The rate of TBI-related emergency room (ER) visits, hospitalizations and deaths is greater than 50% more common in boys than girls ages 0 to 14. Across all ages in children and adolescents, TBI is more common in males than in females. Falls are the most common cause of TBI from ages 0 to 14, accounting for 39% of all TBIs in that age range. After age 14, motor vehicle accidents become the most common cause, followed by assaults and falls. Most fall-related TBIs are evaluated in the emergency room and more than 90% of patients are released to their home. However, after age 4 years, motor vehicle accidents (usually as passenger but also as pedestrian or pedal-powered operator) increasingly account for TBI-related hospitalizations and deaths. These statistics have several implications for mechanisms and severity of injury, and prevention of TBI (discussed below).
MILD TRAUMATIC BRAIN INJURY
It is clear from the statistics that the most common form of pediatric head injury results in mild traumatic brain injury (mTBI).2 Also known as concussion, minor head injury, minor head trauma, or minor TBI, mTBI had been diagnosed based on scores of 13 to 15 on the Glasgow Coma Scale. However, most recently, mTBI has been defined clinically by the brief presence of altered mental status after injury from impact or forceful linear or rotational motion of the head with or without loss of consciousness.3,4 This alteration in mental status is characterized by confusion or disorientation, trauma induced retrograde and/or anterograde amnesia, or loss of consciousness less than 30 minutes. By contrast, moderate or severe TBIs are associated with loss of consciousness longer than 30 minutes, amnesia longer than 24 hours, penetrating skull injury, or visible signs of focal/multifocal brain injury on physical examination or neuroimaging (see below).
 PATHOPHYSIOLOGY
PATHOPHYSIOLOGY
Neurologic sequelae of mild traumatic brain injury (mTBI) are not the result of localization-related injury but of widespread neuronal metabolic dysfunction involving a cascade of subcellular ionic, metabolic, and local physiologic events. These involve neuronal depolarization with release of excitatory neurotransmitters, potassium release from the intracellular compartment, increased energy utilization by ion pumps to restore homeostasis, leading to increased glycolysis and lactate accumulation. This leads to changes in cerebral blood flow and axonal function (Fig. 551-1). During brain development, the excitatory neurotransmitter glutamate predominates, meaning there is an increased probability of excitotoxicity in the developing brain. The widespread activation of glutamate receptors also results in downregulation of the receptors and changes in inhibitory circuitry with increased the chance for seizures.5
 CLINICAL FEATURES AND ASSOCIATED INJURIES
CLINICAL FEATURES AND ASSOCIATED INJURIES
Clinically, mild traumatic brain injury (mTBI) manifests as disruption of one or more of four domains: physical, cognitive, emotional, and sleep patterns. Acutely, children suffering mTBI may experience symptoms of vomiting, headache, emotional lability or inconsolability, restlessness, irritability, mental confusion, amnesia, dizziness, transient loss of vision (often confused with malingering), seizure, or change in personality. Physical signs are often lacking but should be considered as with any trauma-related injury. This includes monitoring of airway, breathing, and circulation. Further management depends on recovery of function and persistence of symptoms. Thus, immediate evaluation on site should document level of functioning after injury such as assessment of retrograde and anterograde amnesia and loss of consciousness. In school age children, mTBI often occurs in sports-related activities so that assessment on the field may be made by coaches or certified athletic trainers using standardized instruments such as the Standardized Assessment of Concussion. When a child is seen by a clinician, the Acute Concussion Evaluation (ACE) form available from the CDC4 helps to document and subsequently track symptoms thus assisting in planning recovery management. In preschool or pre-verbal children, clinicians must have a low threshold of suspicion for concussion after head injury because these individuals will not be able to report symptoms, even though they may have headache, crying, irritability, restlessness, dizziness, confusion, seizure, or change in personality. Emergency room evaluation is warranted if these symptoms worsen in a pre-verbal child.
 DIAGNOSTIC EVALUATION
DIAGNOSTIC EVALUATION
Medical evaluation of any child with mild traumatic brain injury (mTBI) first documents the nature or cause and circumstances of the injury including type and strength of force and location on the head and position of the head at the time of impact. A greater force causing the injury correlates with greater potential for more severe symptoms. However, when the history suggests the symptoms are out of proportion to the force of the injury, malingering should not be assumed but increased susceptibility to mTBI (especially if there is a history of multiple mTBI) or other physical or psychological factors should be considered. Whiplash type injury occurs when a blow to the body or to a vehicle results in acceleration and deceleration forces on the brain, leading to coup and contrecoup injuries. Physical examination should first assess airway, breathing, and circulation. It is important to rule out any bleeding including hematoma or petechiae. Neuroimaging is not necessary in most cases of mTBI, particularly in children older than age 2 years. However, if there is a history of loss of consciousness longer than a few seconds, or deteriorating neurologic function, worsening of initial symptoms, or new symptoms, imaging should be considered. Head computed tomography (CT) is optimal for detecting skull fracture and intracranial blood; it is also ideal for rapid assessment and detection of brain edema.
Neuropsychologic testing using standardized tests establishes quantifiable measures of self-reported or observed impairments in the cognitive domain. This testing can be repeated over the subsequent 6 to 12 months in order to guide recommendations for return to full activity after mTBI.
 COMPLICATIONS
COMPLICATIONS
After the initial symptoms of mild traumatic brain injury (mTBI), a child may continue to complain of headache, dizziness, and cognitive impairment, and exhibit behavioral disorders such as irritability for days, weeks, and even months. These symptoms constitute postconcussive syndrome and are treated symptomatically.
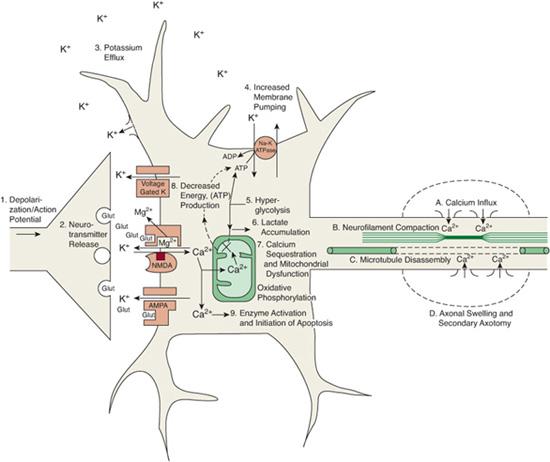
FIGURE 551-1. Neurometabolic cascade following traumatic injury. (1) Nonspecific depolarization and initiation of action potentials. (2) Release of excitatory neurotransmitters (EAAs). (3) Massive efflux of potassium. (4) Increased activity of membrane ionic pumps to restore homeostasis. (5) Hyperglycolysis to generate more adenosine triphosphate (ATP). (6) Lactate accumulation. (7) Calcium influx and sequestration in mitochondria leading to impaired oxidative metabolism. (8) Decreased energy (ATP) production. (9) Calpain activation and initiation of apoptosis. (A) Axolemmal disruption and calcium influx. (B) Neurofilament compaction via phosphorylation or sidearm cleavage. (C) Microtubule disassembly and accumulation of axonally transported organelles. (D) Axonal swelling and eventual axotomy. K+, potassium; Na+, sodium; Glut, glutamate; Mg2+, magnesium; Ca2+, calcium; NMDA, N-methyl-D-aspartate; AMPA, d-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid. (Source: Giza CC, Hovda DA: The neurometabolic cascade of concussion. J Athl Train. 2001; 36(3):228-235. Copyright © by the National Athletic Trainers’ Association, Inc.)
 TREATMENT AND MANAGEMENT
TREATMENT AND MANAGEMENT
Most likely due to the general neuronal metabolic and physiologic dysfunction, during recovery from mTBI, symptoms may worsen or reemerge with physical or mental exertion. Thus treatment is symptomatic and preventive. Immediately after a concussion, rest is essential. There should be no physical exertion until there are no signs or symptoms of mTBI at rest. The decision to return to full activity should be guided and planned. Return to full activity should be gradual and graded as, for example, those involved in sports. The recommended return to sport guidelines6,7 include (1) complete rest, especially on the day of injury (thus removal from the competition); (2) light aerobic exercise, such as walking, without weight training; (3) sport-specific activity such as running with some weight lifting; (4) training drills without contact; (5) training drills with full contact; and (6) competitive game play. At each of these steps, physical and mental monitoring and comparison with initial Acute Concussion Evaluation status should guide ongoing and increasing level of activity.
Minimal TBI affects cognitive abilities and experience-dependent learning. For this reason, the child’s academic performance should be monitored and return to full academic participation should be gradual. Initially after concussion, lighter school and homework loads should be considered. If necessary, more formal Section 504 plans (designed to accommodate the unique needs of an individual with a disability) or Individualized Education Plans should be instituted.
Second Impact Syndrome
The risk of returning to full activity after mTBI is the possibility of further mTBI with resultant worsening of postconcussive symptoms. With the impairment in cognitive ability and reaction time after an initial mTBI, the risk of repeat injury is higher than baseline. A more dangerous, albeit less common occurrence with repeated mTBI, is second impact syndrome. If full recovery from the first impact has not occurred and cerebrovascular autoregulation is still impaired, a second episode of head trauma may trigger diffuse cerebral edema secondary to hyperemia, vasogenic edema, or cytotoxic edema. This may lead to increased intracranial pressure and brain herniation. Unrecognized after minor head trauma and untreated, this can be fatal.
 PROGNOSIS AND PREVENTION
PROGNOSIS AND PREVENTION
Most children recover completely after mTBI and do not have lasting postconcussive symptoms. Treatment of any effects of concussion should be symptomatic with rest, over-the-counter analgesics for headaches and medication for attention deficit symptoms or other behavioral problems. Effects of mTBI may be slightly worse for the younger child. For example, some evidence suggests longer times to recover from the cognitive deficits after concussions in high school athletes compared with college athletes.
Because the mechanisms of mTBI involve direct force on the brain, measures to avoid or dissipate potential forces on the head decrease the likelihood of mTBI. This involves the use of appropriate car seats and seatbelts in motor vehicles to decrease the chance of whiplash injuries, and the use of helmets during sporting and physical activities such as bicycle and scooter riding or winter snow and ice activities. For parents of toddlers, anticipatory guidance against use of walkers is warranted.
TRAUMATIC BRAIN INJURY (MODERATE TO SEVERE)
Clinically, moderate traumatic brain injury (TBI) has been classified based on Glasgow Coma Scale (GCS) score of 9 to 12 and severe TBIs with scores less than 8. These somewhat artificial distinctions are meant to reflect severity of injuries causing unconsciousness longer than 30 minutes, amnesia longer than 24 hours, or penetrating skull injuries. In pediatric patients with severe TBI, lower GCS scores correlate with worse outcome. There may also be associated intracranial injuries based on neuroimaging. These may include skull fractures, brain contusions, and intracranial hemorrhages (see below).
 BIOMECHANICS AND PATHOPHYSIOLOGY
BIOMECHANICS AND PATHOPHYSIOLOGY
With child development, muscles strengthen, skull thickness and tensile strength increase, and the motor repertoire expands and becomes more adept. The mechanisms of injury and implications of accidental injury change with the age of the child. Infants tend to suffer accidental injury most frequently due to low-level falls (ie, less than 3–4 feet), for example from cribs and beds. Skull thickness increases with age from 1 mm in infants to 4 mm in a young child and 10 mm in adults.8 With impact injury, the skull of an infant is more likely to fracture compared with that of an adult, particularly in the thinnest part of the calvarium—the parietal region. The infant skull is able to deform and absorb a significant amount of the energy of the fall thus protecting the brain from more severe injury. Much more energy is required to cause intracranial injury (ie, bleeding) and axonal damage in the infant and young child compared with the adult. Still, intracranial injury may occur (see below) even without any clinical signs and symptoms. As the child begins to ambulate, falls from heights, such as off furniture or down stairs, become more common.
The neurometabolic cascade discussed above also operates after a more forceful head injury. Additionally, diffuse axonal injury from shear forces, disconnection, and necrotic and apoptotic cell death may occur. The resultant effects on the developing brain have delayed and lasting implications for prognosis and outcome (see below). Other than the initial TBI, second insults such as hypoxia and hypotension exacerbate brain injury and are associated with poorer outcome. Diffuse cerebral edema, which may lead to decreased cerebral perfusion, is more common in infants and children compared with adults, after severe TBI.9
 DIAGNOSTIC EVALUATION
DIAGNOSTIC EVALUATION
After stabilizing and securing the airway, breathing, and circulation, the diagnostic evaluation of a child with moderate to severe TBI begins with physical examination for associated injuries and neurologic examination followed by neuroimaging. In infants in whom specific symptoms are difficult to elicit early, imaging of the cranium for signs of skull fracture must be included. Underlying intracranial bleeding is quickest and best seen using computed tomography (CT scanning). If magnetic resonance imaging (MRI) is available, sequences to detect blood can be used. An advantage of MRI is the ability to detect signs of brain edema early and without exposure to radiation. Also, any child with a change in level of consciousness or focal neurologic deficit on examination should undergo neuroimaging using brain MRI.
 TREATMENT
TREATMENT
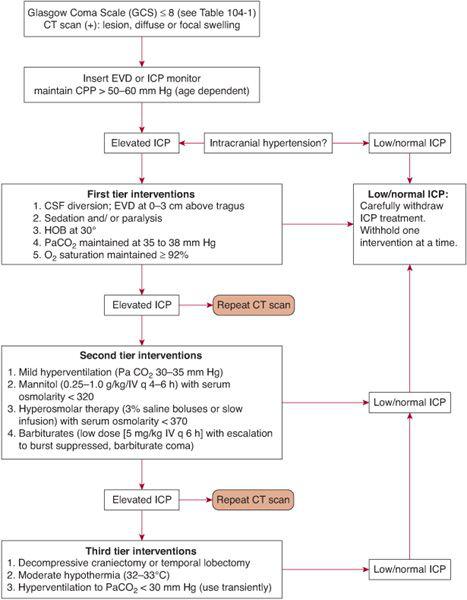
Hospital-based treatment of acute moderate to severe TBI in children aims to reduce the likelihood of second insult and maintain adequate cerebral perfusion pressure and tissue oxygenation. Thus, management of airway, breathing, and circulation is paramount, as is decreasing brain edema to guard against increased intracranial pressure. There is no clear treatment standard but algorithms for tiered management of acute TBI exist (Fig. 551-2).10 Strategies including prophylactic use of antiepileptics and antipyretics are instituted to decrease metabolic demand of the brain and possible second insult. Hypothermia therapy is another means of reducing the metabolic demands of the brain. Observations of improved survival and recovery after cold water drowning have led to trials of therapeutic brain cooling after TBI. However, speed of initiation of hypothermia, degree of cooling, length of cooling time, and rapidity of rewarming have yet to be established. The most recent multicenter trial of hypothermia for pediatric TBI initiated within 8 hours and lasting for 24 hours failed to show any improvement in either neurologic outcome or survival benefit.11 Further large-scale trials to establish standards for hypothermia in pediatric TBI are needed.
 PROGNOSIS AND OUTCOME
PROGNOSIS AND OUTCOME
Children who suffer focal brain lesions often show remarkable neurologic recovery because of developmental plasticity. In fact, the earlier in development a lesion is acquired, the better the neurologic outcome will be. However, this same capacity for plasticity and reorganization may belie a propensity for worse outcome after the more global insult of TBI in children compared with adults. Because a majority of cognitive and adaptive behavior neural systems continue to develop throughout childhood to young adulthood, injury to these frontal, subcortical, distributed systems leads to significant developmental and cognitive delay and behavioral impairment. In one study12 children who suffered accidental TBI prior to age 2 on average performed at least one standard deviation below the mean on standardized cognitive developmental testing at age 3. Those with nonaccidental TBI fared worse (see below). Posttraumatic headaches and seizures may also occur. Seizures occurring within 7 days of injury are termed acute and are the result of immediate effects of the injury such as glutamate release, stretch induced neuronal depolarization, and local irritation from blood products. Late seizures (occurring after 7 days postinjury) may be secondary to infection, neuronal death, gliosis, and aberrant neuronal circuit development.
The same physical protective measures described for mild traumatic brain injury (mTBI) (vehicle safety and helmet use) apply for more serious TBI.
INFLICTED CHILDHOOD NEUROTRAUMA
Physical abuse of children by adults results in many types of injury (see also Chapter 35). The most severe and fatal injuries affect the nervous system, especially the brain and cervical spinal cord. Over the past few decades, various terminologies have been used to describe the method of injury including battered child syndrome, shaken baby syndrome, shaken impact syndrome, trauma X, nonaccidental trauma, inflicted TBI, and inflicted childhood neurotrauma. An adult or older child may inflict injury on an infant or younger child by shaking, hitting, throwing down onto the floor or against a wall, or asphyxiation in attempts to quiet by smothering or strangulating. Each of these mechanisms causes significant and multifocal injuries to the child’s neuraxis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


